-
Cone-beam computed tomography in endodontics: from the specific technical considerations of acquisition parameters and interpretation to advanced clinical applications
-
Néstor Ríos-Osorio, Sara Quijano-Guauque, Sandra Briñez-Rodríguez, Gustavo Velasco-Flechas, Antonieta Muñoz-Solís, Carlos Chávez, Rafael Fernandez-Grisales
-
Restor Dent Endod 2024;49(1):e1. Published online December 11, 2023
-
DOI: https://doi.org/10.5395/rde.2024.49.e1
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
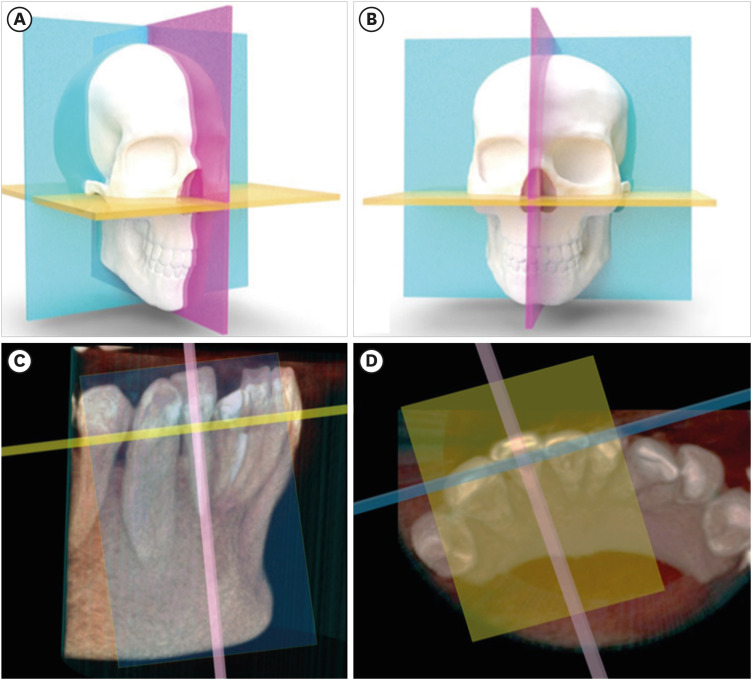
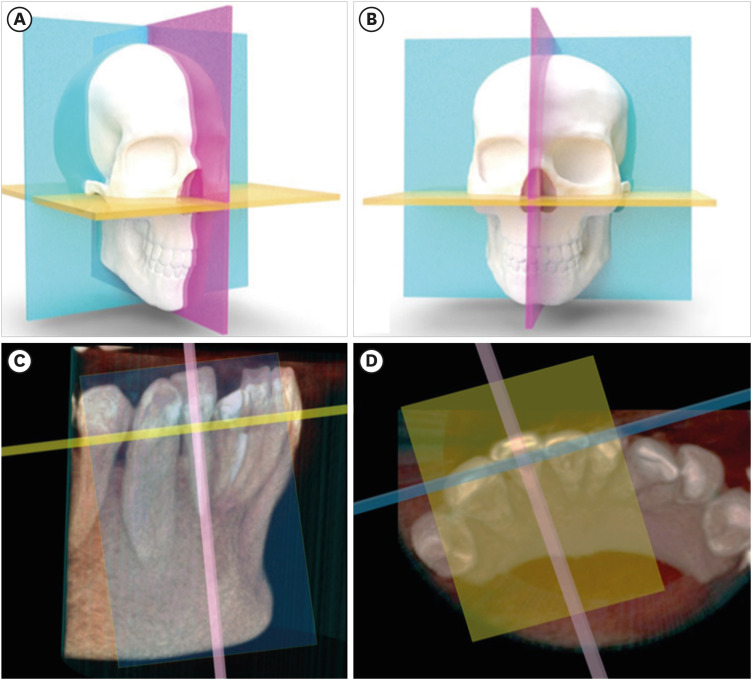
The implementation of imaging methods that enable sensitive and specific observation of anatomical structures has been a constant in the evolution of endodontic therapy. Cone-beam computed tomography (CBCT) enables 3-dimensional (3D) spatial anatomical navigation in the 3 volumetric planes (sagittal, coronal and axial) which translates into great accuracy for the identification of endodontic pathologies/conditions. CBCT interpretation consists of 2 main components: (i) the generation of specific tasks of the image and (ii) the subsequent interpretation report. A systematic and reproducible method to review CBCT scans can improve the accuracy of the interpretation process, translating into greater precision in terms of diagnosis and planning of endodontic clinical procedures. MEDLINE (PubMed), Web of Science, Google Scholar, Embase and Scopus were searched from inception to March 2023. This narrative review addresses the theoretical concepts, elements of interpretation and applications of the CBCT scan in endodontics. In addition, the contents and rationale for reporting 3D endodontic imaging are discussed. -
Citations
Citations to this article as recorded by  - Evaluation of Maxillary Sinus Pathologies in Children and Adolescents with Cleft Lip and Palate Using Cone Beam Computed Tomography: A Retrospective Study
Ayşe Çelik, Nilüfer Ersan, Senem Selvi-Kuvvetli
The Cleft Palate Craniofacial Journal.2025;[Epub] CrossRef - Machine Learning Models in the Detection of MB2 Canal Orifice in CBCT Images
Shishir Shetty, Meliz Yuvali, Ilker Ozsahin, Saad Al-Bayatti, Sangeetha Narasimhan, Mohammed Alsaegh, Hiba Al-Daghestani, Raghavendra Shetty, Renita Castelino, Leena R David, Dilber Uzun Ozsahin
International Dental Journal.2025; 75(3): 1640. CrossRef - Bildgebung im ZMK-Bereich – aber in welcher Reihenfolge?
Rainer Lutz
Zahnmedizin up2date.2024; 18(04): 297. CrossRef - Cone-beam computed tomography evaluation of shaping ability of kedo-S square and fanta AF™ baby rotary files compared to manual K-files in root canal preparation of primary anterior teeth
Shaimaa S. El-Desouky, Bassem N. El Fahl, Ibrahim A. Kabbash, Shimaa M. Hadwa
Clinical Oral Investigations.2024;[Epub] CrossRef - Analysis of Endodontic Successes and Failures in the Removal of Fractured Endodontic Instruments during Retreatment: A Systematic Review, Meta-Analysis, and Trial Sequential Analysis
Mario Dioguardi, Corrado Dello Russo, Filippo Scarano, Fariba Esperouz, Andrea Ballini, Diego Sovereto, Mario Alovisi, Angelo Martella, Lorenzo Lo Muzio
Healthcare.2024; 12(14): 1390. CrossRef
-
412
View
-
64
Download
-
3
Web of Science
-
5
Crossref
-
Association between cigarette smoking and the prevalence of post-endodontic periapical pathology: a systematic review and meta-analysis
-
Néstor Ríos-Osorio, Hernan Darío Muñoz-Alvear, Fabio Andrés Jiménez-Castellanos, Sara Quijano-Guauque, Oscar Jiménez-Peña, Herney Andrés García-Perdomo, Javier Caviedes-Bucheli
-
Restor Dent Endod 2022;47(3):e27. Published online June 13, 2022
-
DOI: https://doi.org/10.5395/rde.2022.47.e27
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
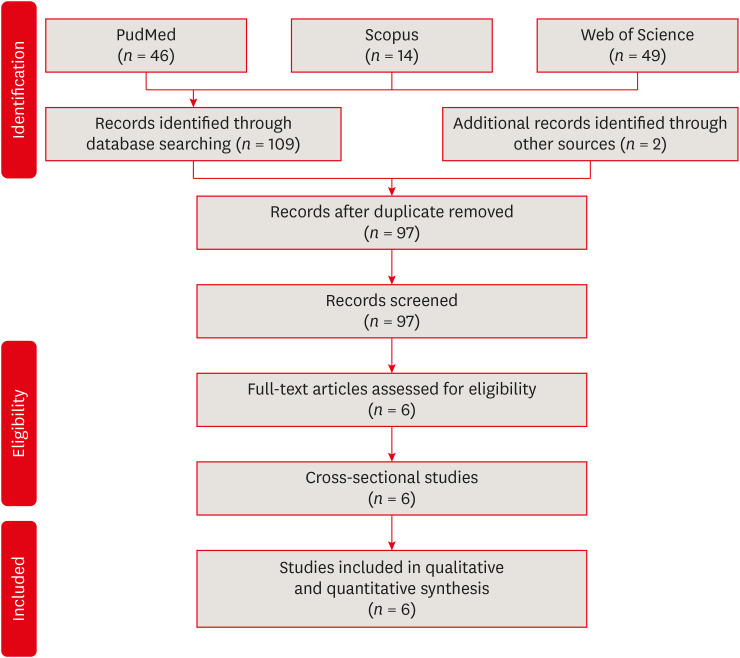
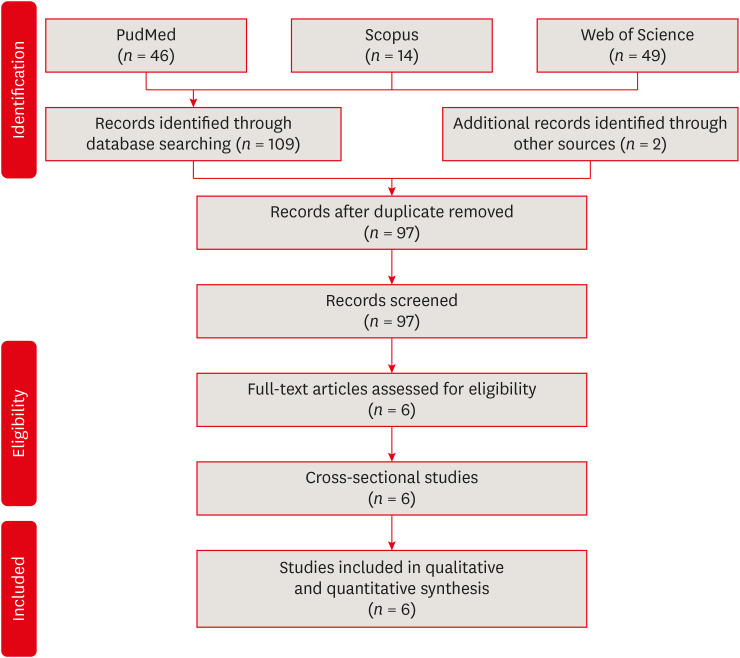
- Objectives
This systematic review and meta-analysis aimed to assess the association of cigarette smoking with the prevalence of post-endodontic apical periodontitis in humans. Materials and MethodsWe searched through PubMed/Medline, Web of Science, and Scopus from inception to December 2020. Risk of bias was performed by using the Newcastle-Ottawa Scale for cross-sectional, cohort, and case-control studies. We performed the statistical analysis in Review Manager 5.3 (RevMan 5.3). Results6 studies met the inclusion criteria for qualitative and quantitative synthesis. Statistical analysis of these studies suggests that there were no differences in the prevalence of post endodontic apical periodontitis (AP) when comparing non-smokers vs smoker subjects regarding patients (odds ratio [OR], 0.68; 95% confidence interval [CI], 0.31–1.49; I2 = 58%) and teeth (OR, 1.71; 95% CI, 0.99–2.93; I2 = 72%). ConclusionsOur findings suggest that there was no association between cigarette smoking and post-endodontic apical periodontitis, as we did not find statistical differences in the prevalence of post-endodontic AP when comparing non-smokers vs smoker subjects. Therefore, smoking should not be considered a risk factor associated with endodontic failure.
|