Search
- Page Path
- HOME > Search
- Endodontic micro-resurgery and guided tissue regeneration of a periapical cyst associated to recurrent root perforation: a case report
- Fernando Córdova-Malca, Hernán Coaguila-Llerena, Lucía Garré-Arnillas, Jorge Rayo-Iparraguirre, Gisele Faria
- Restor Dent Endod 2022;47(4):e35. Published online September 3, 2022
- DOI: https://doi.org/10.5395/rde.2022.47.e35
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
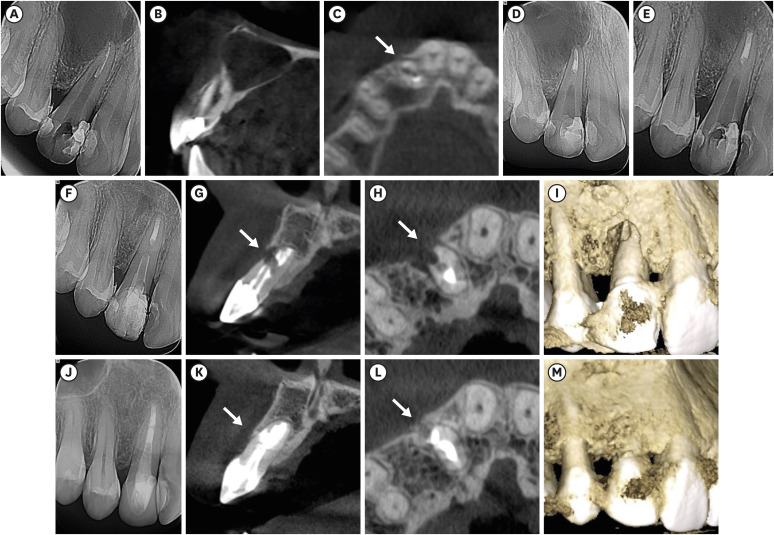
ePub Although the success rates of microsurgery and micro-resurgery are very high, the influence of a recurrent perforation combined with radicular cyst remains unclear. A 21-year-old white female patient had a history of root perforation in a previously treated right maxillary lateral incisor. Analysis using cone-beam computed tomography (CBCT) revealed an extensive and well-defined periapical radiolucency, involving the buccal and palatal bone plate. The perforation was sealed with bioceramic material (Biodentine) in the pre-surgical phase. In the surgical phase, guided tissue regeneration (GTR) was performed by combining xenograft (lyophilized bovine bone) and autologous platelet-rich fibrin applied to the bone defect. The root-end preparation was done using an ultrasonic tip. The retrograde filling was performed using a bioceramic material (Biodentine). Histopathological analysis confirmed a radicular cyst. The patient returned to her referring practitioner to continue the restorative procedures. CBCT analysis after 1-year recall revealed another perforation in the same place as the first intervention, ultimately treated by micro-resurgery using the same protocol with GTR, and a bioceramic material (MTA Angelus). The 2-year recall showed healing and bone neoformation. In conclusion, endodontic micro-resurgery with GTR showed long-term favorable results when a radicular cyst and a recurrent perforation compromised the success.
-
Citations
Citations to this article as recorded by- Outcome of endodontic micro-resurgery: A systematic review
Faisal Alnassar, Riyadh Alroomy, Qamar Hashem, Abdullah Alqedairi, Nabeel Almotairy
Saudi Endodontic Journal.2025; 15(2): 112. CrossRef - Platelet-Rich Plasma and Platelet-Rich Fibrin in Endodontics: A Scoping Review
Simão Rebimbas Guerreiro, Carlos Miguel Marto, Anabela Paula, Joana Rita de Azevedo Pereira, Eunice Carrilho, Manuel Marques-Ferreira, Siri Vicente Paulo
International Journal of Molecular Sciences.2025; 26(12): 5479. CrossRef - Non-surgical Approach to a Maxillary Cyst-Like Lesion: Orthograde Endodontic Treatment With Neodymium-Doped Yttrium Aluminum Garnet (Nd:YAG) Decontamination of the Canal System
Beatrice Spaggiari, Paolo Vescovi, Silvia Pizzi, Roberta Iaria, Ilaria Giovannacci
Cureus.2025;[Epub] CrossRef - Persistent Periradicular Lesion Associated With Concurrent Root Fracture and Odontogenic Keratocyst: A Case Report
Mehdi Vatanpour, Fatemeh Rezaei
Clinical Case Reports.2025;[Epub] CrossRef - Management of Apico-marginal Defects With Endodontic Microsurgery and Guided Tissue Regeneration: A Report of Thirteen Cases
Abayomi O. Baruwa, Jorge N.R. Martins, Mariana D. Pires, Beatriz Pereira, Pedro May Cruz, António Ginjeira
Journal of Endodontics.2023; 49(9): 1207. CrossRef
- Outcome of endodontic micro-resurgery: A systematic review
- 2,701 View
- 53 Download
- 4 Web of Science
- 5 Crossref

- Leukocyte platelet-rich fibrin in endodontic microsurgery: a report of 2 cases
- Mariana Domingos Pires, Jorge N. R. Martins, Abayomi Omokeji Baruwa, Beatriz Pereira, António Ginjeira
- Restor Dent Endod 2022;47(2):e17. Published online March 4, 2022
- DOI: https://doi.org/10.5395/rde.2022.47.e17
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
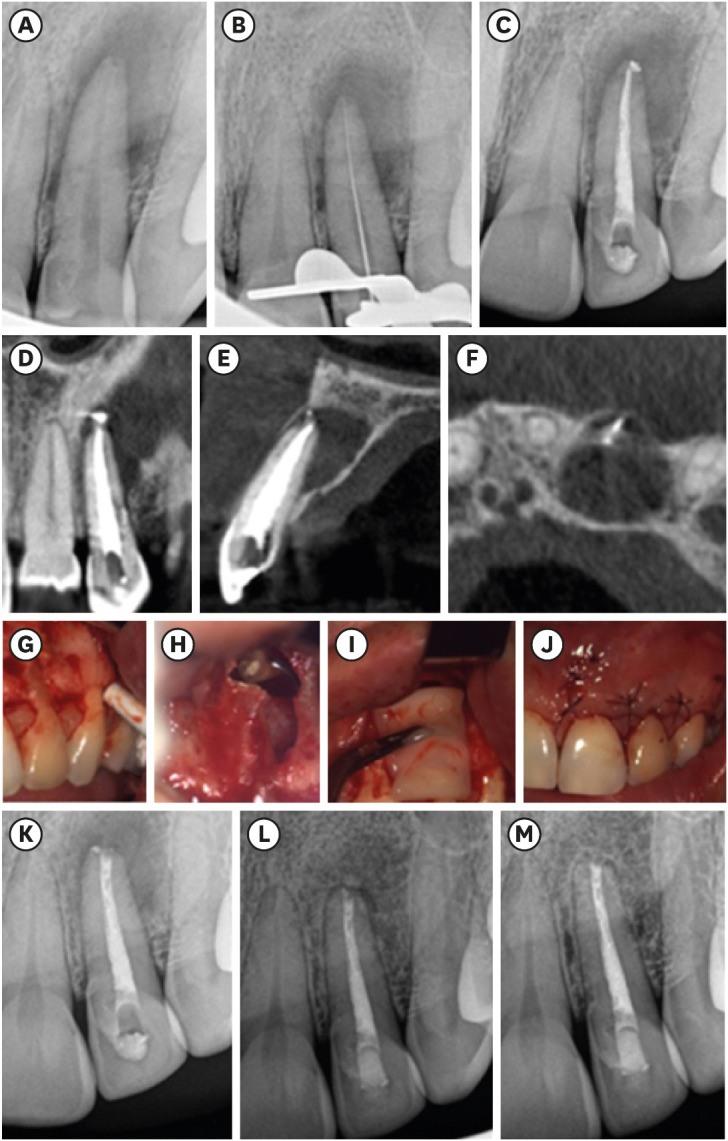
ePub Endodontic microsurgery is a predictable treatment option when orthograde treatment or retreatment is unsuccessful or unfeasible. However, when there is a gross compromise of periapical bone, achievement of bone regeneration after the surgical procedure may be hampered. In such cases, the application of guided tissue regeneration principles, with adjunctive use of leukocyte platelet-rich fibrin to fill the bone defect as a bone substitute and as a membrane to cover the site, provides a cost-effective solution with the benefits of accelerated physiological healing and reduced post-surgical pain and discomfort. This case report presents 2 cases of endodontic microsurgery of the upper lateral incisors with loss of buccal cortical plate, where platelet-rich fibrin was successfully applied.
-
Citations
Citations to this article as recorded by- Focuses and Trends of Research on Platelet-Rich Fibrin: A Bibliometric and Visual Analysis
Ying Zhao, Chen Dong, Liumeizi Fan, Ting Lei, Xin Ge, Zhou Yu, Sheng Hu
Indian Journal of Plastic Surgery.2024; 57(05): 356. CrossRef
- Focuses and Trends of Research on Platelet-Rich Fibrin: A Bibliometric and Visual Analysis
- 1,559 View
- 30 Download
- 1 Web of Science
- 1 Crossref

- Management of apicomarginal defect in esthetic region associated with a tooth with anomalies
- Vinayak Venkoosa Meharwade, Dipali Yogesh Shah, Pradyna Prabhakar Mali, Vidya Vinayak Meharwade
- Restor Dent Endod 2015;40(4):314-321. Published online June 24, 2015
- DOI: https://doi.org/10.5395/rde.2015.40.4.314
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Tooth related factors such as palatoradicular groove can be one of the causes for localized periodontal destruction. Such pathological process may result in apicomarginal defect along with inflammation of pulp. This creates challenging situation which clinician must be capable of performing advanced periodontal regenerative procedures for the successful management. This case report discusses clinical management of apicomarginal defect associated with extensive periradicular destruction in a maxillary lateral incisor, along with histopathologic aspect of the lesion.
-
Citations
Citations to this article as recorded by- Surgical treatment of apico-marginal defect associated with maxillary incisor teeth with a large periapical lesion using sticky bone & platelet rich fibrin membrane – A case report
Snigdho Das, Parthasarathi Mondal, Dipanjan Das, Kurchi Mandal, Kallol Kumar Saha
IP Annals of Prosthodontics and Restorative Dentistry.2024; 10(3): 250. CrossRef - Comparative evaluation of sticky bone with guided tissue regeneration and platelet-rich fibrin membranes in healing of apicomarginal defects with periapical pathology: An in-vivo study
D. Das, P. Mondal, K. K. Saha, S. Das, D. Karmakar, A. Bhagawati
Endodontics Today.2024; 22(4): 335. CrossRef
- Surgical treatment of apico-marginal defect associated with maxillary incisor teeth with a large periapical lesion using sticky bone & platelet rich fibrin membrane – A case report
- 1,265 View
- 5 Download
- 2 Crossref


 KACD
KACD

 First
First Prev
Prev


