Search
- Page Path
- HOME > Search
-
Incorporation of amoxicillin-loaded microspheres in mineral trioxide aggregate cement: an
in vitro study - Fábio Rocha Bohns, Vicente Castelo Branco Leitune, Isadora Martini Garcia, Bruna Genari, Nélio Bairros Dornelles, Silvia Stanisçuaski Guterres, Fabrício Aulo Ogliari, Mary Anne Sampaio de Melo, Fabrício Mezzomo Collares
- Restor Dent Endod 2020;45(4):e50. Published online October 7, 2020
- DOI: https://doi.org/10.5395/rde.2020.45.e50
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
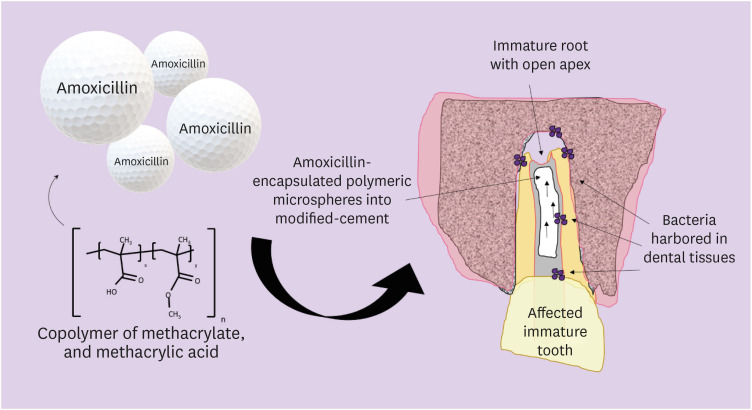
ePub Objectives In this study, we investigated the potential of amoxicillin-loaded polymeric microspheres to be delivered to tooth root infection sites via a bioactive reparative cement.
Materials and Methods Amoxicillin-loaded microspheres were synthesized by a spray-dray method and incorporated at 2.5% and 5% into a mineral trioxide aggregate cement clinically used to induce a mineralized barrier at the root tip of young permanent teeth with incomplete root development and necrotic pulp. The formulations were modified in liquid:powder ratios and in composition by the microspheres. The optimized formulations were evaluated
in vitro for physical and mechanical eligibility. The morphology of microspheres was observed under scanning electron microscopy.Results The optimized cement formulation containing microspheres at 5% exhibited a delayed-release response and maintained its fundamental functional properties. When mixed with amoxicillin-loaded microspheres, the setting times of both test materials significantly increased. The diametral tensile strength of cement containing microspheres at 5% was similar to control. However, phytic acid had no effect on this outcome (
p > 0.05). When mixed with modified liquid:powder ratio, the setting time was significantly longer than that original liquid:powder ratio (p < 0.05).Conclusions Lack of optimal concentrations of antibiotics at anatomical sites of the dental tissues is a hallmark of recurrent endodontic infections. Therefore, targeting the controlled release of broad-spectrum antibiotics may improve the therapeutic outcomes of current treatments. Overall, these results indicate that the carry of amoxicillin by microspheres could provide an alternative strategy for the local delivery of antibiotics for the management of tooth infections.
-
Citations
Citations to this article as recorded by- Local drug delivery for regeneration and disinfection in endodontics: A narrative review
Anu Elsa Swaroop, Sylvia Mathew, P. Harshini, Shruthi Nagaraja
Journal of Conservative Dentistry and Endodontics.2025; 28(2): 119. CrossRef - Modified Mineral Trioxide Aggregate—A Versatile Dental Material: An Insight on Applications and Newer Advancements
C. Pushpalatha, Vismaya Dhareshwar, S. V. Sowmya, Dominic Augustine, Thilla Sekar Vinothkumar, Apathsakayan Renugalakshmi, Amal Shaiban, Ateet Kakti, Shilpa H. Bhandi, Alok Dubey, Amulya V. Rai, Shankargouda Patil
Frontiers in Bioengineering and Biotechnology.2022;[Epub] CrossRef - Local Drug Delivery Systems for Vital Pulp Therapy: A New Hope
Ardavan Parhizkar, Saeed Asgary, Carlo Galli
International Journal of Biomaterials.2021; 2021: 1. CrossRef
- Local drug delivery for regeneration and disinfection in endodontics: A narrative review
- 1,876 View
- 13 Download
- 3 Crossref

- Treatment of non-vital immature teeth with amoxicillin-containing triple antibiotic paste resulting in apexification
- Hyon-Beom Park, Bin-Na Lee, Yun-Chan Hwang, In-Nam Hwang, Won-Mann Oh, Hoon-Sang Chang
- Restor Dent Endod 2015;40(4):322-327. Published online August 28, 2015
- DOI: https://doi.org/10.5395/rde.2015.40.4.322
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub A recent treatment option for non-vital immature teeth in young patients is revascularization with triple antibiotic paste (TAP). However, tooth discoloration was reported with the use of conventional minocycline-containing TAP. In this case report, amoxicillin-containing TAP was used for revascularization of non-vital immature teeth to prevent tooth discoloration. At the 1 yr follow up, the teeth were asymptomatic on clinical examination and showed slight discoloration of the crown due to mineral trioxide aggregate (MTA) filling rather than amoxicillin-containing TAP. Radiographic examination revealed complete resolution of the periapical radiolucency, and closed apex with obvious periodontal ligament space. However, the root growth was limited, and the treatment outcome was more like apexification rather than revascularization. These results may be due to unstable blood clot formation which could not resist the condensation force of MTA filling, whether or not a collagen matrix was in place. These cases showed that although revascularization was not successful, apexification could be expected, resulting in the resolution of the periapical radiolucency and the closure of the apex. Therefore, it is worthwhile attempting revascularization of non-vital immature teeth in young patients.
-
Citations
Citations to this article as recorded by- Comparative evaluation of effect of modified triple antibiotic paste and calcium hydroxide as intracanal medicament on microhardness of root dentin: An in vitro study
Aparna Palekar, Piyush Mantri, Minal Awinashe, Basawaraj Biradar, Mukund Singh
Endodontology.2024;[Epub] CrossRef - Healing of Large Endodontic Lesions Using Long‐Term Application of a New Combination of Triple Antibiotics: A Series of Cases
Saeed Asgary, Ardavan Parhizkar, Maria Beatriz Duarte Gavião
Case Reports in Dentistry.2023;[Epub] CrossRef - Comparative Evaluation of Two Antibiotic Pastes for Root Canal Disinfection
Sadhna Sharma, Urvashi Bhushan, Mridula Goswami, CP Baveja
International Journal of Clinical Pediatric Dentistry.2022; 15(S1): S12. CrossRef - Regenerative Endodontics as the Future Treatment of Immature Permanent Teeth
Justyna Zbańska, Katarzyna Herman, Piotr Kuropka, Maciej Dobrzyński
Applied Sciences.2021; 11(13): 6211. CrossRef - Antimicrobial efficacy of triple antibiotic paste in teeth with primary endodontic infection: A systematic review
Rhythm Bains, Aseem P. Tikku, Promila Verma, Pragya Pandey
Asian Journal of Oral Health and Allied Sciences.2021; 11: 2. CrossRef - Effectiveness of MTA apical plug in dens evaginatus with open apices
Khoa Van Pham, Thu Anh Tran
BMC Oral Health.2021;[Epub] CrossRef - Lesion Sterilization and Tissue Repair: A Literature Review
Ankit Rawat, Jyoti Nagpal, Shreeya Mehta, Divya Vyas, Abhishek Kumar, Fathima Amal
Journal of Research and Advancement in Dentistry.2021; 12(3): 6. CrossRef - Spectrophotometric assessment of Tooth discoloration induced by various Antibiotic pastes
Ravi Gupta, Radhika Kewalramani, Dishant Patel
Research Journal of Pharmacy and Technology.2021; : 1979. CrossRef - Comparative evaluation of calcium release of the apical plugs formed by mineral trioxide aggregate, Biodentine, and EndoSequence root repair material with and without 2% triple antibiotic powder: An in vitro study
PoojaNitin Mapara, ND Shashikiran, Sachin Gugawad, Namrata Gaonkar, Savita Hadakar, Swapnil Taur, Dhanshri Khade
Journal of Indian Society of Pedodontics and Preventive Dentistry.2020; 38(2): 132. CrossRef - Effect of triple antibiotic loaded apatitic nanocarriers on Enterococcus faecalis biofilm – An In vitro study
S. Nagarathinam, V. Sujatha, K. Madhumathi, S. Mahalaxmi, P.Pranav Vanajassun, T.S.Sampath Kumar
Journal of Drug Delivery Science and Technology.2019; 51: 499. CrossRef - Coronal tooth discoloration induced by regenerative endodontic treatment using different scaffolds and intracanal coronal barriers: a 6-month ex vivo study
Noushin Shokouhinejad, Hassan Razmi, Maryam Farbod, Marzieh Alikhasi, Josette Camilleri
Restorative Dentistry & Endodontics.2019;[Epub] CrossRef - Triple antibiotic paste: momentous roles and applications in endodontics: a review
Ardavan Parhizkar, Hanieh Nojehdehian, Saeed Asgary
Restorative Dentistry & Endodontics.2018;[Epub] CrossRef - Mineral trioxide aggregate and other bioactive endodontic cements: an updated overview – part II: other clinical applications and complications
M. Torabinejad, M. Parirokh, P. M. H. Dummer
International Endodontic Journal.2018; 51(3): 284. CrossRef - Alternative to Avoid Tooth Discoloration after Regenerative Endodontic Procedure: A Systematic Review
Luciane Geanini Pena dos Santos, Luiz Alexandre Chisini, Camila Guerner Springmann, Beatriz Dulcineia Mendes de Souza, Fernanda Geraldo Pappen, Flávio Fernando Demarco, Mara Cristina Santos Felippe, Wilson Tadeu Felippe
Brazilian Dental Journal.2018; 29(5): 409. CrossRef - Regenerative Endodontic Treatment or Mineral Trioxide Aggregate Apical Plug in Teeth with Necrotic Pulps and Open Apices: A Systematic Review and Meta-analysis
Mahmoud Torabinejad, Ali Nosrat, Prashant Verma, Oyoyo Udochukwu
Journal of Endodontics.2017; 43(11): 1806. CrossRef - Revascularization in Immature Permanent Teeth with Necrotic Pulp and Apical Pathology: Case Series
López Carmen, Mendoza Asunción, Solano Beatriz, Yáñez-Vico Rosa, Jiiang H. Jeng
Case Reports in Dentistry.2017;[Epub] CrossRef
- Comparative evaluation of effect of modified triple antibiotic paste and calcium hydroxide as intracanal medicament on microhardness of root dentin: An in vitro study
- 2,141 View
- 9 Download
- 16 Crossref


 KACD
KACD

 First
First Prev
Prev


