Search
- Page Path
- HOME > Search
- Impact of post adhesion on stress distribution: an in silico study
- Kkot-Byeol Bae, Jae-Yoon Choi, Young-Tae Cho, Bin-Na Lee, Hoon-Sang Chang, Yun-Chan Hwang, Won-Mann Oh, In-Nam Hwang
- Restor Dent Endod 2025;50(2):e19. Published online May 21, 2025
- DOI: https://doi.org/10.5395/rde.2025.50.e19
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Objectives
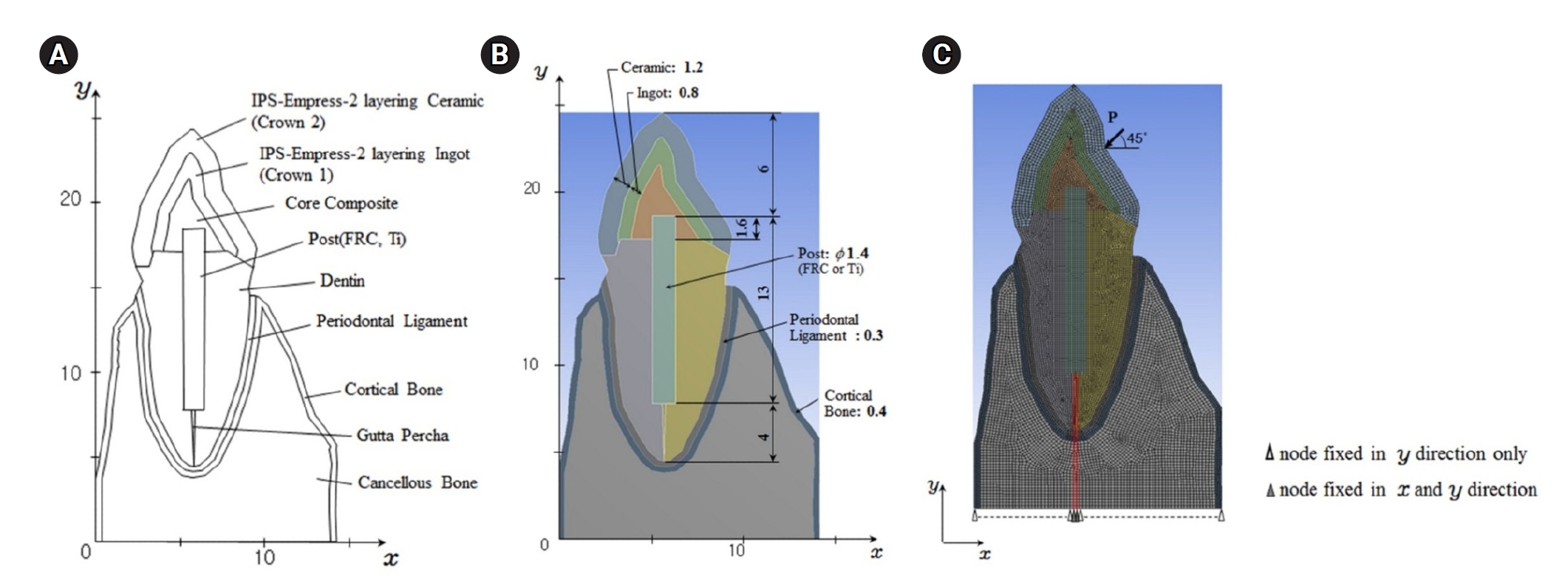
This study aimed to evaluate the stress distribution in teeth restored with different post materials and bonding conditions using finite element analysis (FEA).
Methods
A two-dimensional FEA model of a maxillary central incisor restored with IPS-Empress-2 crown (Ivoclar Vivadent), composite resin core, and posts were created. The model simulated bonded and non-bonded conditions for both fiber-reinforced composite (FRC) and titanium (Ti) posts. Stress distribution was analyzed using ANSYS 14.0 software under a 100-N load applied at a 45° angle to the long axis of the tooth.
Results
The results revealed that stress concentration was significantly higher in non-bonded posts compared to bonded ones. FRC posts exhibited stress values closer to those of dentin, whereas Ti posts demonstrated higher stress concentration, particularly in non-bonded states, increasing the potential risk of damage to surrounding tissues.
Conclusions
FRC posts, with elastic properties similar to dentin and proper adhesion, minimize stress concentration and potential damage to surrounding tissues. Conversely, materials with higher elastic modulus like Ti, can cause unfavorable stress concentrations if not properly bonded, emphasizing the importance of post adhesion in tooth restoration.
- 2,151 View
- 85 Download

- Push-out bond strength and dentinal tubule penetration of different root canal sealers used with coated core materials
- Derya Deniz Sungur, Nuhan Purali, Erdal Coşgun, Semra Calt
- Restor Dent Endod 2016;41(2):114-120. Published online May 4, 2016
- DOI: https://doi.org/10.5395/rde.2016.41.2.114
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives The aim of this study was to compare the push-out bond strength and dentinal tubule penetration of root canal sealers used with coated core materials and conventional gutta-percha.
Materials and Methods A total of 72 single-rooted human mandibular incisors were instrumented with NiTi rotary files with irrigation of 2.5% NaOCl. The smear layer was removed with 17% ethylenediaminetetraacetic acid (EDTA). Specimens were assigned into four groups according to the obturation system: Group 1, EndoRez (Ultradent Product Inc.); Group 2, Activ GP (Brasseler); Group 3, SmartSeal (DFRP Ltd. Villa Farm); Group 4, AH 26 (Dentsply de Trey)/gutta-percha (GP). For push-out bond strength measurement, two horizontal slices were obtained from each specimen (
n = 20). To compare dentinal tubule penetration, remaining 32 roots assigned to 4 groups as above were obturated with 0.1% Rhodamine B labeled sealers. One horizontal slice was obtained from the middle third of each specimen (n = 8) and scanned under confocal laser scanning electron microscope. Tubule penetration area, depth, and percentage were measured. Kruskall-Wallis test was used for statistical analysis.Results EndoRez showed significantly lower push-out bond strength than the others (
p < 0.05). No significant difference was found amongst the groups in terms of percentage of sealer penetration. SmartSeal showed the least penetration than the others (p < 0.05).Conclusions The bond strength and sealer penetration of resin-and glass ionomer-based sealers used with coated core was not superior to resin-based sealer used with conventional GP. Dentinal tubule penetration has limited effect on bond strength. The use of conventional GP with sealer seems to be sufficient in terms of push-out bond strength.
-
Citations
Citations to this article as recorded by- Comparative evaluation of pushout bond strength of three different sealers: An in vitro study
J. S. Beautlin, M. S. Ravisankar, Arvind Kumar Alexander, R. C. Neil Ananth, V. Jevina Christy, K. T. Manoj
Journal of Conservative Dentistry and Endodontics.2025; 28(7): 637. CrossRef - Comparative analysis of dentinal tubule penetration: effects of irrigation activation methods and root canal sealers: in-vitro study
Yagmur Kilic, Mustafa Mert Tulgar, Emrah Karataslioglu, Tugba Turk
BMC Oral Health.2025;[Epub] CrossRef - Comparative evaluation of bioactive calcium silicate coating on functionalized gutta-percha and its effect on bioceramic sealer wettability – An in vitro study
Bollineni Swetha, B. Devi Priya, K. Hanisha Reddy, G. Prasanthi, T. Murali Mohan, Dumpa Tejaswi
Journal of Conservative Dentistry and Endodontics.2025; 28(7): 613. CrossRef - In Vitro and In Vivo Evaluation of a New Experimental Polydimethylsiloxane-Based Endodontic Sealer
Fabiola Cardoso Maldonado, Cesar Gaitan Fonseca, Carlos Bermudez Jimenez, Luis Alejandro Aguilera Galaviz, Margarita L. Martinez-Fierro, Lorena Troncoso Vazquez, Martha Eugenia Reyes Ortiz
Journal of Functional Biomaterials.2025; 16(11): 402. CrossRef - A Comparative Evaluation of Push-Out Bond Strength of Fiber-Reinforced Composite Posts Luted with Two Different Cement Systems: An Ex vivo Study
Shahnaz Shahnawaz, R. P. Shanoj, K. Nandakumar, M. C. Juraise, Smrithi Sudhakaran, R. Shaheena
Journal of Pharmacy and Bioallied Sciences.2025; 17(Suppl 4): S3084. CrossRef - Efficacy of Different Irrigation Activation Techniques on Dentinal Tubule Penetration of the Novel AH-Plus Bioceramic Sealer
Alhasan Almasri, Mohamad Abduljalil, Umut Aksoy
Applied Sciences.2024; 14(2): 701. CrossRef - In Vitro Microscopical and Microbiological Assessment of the Sealing Ability of Calcium Silicate-Based Root Canal Sealers
Karin Christine Huth, Sabina Noreen Wuersching, Leander Benz, Stefan Kist, Maximilian Kollmuss
Journal of Functional Biomaterials.2024; 15(11): 341. CrossRef - Comparative evaluation of dentinal tubule penetration and push-out bond strength of new injectable hydraulic calcium disilicate based root canal sealer: A single blinded in vitro study
Aman Verma, Anshul Arora, Sonali Taneja
Journal of Oral Biology and Craniofacial Research.2024; 14(2): 143. CrossRef - Scanning Electron Microscopy Analysis of the Intratubular Radicular Dentin Penetration of Calcium Hydroxide, Triple Antibiotic Paste, and Nitrofurantoin
Unmesh Khanvilkar, Sanika Pawar, Siddhesh Bandekar, Vaishnavi Dhok, Suraj Arora, Ajinkya M. Pawar, Francesco Pagnoni, Rodolfo Reda, Luca Testarelli
Journal of Personalized Medicine.2023; 13(11): 1554. CrossRef - Influence of access cavity design on calcium hydroxide removal using different cleaning protocols: a confocal laser scanning microscopy study
Seda Falakaloğlu, Merve Yeniçeri Özata, Betül Güneş, Emmanuel João Nogueira Leal Silva, Mustafa Gündoğar, Burcu Güçyetmez Topal
Restorative Dentistry & Endodontics.2023;[Epub] CrossRef - Efficacy of antimicrobial photodynamic therapy and Er,Cr:YSGG laser-activated irrigation on dentinal tubule penetration of MTA-based root canal sealer: a confocal microscopy study
Gül Keskin, Mehmet Çiloğlu
Photodiagnosis and Photodynamic Therapy.2021; 36: 102584. CrossRef - Smear layer removal and sealer penetration with different tapers after using photon-initiated photoacoustic streaming technique
Islam Mohamed Eldeeb, Nawar Naguib Nawar, Shehabeldin Mohamed Saber, Ehab El-Sayed Hassanein, Edgar Schäfer
Clinical Oral Investigations.2021; 25(8): 5025. CrossRef - The Effect of Different Final Irrigation Regimens on the Dentinal Tubule Penetration of Three Different Root Canal Sealers: A Confocal Laser Scanning Microscopy Study In Vitro
Tufan Ozasir, Birgul Eren, Kamran Gulsahi, Mete Ungor, Stefan G. Stanciu
Scanning.2021; 2021: 1. CrossRef - Effect of Vehicle and Agitation Methods on the Penetration of Calcium Hydroxide Paste in the Dentinal Tubules
Mariana de Almeida Barbosa, Kauhanna Vianna de Oliveira, Vinícius Rodrigues dos Santos, Wander José da Silva, Flávia Sens Fagundes Tomazinho, Flares Baratto-Filho, Marilisa Carneiro Leão Gabardo
Journal of Endodontics.2020; 46(7): 980. CrossRef - Micro-computed tomographic evaluation of a new system for root canal filling using calcium silicate-based root canal sealers
Mario Tanomaru-Filho, Fernanda Ferrari Esteves Torres, Jader Camilo Pinto, Airton Oliveira Santos-Junior, Karina Ines Medina Carita Tavares, Juliane Maria Guerreiro-Tanomaru
Restorative Dentistry & Endodontics.2020;[Epub] CrossRef - Dentinal tubule penetration of endodontic sealers after nonthermal plasma treatment: A confocal laser scanning microscopy study
Betul Gunes, Kubra Y. Yeter, Arslan Terlemez, Basak Seker, Yasin Altay
Microscopy Research and Technique.2019; 82(6): 903. CrossRef - Tooth crown discoloration induced by endodontic sealers: a 3-year ex vivo evaluation
Mügem Aslı Ekici, Adil Ekici, Tolga Kaskatı, Bağdagül Helvacıoğlu Kıvanç
Clinical Oral Investigations.2019; 23(5): 2097. CrossRef - Effect of Calcium Hydroxide Dressing on the Dentinal Tubule Penetration of 2 Different Root Canal Sealers: A Confocal Laser Scanning Microscopic Study
Emel Uzunoglu-Özyürek, Özge Erdoğan, Sevinç Aktemur Türker
Journal of Endodontics.2018; 44(6): 1018. CrossRef - Design Variability of the Push-out Bond Test in Endodontic Research: A Systematic Review
James Brichko, Michael F. Burrow, Peter Parashos
Journal of Endodontics.2018; 44(8): 1237. CrossRef - Evaluation of dentinal tubule penetration depth and push-out bond strength of AH 26, BioRoot RCS, and MTA Plus root canal sealers in presence or absence of smear layer
Sevinç Aktemur Türker, Emel Uzunoğlu, Nuhan Purali
Journal of Dental Research, Dental Clinics, Dental Prospects.2018; 12(4): 294. CrossRef - Comparison of Tubular Penetration of AH26, EasySeal, and SureSeal Root Canal Sealers in Single-Rooted Teeth Using Scanning Electron Microscopy
S Toursavadkohi, F Zameni, M Afkar
Journal of Research in Dental and Maxillofacial Sciences.2018; 3(3): 27. CrossRef - Effect of a Low Surface Tension Vehicle on the Dentinal Tubule Penetration of Calcium Hydroxide and Triple Antibiotic Paste
Derya Deniz Sungur, Hacer Aksel, Nuhan Purali
Journal of Endodontics.2017; 43(3): 452. CrossRef
- Comparative evaluation of pushout bond strength of three different sealers: An in vitro study
- 2,124 View
- 13 Download
- 22 Crossref

- The effects of total-etch, wet-bonding, and light-curing of adhesive on the apical seal of a resin-based root canal filling system
- Won-Il Ryu, Won-Jun Shon, Seung-Ho Baek, In-Han Lee, Byeong-Hoon Cho
- J Korean Acad Conserv Dent 2011;36(5):385-396. Published online September 30, 2011
- DOI: https://doi.org/10.5395/JKACD.2011.36.5.385
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives This study evaluated the effects of adhesion variables such as the priming concepts of canal wall and the curing modes of adhesives on the sealing ability of a resin-based root canal filling system.
Materials and Methods Apical microleakage of the Resilon-RealSeal systems filled with 3 different combinations of adhesion variables was compared with the conventional gutta-percha filling using a dye penetration method. Experimental groups were SEDC, Resilon (Resilon Research LLC) filling with self-etch RealSeal (SybronEndo) primer and dual-cure RealSeal sealer; NELC, Resilon filling with no etching, Scotchbond Multi-Purpose (3M ESPE) primer application and light-curing adhesive; and TELC, Resilon filling with Scotchbond Multi-Purpose primer and adhesive used under total etch / wet bonding and light-cure protocols. GPCS, gutta-percha filling with conventional AH26 plus sealer, was the control group.
Results The median longitudinal dye penetration length of TELC was significantly shorter than those of GPCS and SEDC (Kruskal-Wallis test,
p < 0.05). In the cross-sectional microleakage scores, TELC showed significant differences from other groups at 2 to 5 mm from the apical foramen (Kruskal-Wallis test,p < 0.05).Conclusions When a resin-based root canal filling material was used, compared to the self-etching primer and the dual-cure sealer, the total etch/wet-bonding with primer and light-curing of adhesive showed improved apical sealing and was highly recommended.
- 1,154 View
- 1 Download

- Anti-inflammatory effects of PPARγ on human dental pulp cells
- Jeong-Hee Kim
- J Korean Acad Conserv Dent 2006;31(3):203-214. Published online May 31, 2006
- DOI: https://doi.org/10.5395/JKACD.2006.31.3.203
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Dental pulp is a loose, mesenchymal tissue almost entirely enclosed in the dentin. It consists of cells, ground substance, and neural and vascular supplies. Damage to the dental pulp by mechanical, chemical, thermal, and microbial irritants can provoke various types of inflammatory response. Pulpal inflammation leads to the tissue degradation, which is mediated in part by Matrix metalloproteinase leads to accelerate extracellular matrix degradation with pathological pathway. We have now investigated the induction of MMPs and inflammatory cytokines by Lipopolysaccharide (LPS) control of inflammatory mediators by peroxisome proliferator-activated receptors (PPARs).
Human dental pulp cells exposed to various concentrations of LPS (1-10 µg/ml) revealed elevated levels of MMP-2 and MMP-9 at 24 hrs of culture. LPS also stimulated the production of ICAM-1, VCAM-1, IL-1β, and TNF-α. Adenovirus PPARγ (Ad/PPARγ) and PPARγ agonist rosiglitazone reduced the synthesis of MMPs, adhesion molecules and pro-inflammatory cytokines. The inhibitory effect of Ad/PPARγ was higher than that of PPARγ agonist.
These result offer new insights in regard to the anti-inflammatory potential of PPARγ in human dental pulp cell.
- 1,084 View
- 1 Download

- Effect of a rewetting agent on dentin adhesion
- Young-Gon Cho, Yil-Yoon Park, Young-Gon Lee
- J Korean Acad Conserv Dent 2003;28(1):11-22. Published online January 31, 2003
- DOI: https://doi.org/10.5395/JKACD.2003.28.1.011
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub This study compared the dentin adhesion to composite resin according to air-dry, blot dry, application of rewetting agent on air-dry or blot dry dentin surface by microleakag test and SEM observation.
For microleakage test, class V cavity preparations with dentinal margins were prepared on both buccal and lingual surfaces of 40 extracted human molars. For SEM observation, occlusal dentin of 20 extracted human molars were exposed.
After etched the dentin, prepared teeth were randomly divided into four groups;
D group: air dry for 10-15 sec., B group: blot dry with moist cotton pellet, D-R group: air dry and rewet with Aqua-Prep F for 20 sec., B-R group: blot dry and rewet with Aqua-Prep F for 20 sec.
Treated cavities and surfaces were filled or constructed using One-Step adhesives and Aelitefil composite resins. Specimens were stored in distilled water for 24 hours. For microleakage test, the specimens were thermocycled and soaked into 2% methylene blue. The specimens were sectioned longitudinally and evaluated for microleakage under steromicroscope. The data were statistically analysed by Kruskal-Wallis Test, Mann-Whitney and Wilcoxon signed ranked tests. For SEM observation, the specimens were bisectioned mesiodiatally. After decalcified and deproteinized, specimens were observed under SEM.
The results of this study were as follows;
1. The microleakges on dentinal margin were the highest in D group compared with B group, D-R group, and B-R group(p<0.05). But there was no significant difference between B group, D-R group and B-R group.
2. D group showed gap and a few resin tags between dentin and composite resin.
3. B group, D-R group, and B-R groups showed close adaptation between dentin and composite resin. It showed that resin rags in B group were numerous and long, in D-R group were few and short, in B-R group were numerous and short or long.
4. Adhesive layer showed in D-R group (10 µm) and B-R group (3 µm)
In conclusion, use of rewetting agent to dry dentin was efficient to dentin adhesion, also it did not provide reverse effect on blot dry dentin.
-
Citations
Citations to this article as recorded by- Effect of rewetting agent on dentinal microtensile bond strength
Hee-Young Kang, Young-Gon Cho, Jong-Uk Kim, Byung-Cheul Park, Sang-Hoon Yoo, Cheul-Hee Jin, Hee-Young Choi, Young-Jae Ki
Journal of Korean Academy of Conservative Dentistry.2004; 29(2): 153. CrossRef
- Effect of rewetting agent on dentinal microtensile bond strength
- 1,007 View
- 3 Download
- 1 Crossref


 KACD
KACD

 First
First Prev
Prev


