-
Bioactivity of endodontic biomaterials on dental pulp stem cells through dentin
-
Bahar Javid, Narges Panahandeh, Hassan Torabzadeh, Hamid Nazarian, Ardavan Parhizkar, Saeed Asgary
-
Restor Dent Endod 2020;45(1):e3. Published online November 4, 2019
-
DOI: https://doi.org/10.5395/rde.2020.45.e3
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Objectives
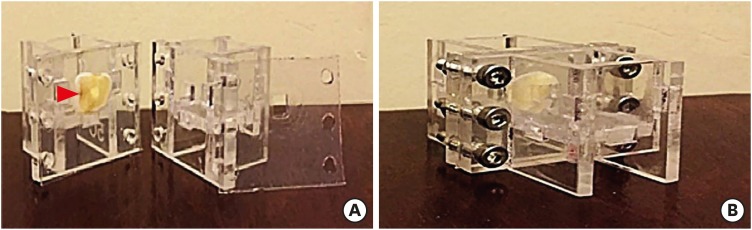
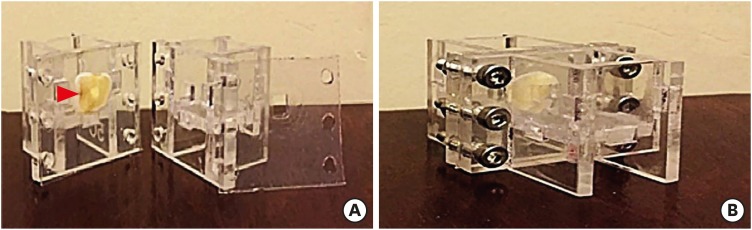
This study investigated the indirect effect of calcium-enriched mixture (CEM) cement and mineral trioxide aggregate (MTA), as 2 calcium silicate-based hydraulic cements, on human dental pulp stem cells (hDPSCs) through different dentin thicknesses. Materials and MethodsTwo-chamber setups were designed to simulate indirect pulp capping (IPC). Human molars were sectioned to obtain 0.1-, 0.3-, and 0.5-mm-thick dentin discs, which were placed between the 2 chambers to simulate an IPC procedure. Then, MTA and CEM were applied on one side of the discs, while hDPSCs were cultured on the other side. After 2 weeks of incubation, the cells were removed, and cell proliferation, morphology, and attachment to the discs were evaluated under scanning electron microscopy (SEM). Energy-dispersive X-ray (EDXA) spectroscopy was performed for elemental analysis. Alkaline phosphatase (ALP) activity was assessed quantitatively. The data were analyzed using the Kruskal-Wallis and Mann-Whitney tests. ResultsSEM micrographs revealed elongated cells, collagen fibers, and calcified nucleations in all samples. EDXA verified that the calcified nucleations consisted of calcium phosphate. The largest calcifications were seen in the 0.1-mm-thick dentin subgroups. There was no significant difference in ALP activity across the CEM subgroups; however, ALP activity was significantly lower in the 0.1-mm-thick dentin subgroup than in the other MTA subgroups (p < 0.05). ConclusionsThe employed capping biomaterials exerted biological activity on hDPSCs, as shown by cell proliferation, morphology, and attachment and calcific precipitations, through 0.1- to 0.5-mm-thick layers of dentin. In IPC, the bioactivity of these endodontic biomaterials is probably beneficial.
-
Citations
Citations to this article as recorded by  - Dental pulp capping materials: modulators of stem cell behavior and regenerative potential
Ali Cheayto, Sara Ayoub, Sarah Ayad Al-Tameemi, Mohammad Fayyad-Kazan
Biomedical Physics & Engineering Express.2025; 11(6): 062004. CrossRef - Effect of pulp capping materials on odontogenic differentiation of human dental pulp stem cells: An in vitro study
Mahmoud M. Bakr, Mohamed Shamel, Shereen N. Raafat, Robert M. Love, Mahmoud M. Al‐Ankily
Clinical and Experimental Dental Research.2024;[Epub] CrossRef - Effects of Growth Factors on the Differentiation of Dental Stem Cells: A
Systematic Review and Meta-analysis (Part I)
Sayna Shamszadeh, Armin Shirvani, Hassan Torabzadeh, Saeed Asgary
Current Stem Cell Research & Therapy.2024; 19(4): 523. CrossRef - The Role of Growth Factor Delivery Systems on Cellular Activities of Dental
Stem Cells: A Systematic Review (Part II)
Sayna Shamszadeh, Armin Shirvani, Saeed Asgary
Current Stem Cell Research & Therapy.2024; 19(4): 587. CrossRef - Comprehensive review of composition, properties, clinical applications, and future perspectives of calcium-enriched mixture (CEM) cement: a systematic analysis
Saeed Asgary, Mahtab Aram, Mahta Fazlyab
BioMedical Engineering OnLine.2024;[Epub] CrossRef - Evaluation of dental pulp stem cells behavior after odontogenic differentiation induction by three different bioactive materials on two different scaffolds
Basma Ahmed, Mai H. Ragab, Rania A. Galhom, Hayam Y. Hassan
BMC Oral Health.2023;[Epub] CrossRef - Characterization of Dental Pulp Stem Cell Responses to Functional Biomaterials Including Mineralized Trioxide Aggregates
Sejin Bae, Bueonguk Kang, Hyungbin Lee, Harrison Luu, Eric Mullins, Karl Kingsley
Journal of Functional Biomaterials.2021; 12(1): 15. CrossRef - Incorporation of amoxicillin-loaded microspheres in mineral trioxide aggregate cement: an in vitro study
Fábio Rocha Bohns, Vicente Castelo Branco Leitune, Isadora Martini Garcia, Bruna Genari, Nélio Bairros Dornelles, Silvia Stanisçuaski Guterres, Fabrício Aulo Ogliari, Mary Anne Sampaio de Melo, Fabrício Mezzomo Collares
Restorative Dentistry & Endodontics.2020;[Epub] CrossRef
-
1,223
View
-
11
Download
-
8
Crossref
-
Triple antibiotic paste: momentous roles and applications in endodontics: a review
-
Ardavan Parhizkar, Hanieh Nojehdehian, Saeed Asgary
-
Restor Dent Endod 2018;43(3):e28. Published online June 20, 2018
-
DOI: https://doi.org/10.5395/rde.2018.43.e28
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
This study investigated the latest findings and notions regarding ‘triple antibiotic paste’ (TAP) and its applications in dentistry, particularly endodontics. TAP is a combination of 3 antibiotics, ciprofloxacin, metronidazole, and minocycline. Despite the problems and pitfalls research pertaining to this paste has unveiled, it has been vastly used in endodontic treatments. The paste's applications vary, from vital pulp therapy to the recently introduced regeneration and revascularisation protocol. Studies have shown that the paste can eliminate the root canal microorganisms and prepare an appropriate matrix for further treatments. This combination is able to remove diverse groups of obligate and facultative gram-positive and gram-negative bacteria, providing an environment for healing. In regeneration protocol cases, this allows the development, disinfection, and possible sterilization of the root canal system, so that new tissue can infiltrate and grow into the radicular area. Moreover, TAP is capable of creating a discipline in which other wanted and needed treatments can be successfully performed. In conclusion, TAP, as an antibacterial intracanal medication, has diverse uses. Nevertheless, despite its positive effects, the paste has shown drawbacks. Further research concerning the combined paste and other intracanal medications to control microbiota is a must. -
Citations
Citations to this article as recorded by  - Endodontic Intracanal Medicaments and Agents
Anu Priya Guruswamy Pandian, Depti Bellani, Ritya Mary Jibu, Varsha Agnihotri
Dental Clinics of North America.2026; 70(1): 45. CrossRef - Evaluation of Effect of Laser in Root Canal Disinfection in Pulp Regenerative Therapy: A Systematic Review
Kiran Kumar N, Abhishek M, Savitha B. Naik, Biji Brigit, Swetha Geervani V, M Manimozhi
Photobiomodulation, Photomedicine, and Laser Surgery.2025; 43(2): 53. CrossRef - Assessing Cell Viability: Comparative Analysis of Calcium Hydroxide, Triple Antibiotic Paste, and Their Synergistic Impact on human Dental Pulp Stem Cells
Dini Asrianti Bagio, Ibramanto Warganegara, Ike Dwi Maharti, Anggraini Margono, Citra Kusumasari, Sylva Dinie Alinda, Valeria Widita Wairooy
European Journal of General Dentistry.2025; 14(01): 073. CrossRef - Cytotoxic and Antibiofilm Properties of Antibiotic-Loaded Thermoresponsive Hydrogels for Root Canal Therapy
Cristiane Duque, Gabriela Pacheco de Almeida Braga, Juliana Machado de Carvalho, Karina Sampaio Caiaffa, Gabriel Pereira Nunes, Rafaela Laruzo Rabelo, Vanessa Rodrigues dos Santos, Geórgia Rondó Peres, Lucas da Silva Ribeiro, Emerson Rodrigues de Camargo
Processes.2025; 13(3): 661. CrossRef - Antibiofilm properties, cytotoxicity, and effect on protease activity of antibiotics and EGCG-based medications for endodontic purposes
Daniela Alvim Chrisostomo, Jesse Augusto Pereira, Polliana Mendes Candia Scaffa, Zach Gouveia, Gabriel Flores Abuna, Sergey V. Plotnikov, Anuradha Prakki, Cristiane Duque
Journal of Dentistry.2025; 156: 105660. CrossRef - The use of three-dimensional-printed guides, static navigation, and bioactive materials to treat bilateral and double dens invaginatus
Parth Patel, Nidhi Bharti, Ankit Arora, C. Nimisha Shah
Saudi Endodontic Journal.2025; 15(2): 207. CrossRef - To Assess the Cell Viability of Triple Antibiotic Paste under Confocal Microscope: An In Vitro Study
Elanthendral Saravanan, Mahesh Ramakrishnan
Journal of South Asian Association of Pediatric Dentistry.2025; 8(2): 81. CrossRef - Eficacia de la pasta triantibiótica en endodoncia: actividad antibacteriana frente a cepas resistentes de Enterococcus faecalis. Una revisión exhaustiva
Elena Patricia Cevallos Fernández, Katherine de los Ángeles Cuenca León
Anatomía Digital.2025; 8(3.1): 88. CrossRef - Efectividad de diferentes antimicóticos, junto con la pasta triantibiotica, para el tratamiento de Candida albicans en conductos radiculares
Carlos Andrés Rodríguez Tapia, Jessica María Sarmiento Ordoñez
Anatomía Digital.2025; 8(3.2): 45. CrossRef - Comparative Evaluation of Calcium Hydroxide, Triple Antibiotic Paste, and Calcium Hydroxide with 2% Chlorhexidine as Intracanal Medicaments in Reducing Interappointment Pain during Endodontic Treatment: An In Vivo Study
Rachit Mathur, Shaista Gazal, Itika Jain, Shyam Agrawal, Akshada Mungee, Babra Khan
International Journal of Clinical Pediatric Dentistry.2025; 18(6): 628. CrossRef - In Vitro Effectiveness of Endodontic Triple Antibiotic Paste Associated With Daptomycin
Sabrina S Azevedo, Gabriela C Chianca, Bruna A Thurler, Raiane C Chamon, Helvécio C Corrêa Póvoa, Leonardo S Antunes, Natalia L Pontes Póvoa Iorio
Cureus.2025;[Epub] CrossRef - Effect of Chitosan and bioactive glass nanomaterials as intracanal medicaments on TGF-β1 release from intraradicular dentin
Sarah Salah Hashem, Mohammed M. Khalefa, Mahmoud Hassan Mohamed, Hemat M. ELSheikh, Fatma Abd El-Rahman Taher
BMC Oral Health.2025;[Epub] CrossRef - Clinical and radiographic success of lesion sterilization and tissue repair in primary teeth: a systematic review and meta-analysis
Khlood Baghlaf, Rana A. Alamoudi
The Saudi Dental Journal.2025;[Epub] CrossRef - A Comparative Evaluation of Herbal Extracts and Triple Antibiotic Paste as Intracanal Medicament against Enterococcus faecalis: A Microbiological Study
Divya Singh, Rashi Singh, Nidhi Gupta, Natasha Gambhir, Saritha Golla
International Journal of Clinical Pediatric Dentistry.2024; 17(3): 285. CrossRef - Comparative Evaluation of Push-Out Bond Strength of Conventional Mineral Trioxide Aggregate, Biodentine, a Modified Mineral Trioxide Aggregate, and Two Novel Antibacterial-Enhanced Mineral Trioxide Aggregates
Arokia Rajkumar Shancy Merlin, Vignesh Ravindran, Ganesh Jeevanandan, Rajalakshmanan Eswaramoorthy, Abirami Arthanari
Cureus.2024;[Epub] CrossRef - In Vitro Evaluation of the Effect of Oleanolic Acid as a Potential Root Canal Medicament on Viability and Proliferation of Dental Pulp Stem Cells
Khalifah A. Alhaila, Manal Farouk Badawi, Mohamed G. Elbeltagy, Amany E. Badr
European Journal of General Dentistry.2024; 13(01): 051. CrossRef - Regenerative Endodontic Treatment in Dentinogenesis Imperfecta‐Induced Apical Periodontitis
Ying Liao, Ting Pan, Xianghui Xing, Sivakumar Nuvvula
Case Reports in Dentistry.2024;[Epub] CrossRef - Efecto antimicrobiano como medicación intraconducto de la pasta triantibiótica.
Paúl Sebastián Ulloa Amores, Diana Álvarez Álvarez, María Elizabeth Moscoso Abad, Magda Zulay Bastidas Calva
Revista de la Asociación Dental Mexicana.2024; 81(4): 211. CrossRef - Synthesis and Characterization of Nanosilica-Coated Antibiotics, TAP: A Comprehensive Study Utilizing XRD, EDS, FTIR, SEM, and TEM – Invitro Study
Mahaboob S. Hameed, S. Delphine P. Antony, Rajeshkumar Shanmugam, Sandhya Raghu
Journal of International Oral Health.2024; 16(5): 386. CrossRef - Association between host defence peptide IDR‐1002 and ciprofloxacin: Effects on human dental pulp cells
Danilo César Mota Martins, Maurício Gonçalves da Costa Sousa, Poliana Amanda Oliveira Silva, Lana Ribeiro Aguiar, Rosângela Vieira de Andrade, Amandda Évellin Silva‐Carvalho, Felipe Saldanha‐Araújo, Octávio Luiz Franco, Taia Maria Berto Rezende
Australian Endodontic Journal.2024; 50(3): 547. CrossRef - Comparative evaluation of antimicrobial efficacy of triple antibiotic paste and amoxicillin clavulanate paste as an intracanal medicament against Enterococcus faecalis: An in vitro study
Dhandayuthapani Sasikala, Parisa Norouzi Baghkomeh, Jamaluddin Mohammed Farzan
Dental Research Journal.2024;[Epub] CrossRef - Triple Antibiotic Paste: A Game Changer in Endodontics
Kalagi G. Panchal, Karima Virani, Vraj Patel, Aquib Ali Khan, Anam Pettiwala, Srikala S. Puranik, Srushti Joshi
Journal of Pharmacy and Bioallied Sciences.2024; 16(Suppl 3): S1913. CrossRef - Non-surgical Management of a Large Periapical Lesion: A Case Study of the Successful Application of a Modified Triple Antibacterial Paste
Srushti Awghad, Joyeeta Mahapatra, Amit Reche, Ankita Burse, Aradhana Kibe
Cureus.2024;[Epub] CrossRef - Enhancing Antimicrobial Efficacy and Synergistic Effects of Nano-Silica-Based Combinations With Doxycycline, Metronidazole, and Ciprofloxacin Against Enterococcus faecalis Biofilms
Shahul Hameed, Delphine P Antony, Rajeshkumar Shanmugam, Sandhya Raghu, Hima Sandeep Adimulapu
Cureus.2024;[Epub] CrossRef - Healing of periapical lesion by non-surgical endodontic therapy: A case series
Athira Ramesh, Rajesh Pillai, Afzal A, Anakha Santhosh, Arunima G.S, Sandeep K. V
IP Indian Journal of Conservative and Endodontics.2024; 9(2): 99. CrossRef - Effect of Calcium Hydroxide Versus Double Antibiotic Paste on Endodontic Treatment Outcomes in Teeth With Large Periapical Lesions: A Triple‐Blind Randomized Clinical Trial
Afsaneh Rahmati, Farshad Seyedein, Omid Dianat, Sara Saedi, Golriz Rostami, Alireza Akbarzadeh Baghban, Shima Sabertahan, Majid Kazem, Kee Y. Kum
International Journal of Dentistry.2024;[Epub] CrossRef - Can antimicrobial photodynamic therapy serve as an effective adjunct protocol for disinfecting the necrotic root canal system? A randomized controlled study
Remy Barazy, Hisham Alafif, Hassan Achour, Ahmad Al-Aloul, Yasser Alsayed Tolibah
BDJ Open.2024;[Epub] CrossRef - Drain and Treat: A Rubber Dam Technique for Acute Periapical Abscess
S. Grover, K. Mala, J. D’Souza
Acta Medica Bulgarica.2024; 51(s2): 143. CrossRef - Microbial Dynamics in Endodontic Pathology—From Bacterial Infection to Therapeutic Interventions—A Narrative Review
Klara Wieczorkiewicz, Anna Jarząbek, Estera Bakinowska, Kajetan Kiełbowski, Andrzej Pawlik
Pathogens.2024; 14(1): 12. CrossRef - An in vitro comparative evaluation of the effect of three intracanal medicaments – chlorhexidine gel, triple antibiotic paste, and calcium hydroxide paste on the push-out bond strength of MTA Plus, Biodentine, and calcium-enriched mixture
Gouthami Datta, Ramya Raghu, Ashish Shetty, Gautham P Manjunath, Dishant Patel, Subhashini Rajasekhara
Endodontology.2023; 35(1): 60. CrossRef - The cytotoxic effect of cysteamine and its combinations with various endodontic intracanal medications on fibroblast cells: in vitro study
Esraa Adel Mohamed Abd Elhameed ElGammal, Abeer Hashem Mahran, Salma Hassan El Ashry, Sara Hossam Fahmy
Bulletin of the National Research Centre.2023;[Epub] CrossRef - Healing of large endodontic lesions using a new combination of triple antibiotics: A case report
Saeed Asgary, Ardavan Parhizkar
Clinical Case Reports.2023;[Epub] CrossRef - Effects of Intracanal Medicaments on the Measurement Accuracy of Four Apex Locators: An In Vitro Study
Hamza Cudal, Tuğrul Aslan, Bertan Kesim
Meandros Medical and Dental Journal.2023; 24(3): 215. CrossRef - Comparative evaluation of the antibacterial efficacy of herbal agents as intracanal medicaments individually or in combination with chitosan: An in vitro RTPCR study
Gaurav Patri, Kotni Sheetal, PrasantiKumar Pradhan, Pratik Agrawal, S Lata
Journal of International Oral Health.2023; 15(1): 89. CrossRef - Recent progress in carbon dots for anti-pathogen applications in oral cavity
Yuying Jiang, Chuqiang Yin, Jianning Mo, Xiaoyu Wang, Ting Wang, Guotai Li, Qihui Zhou
Frontiers in Cellular and Infection Microbiology.2023;[Epub] CrossRef - A Comprehensive Review of Lesion Sterilization and Tissue Repair: An Alternative for Pulpectomy in Deciduous Teeth
Aparna Achanta, Amit Reche, Rishika Dakhale, Rudra R Bharate
Cureus.2023;[Epub] CrossRef - Healing of Large Endodontic Lesions Using Long‐Term Application of a New Combination of Triple Antibiotics: A Series of Cases
Saeed Asgary, Ardavan Parhizkar, Maria Beatriz Duarte Gavião
Case Reports in Dentistry.2023;[Epub] CrossRef - Non-cytotoxic Root Canal Dressing with Improved Antimicrobial Efficacy
Farzad Koosha, Jerome Cymerman, Thomas Manders, Marcia Simon, Stephen Walker, Miriam Rafailovich
Journal of Endodontics.2023; 49(2): 205. CrossRef - Triple antibiotics: A synergistic approach to combating infection
Hemant Sawhney, Anukriti Kumari, Ritik Kashwani, Geetanjali Gupta, SJ Das
IP Indian Journal of Conservative and Endodontics.2023; 8(4): 189. CrossRef - A 1-year Clinical and Radiographic Assessment of Regenerative Endodontic Therapy for Necrotic Primary Molars: A Randomized controlled Trial
Dina D Abdelmoneim, Amr M Abdelaziz, Gehan G Allam, Amira S Badran
International Journal of Clinical Pediatric Dentistry.2023; 16(2): 295. CrossRef - “BIODENTINE” THE DENTINE IN A CAPSULE AS AN APICAL BARRIER IN TRAUMATIZED MAXILLARY CENTRAL INCISOR WITH TWO YEARS FOLLOW UP.
Savita Thakur, Udai Bhanu, Gurkirat Singh Grewal
INTERNATIONAL JOURNAL OF SCIENTIFIC RESEARCH.2022; : 64. CrossRef - Long-term treatment of dentine with triple antibiotic paste promotes stem cell viability and attachment
Samiya Riaz, Ahmad Azlina, Zuliani Mahmood, Aung T. Htun
Journal of Taibah University Medical Sciences.2022; 17(4): 630. CrossRef - Non surgical management of trauma induced root resorption and large periapical
lesion using bioactive material- A case report
Tejasvini Prajapati, Sonali Kapoor, Purnil Shah, Ankit Arora, Hardik Rana
Clinical Dentistry.2022;[Epub] CrossRef - Antibacterial efficacy of antibiotic pastes versus calcium hydroxide intracanal dressing: A systematic review and meta-analysis of ex vivo studies
Mohammadreza Vatankhah, Kamyar Khosravi, Nazanin Zargar, Armin Shirvani, MohammadHossein Nekoofar, Omid Dianat
Journal of Conservative Dentistry.2022; 25(5): 463. CrossRef - Triple Antibiotic Paste: A Suitable Medicament for Intracanal Disinfection
Krutika Malu, Monika Khubchandani
Cureus.2022;[Epub] CrossRef - Present status and future directions of intracanal medicaments
Ronald Ordinola‐Zapata, W. Craig Noblett, Alejandro Perez‐Ron, Zhou Ye, Jorge Vera
International Endodontic Journal.2022; 55(S3): 613. CrossRef - The effect of four different intracanal medicaments on the push-out bond strength of root canal sealers
Shalu Maan, Vijaya Dhar Bhatt, Rohit Singh, Sayak Gupta, Syed Alay Noorain, Aashna Gill, Pradeep Kumar, Sushil Yadav, Preeti Sharma
Journal of Medicine and Life.2022; 15(4): 448. CrossRef - A Comparative Evaluation of Microhardness and Chemical Structure of Radicular Dentin with Two Combinations of TAP and MTAP: An In Vitro Study
P Niharika, Saigeeta Kondamadugu, Nagireddy Venugopal Reddy, Muthumula Daneswari, Annie P Chris, Nikhila V Reddy
International Journal of Clinical Pediatric Dentistry.2022; 15(S2): S151. CrossRef - Comparative Evaluation of Two Antibiotic Pastes for Root Canal Disinfection
Sadhna Sharma, Urvashi Bhushan, Mridula Goswami, CP Baveja
International Journal of Clinical Pediatric Dentistry.2022; 15(S1): S12. CrossRef - Management of External Inflammatory Root Resorption following Tooth Autotransplantation Using a Modified Combination of Triple Antibiotics
Saeed Asgary, Ardavan Parhizkar, Paulo J. Palma
Case Reports in Dentistry.2022;[Epub] CrossRef - Effect of triple antibiotic paste on the bond strength of epoxy and methacrylate resin-based sealers to root canal dentin
Fereshte Sobhnamayan, Alireza Adl, Mahdi Sedigh-Shams, Hossein Mirkhaghani
Journal of Conservative Dentistry.2022; 25(4): 426. CrossRef - Progress of Research on the Application of Triple Antibiotic Paste and Hydrogel Scaffold Materials in Endodontic Revascularization: A Systematic Review
Jia Zhao, Tian Jiao Wang
Evidence-Based Complementary and Alternative Medicine.2022; 2022: 1. CrossRef - The effect of different intracanal medicaments on the dislodgement resistance of mineral trioxide aggregate
Farzaneh Afkhami, Shahrzad Razavi, Sholeh Ghabraei
BMC Oral Health.2022;[Epub] CrossRef - Efficacy of Ciprofloxacin, Metronidazole and Minocycline in Ordered Mesoporous Silica against Enterococcus faecalis for Dental Pulp Revascularization: An In-Vitro Study
Cintia Micaela Chamorro-Petronacci, Beatriz Santos Torres, Rocío Guerrero-Nieves, Mario Pérez-Sayáns, Marcia Carvalho-de Abreu Fantini, Luis Carlos Cides-da-Silva, Beatriz Magariños, Berta Rivas-Mundiña
Materials.2022; 15(6): 2266. CrossRef - Antibiotic Mixtures in Noninstrumental Endodontic Treatment of Primary Teeth with Necrotic Pulps: A Systematic Review
Farah Chouchene, Fatma Masmoudi, Ahlem Baaziz, Fethi Maatouk, Hichem Ghedira, Sivakumar Nuvvula
International Journal of Dentistry.2021; 2021: 1. CrossRef - Potential apply of hydrogel-carried chlorhexidine and metronidazole in root canal disinfection
Yanhong YAN, Peng ZHOU, Haibing LU, Yun GUAN, Ming MA, Juan WANG, Guangwei SHANG, Beizhan JIANG
Dental Materials Journal.2021; 40(4): 986. CrossRef - Evaluation of the Effect of Nitrofurantoin Paste as an Intracanal Medicament on the Chemical Structure of Radicular Dentine
Mewan Abdulrahman, Bestoon Faraj, Kawa Dizaye
Sulaimani Dental Journal.2021; 8(2): 8. CrossRef - Local Drug Delivery Systems for Vital Pulp Therapy: A New Hope
Ardavan Parhizkar, Saeed Asgary, Carlo Galli
International Journal of Biomaterials.2021; 2021: 1. CrossRef - Antibiofilm and cytotoxic effect of 3,3′-dihydroxycurcumin (DHC) as photosensitizer agent in antimicrobial photodynamic therapy for endodontic purposes
Jesse Augusto Pereira, Carlos Roberto Polaquini, VanessaRodrigues dos Santos, Karina Sampaio Caiaffa, Rafaela Laruzo Rabelo, Reinaldo dos Santos Theodoro, Letícia Helena Theodoro, Luis Octavio Regasini, Cristiane Duque
Photodiagnosis and Photodynamic Therapy.2021; 36: 102534. CrossRef - An in-vitro Comparative Evaluation of Quantitative Release of Transforming Growth Factor β-1 from Dentin upon the Action of Endodontic Irrigants, Medicaments, Ultrasonic Activation, and Low-Level Laser Irradiation
Anilkumar Akhila, V. P. Prabath Singh, Kerala R. Varma, Senthil V. Vasudevan, V. Sukhithasri, Salu Sasikumar
Amrita Journal of Medicine.2021; 17(2): 34. CrossRef - Effect of triple antibiotic paste and calcium hydroxide on the rate of healing of periapical lesions: A systematic review
NKiran Kumar, Biji Brigit, BS Annapoorna, SavithaB Naik, Seema Merwade, K Rashmi
Journal of Conservative Dentistry.2021; 24(4): 307. CrossRef - Comparison of the efficacy of CanalBrush, EndoActivator, and Passive Ultrasonic Irrigation on the removal of triple antibiotic paste from root canal walls: An in vitro study
Santosh Kumar, Kavisha Desai, Aparna Palekar, Baswaraj Biradar, Ananjan Chatterjee, Khushboo Kumari
Journal of International Society of Preventive and Community Dentistry.2020; 10(4): 424. CrossRef - Apexification with Calcium Hydroxide vs. Revascularization
H. Boufdil, M. Mtalsi, S. El Arabi, B. Bousfiha, Jose López-López
Case Reports in Dentistry.2020;[Epub] CrossRef - Effect of Intracanal Medicaments and Irrigants on the Release of Transforming Growth Factor Beta 1 and Vascular Endothelial Growth Factor from Cervical Root Dentin
Lívia Nazareth Ferreira, Regina Maria Puppin-Rontani, Fernanda Miori Pascon
Journal of Endodontics.2020; 46(11): 1616. CrossRef - Incorporation of amoxicillin-loaded microspheres in mineral trioxide aggregate cement: an in vitro study
Fábio Rocha Bohns, Vicente Castelo Branco Leitune, Isadora Martini Garcia, Bruna Genari, Nélio Bairros Dornelles, Silvia Stanisçuaski Guterres, Fabrício Aulo Ogliari, Mary Anne Sampaio de Melo, Fabrício Mezzomo Collares
Restorative Dentistry & Endodontics.2020;[Epub] CrossRef - Assessment of Nitrofurantoin as an Experimental Intracanal Medicament in Endodontics
Mewan Salahalddin A. Alrahman, Bestoon Muhammed Faraj, Kawa F. Dizaye, Abdelwahab Omri
BioMed Research International.2020;[Epub] CrossRef - An in vitro assessment of effect on microhardness of dentin using vicker's hardness method
Manoj Chandak, Richa Modi, Rakesh Gogiya, Rakhi Chandak, Anuja Ikhar, Nikhil Mankar
Journal of Datta Meghe Institute of Medical Sciences University.2020; 15(2): 251. CrossRef - Inspection of the Microbiota in Endodontic Lesions
Mario Dioguardi, Giovanni Di Gioia, Gaetano Illuzzi, Claudia Arena, Vito Carlo Alberto Caponio, Giorgia Apollonia Caloro, Khrystyna Zhurakivska, Iolanda Adipietro, Giuseppe Troiano, Lorenzo Lo Muzio
Dentistry Journal.2019; 7(2): 47. CrossRef - Materials for pulpotomy in immature permanent teeth: a systematic review and meta-analysis
Yuan Chen, Xinlei Chen, Yali Zhang, Fangjie Zhou, Jiaxin Deng, Jing Zou, Yan Wang
BMC Oral Health.2019;[Epub] CrossRef - Adjunctive antimicrobial photodynamic therapy to conventional chemo-mechanical debridement of infected root canal systems: A systematic review and meta-analysis
Maryam Pourhajibagher, Abbas bahador
Photodiagnosis and Photodynamic Therapy.2019; 26: 19. CrossRef - Comparison of Antibacterial Effects of Photodynamic Therapy, Modified Triple Antibiotic Paste and Calcium Hydroxide on Root Canals Infected With Enterococcus faecalis: An In Vitro Study
Mohammad Asnaashari, Mohammad Jafar Eghbal, Amirali Sahba Yaghmayi, Mehdi Shokri, Saranaz Azari-Marhabi
Journal of Lasers in Medical Sciences.2019; 10(5): S23. CrossRef
-
12,195
View
-
140
Download
-
71
Crossref
-
Periodontal healing following non-surgical repair of an old perforation with pocket formation and oral communication
-
Saeed Asgary, Prashant Verma, Ali Nosrat
-
Restor Dent Endod 2018;43(2):e17. Published online April 13, 2018
-
DOI: https://doi.org/10.5395/rde.2018.43.e17
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
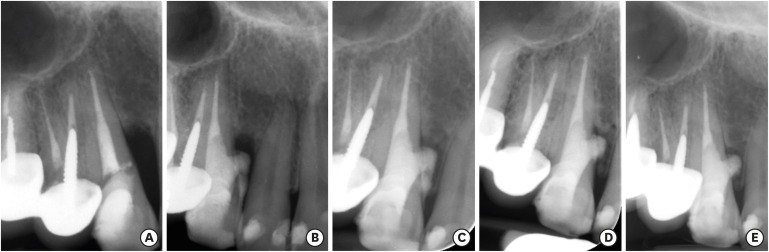
Iatrogenic perforations negatively impact the outcome of endodontic treatments. Studies on prognostic factors showed that perforations in the coronal third of the root with periodontal pocket formation have an unfavorable prognosis. A 36-year-old female was referred for endodontic evaluation of tooth #13 with a history of an iatrogenic perforation, happened 3 years ago. There was a sinus tract associated with perforation, 10 mm probing on the mesial and mesio-palatal, bleeding on probing, radiolucent lesion adjacent to the perforation and complete resorption of the interdental bone between teeth #13 and #12. After the treatment options were discussed, she chose to save the tooth. The tooth was accessed under rubber dam isolation, the perforation site was cleaned and disinfected using 0.5% sodium hypochlorite and sealed with calcium-enriched mixture cement. Eighteen months after treatment the tooth was functional and asymptomatic. The probing depths were normal without bleeding on probing. Radiographically, the interdental crestal bone formed between teeth #13 and #12. Despite all negative prognostic factors in this case (i.e., perforations in the coronal third, pocket formation, and radiolucent lesion), healing was unexpectedly achieved via non-surgical repair of the perforation. Further research on biological aspects of healing in the periodontium following iatrogenic perforations are recommended. -
Citations
Citations to this article as recorded by  - Managing Internal Inflammatory Root Resorption and Perforation of a Mandibular Primary Molar: A Case Report With 15 Months Follow‐Up
Mana Mowji, Motahareh Khosrojerdi
Clinical Case Reports.2025;[Epub] CrossRef - Nonsurgical Management of Furcation Defects Using Cervical Sealing With Calcium–Silicate Cements: A Clinical Case Series
Saeed Asgary, Shamimul Hasan
Case Reports in Medicine.2025;[Epub] CrossRef - Nonsurgical Management of Simultaneous Double Lateral Root Perforations in Adjacent Teeth Using CBCT and MTA: A Case Report
Beyhan Başkan, Hatice Kübra Başkan, Beyza Güler, Ricardo Faria Ribeiro
Case Reports in Dentistry.2025;[Epub] CrossRef - Comprehensive review of composition, properties, clinical applications, and future perspectives of calcium-enriched mixture (CEM) cement: a systematic analysis
Saeed Asgary, Mahtab Aram, Mahta Fazlyab
BioMedical Engineering OnLine.2024;[Epub] CrossRef - External Cervical Resorption: A Volumetric Analysis on Evolution of Defects over Time
Ali Nosrat, Omid Dianat, Prashant Verma, Martin D. Levin, Jeffery B. Price, Anita Aminoshariae, Fabio Antonio Piola Rizzante
Journal of Endodontics.2023; 49(1): 36. CrossRef - Comparative evaluation of mineral trioxide aggregate, endoseal, and biodentine in furcation perforation repair
Udita Khare Baralay, Srinidhi Surya Raghavendra
Endodontology.2022; 34(1): 22. CrossRef - Calcium Silicate Cements Application in Lateral Root Perforation Repair: A Case Report with 16-Month Follow-Up
Juan G. Robledo, Pablo A. Rodríguez
Open Journal of Stomatology.2021; 11(08): 317. CrossRef - Vital Pulp Therapy as a Conservative Approach for Management of Invasive Cervical Root Resorption: A Case Series
Saeed Asgary, Mahdieh Nourzadeh, Prashant Verma, M. Lamar Hicks, Ali Nosrat
Journal of Endodontics.2019; 45(9): 1161. CrossRef
-
2,239
View
-
12
Download
-
8
Crossref
-
Management of failed periodontal surgical intervention for a furcal lesion with a nonsurgical endodontic approach
-
Saeed Asgary, Mahta Fazlyab
-
Restor Dent Endod 2014;39(2):115-119. Published online March 21, 2014
-
DOI: https://doi.org/10.5395/rde.2014.39.2.115
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
As long as the prognosis of teeth remains a matter of concern, the endodontic-periodontal relationship will be considered a challenge for the clinician. Many etiologic factors, including bacteria, fungi, and viruses, plus other contributing factors, such as trauma, root resorptions/perforations, and dental malformations, play a role in the co-occurrence of endodontic and periodontal lesions. Whatever the cause, a correct diagnosis on which to base the treatment plan is the key to successful maintenance of the tooth. This article reports the successful endodontic management of a furcation lesion in a mandibular molar that was nonresponsive to a previous periodontal surgical graft. The case had presented a diagnostic challenge for the clinicians, and this article reviews the key points that can lead to a correct diagnosis and treatment planning. -
Citations
Citations to this article as recorded by  - Acute periodontal lesions (periodontal abscesses and necrotizing periodontal diseases) and endo‐periodontal lesions
David Herrera, Belén Retamal‐Valdes, Bettina Alonso, Magda Feres
Journal of Clinical Periodontology.2018;[Epub] CrossRef - Acute periodontal lesions (periodontal abscesses and necrotizing periodontal diseases) and endo‐periodontal lesions
David Herrera, Belén Retamal‐Valdes, Bettina Alonso, Magda Feres
Journal of Periodontology.2018;[Epub] CrossRef - The importance of correct diagnosis and treatment in endo-periodontal lesions: a two cases comparison
Sara Bernardi, Christian Frascarelli, Giulia Fantozzi, Silvia Caruso, Robert Gatto, Gianna Maria Nardi, Maria Adelaide Continenza
Dental Update.2016; 43(8): 766. CrossRef
-
2,294
View
-
11
Download
-
3
Crossref
-
Surgical management of a failed internal root resorption treatment: a histological and clinical report
-
Saeed Asgary, Mohammad Jafar Eghbal, Leili Mehrdad, Sanam Kheirieh, Ali Nosrat
-
Restor Dent Endod 2014;39(2):137-142. Published online March 21, 2014
-
DOI: https://doi.org/10.5395/rde.2014.39.2.137
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
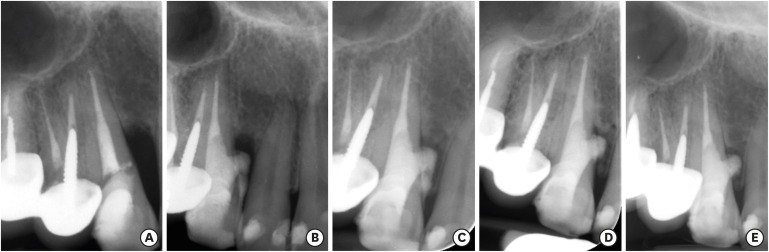
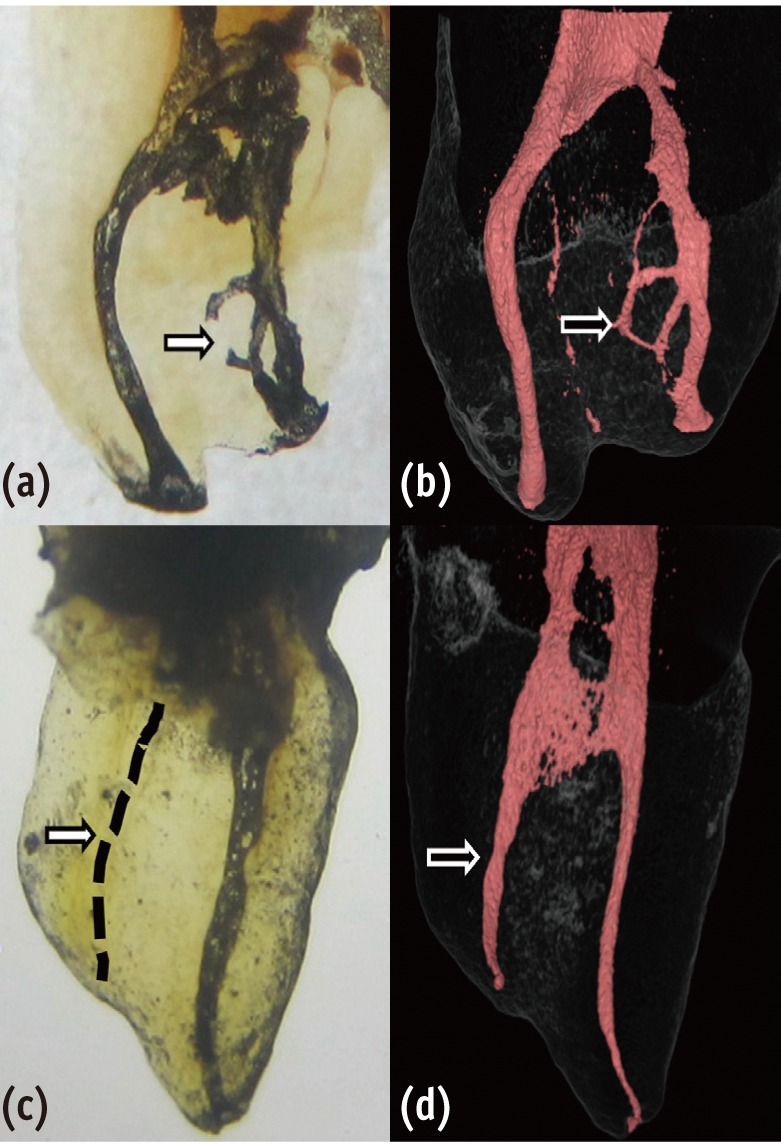
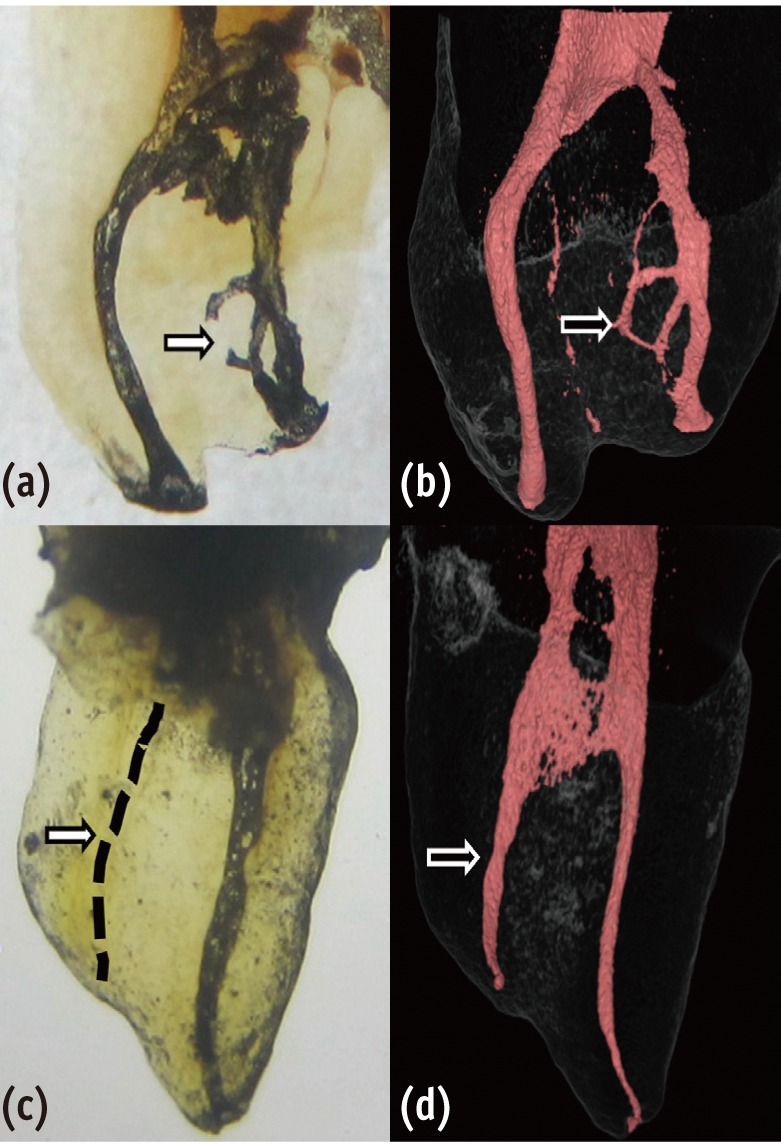
This article presents the successful surgical management of a failed mineral trioxide aggregate (MTA) orthograde obturation of a tooth with a history of impact trauma and perforated internal root resorption. A symptomatic maxillary lateral incisor with a history of perforation due to internal root resorption and nonsurgical repair using MTA was referred. Unintentional overfill of the defect with MTA had occurred 4 yr before the initial visit. The excess MTA had since disappeared, and a radiolucent lesion adjacent to the perforation site was evident radiographically. Surgical endodontic retreatment was performed using calcium enriched mixture (CEM) cement as a repair material. Histological examination of the lesion revealed granulation tissue with chronic inflammation, and small fragments of MTA encapsulated within fibroconnective tissue. At the one and two year follow up exams, all signs and symptoms of disease had resolved and the tooth was functional. Complete radiographic healing of the lesion was observed two years after the initial visit. This case report illustrates how the selection of an appropriate approach to treatment of a perforation can affect the long term prognosis of a tooth. In addition, extrusion of MTA into a periradicular lesion should be avoided. -
Citations
Citations to this article as recorded by  - Managing Internal Inflammatory Root Resorption and Perforation of a Mandibular Primary Molar: A Case Report With 15 Months Follow‐Up
Mana Mowji, Motahareh Khosrojerdi
Clinical Case Reports.2025;[Epub] CrossRef - Endodontic management of internal replacement resorption of two maxillary central incisors with the aid of cone-beam computed tomography as the diagnostic tool: a case report and review of literature
Fatemeh Eskandari, Safoora Sahebi, Negar Ghorbani Jahandizi, Hossein Mofidi
Journal of Medical Case Reports.2025;[Epub] CrossRef - Removal of AH Plus Bioceramic Sealer from Artificial Internal Resorption Cavities Using Different Irrigation Activation Systems
Mine Büker, Meltem Sümbüllü, Emine Şimşek, Fadime Sena Sezer
Cumhuriyet Dental Journal.2025; 28(3): 383. CrossRef - Comprehensive review of composition, properties, clinical applications, and future perspectives of calcium-enriched mixture (CEM) cement: a systematic analysis
Saeed Asgary, Mahtab Aram, Mahta Fazlyab
BioMedical Engineering OnLine.2024;[Epub] CrossRef - The various forms of tooth resorption
Jordan Samuel Blum
Australian Endodontic Journal.2024; 50(2): 191. CrossRef - Bioceramics in Endodontics: Updates and Future Perspectives
Xu Dong, Xin Xu
Bioengineering.2023; 10(3): 354. CrossRef - Imaging techniques and various treatment modalities used in the management of internal root resorption: A systematic review
R. S Digholkar, S D Aggarwal, P S Kurtarkar, P. B Dhatavkar, V L Neil, D N Agarwal
Endodontology.2023; 35(2): 85. CrossRef - Treatment of Teeth with Root Resorptions: A Case Report and Systematic Review
Damla Erkal, Abdullah Başoğlu, Damla Kırıcı, Nezahat Arzu Kayar, Simay Koç, Kürşat Er
Galician Medical Journal.2023;[Epub] CrossRef - Effects of calcium silicate cements on neuronal conductivity
Derya Deniz-Sungur, Mehmet Ali Onur, Esin Akbay, Gamze Tan, Fügen Daglı-Comert, Taner Cem Sayın
Restorative Dentistry & Endodontics.2022;[Epub] CrossRef - Mineral trioxide aggregate and other bioactive endodontic cements: an updated overview – part II: other clinical applications and complications
M. Torabinejad, M. Parirokh, P. M. H. Dummer
International Endodontic Journal.2018; 51(3): 284. CrossRef - Periodontal healing following non-surgical repair of an old perforation with pocket formation and oral communication
Saeed Asgary, Prashant Verma, Ali Nosrat
Restorative Dentistry & Endodontics.2018;[Epub] CrossRef - Conservative Management of Class 4 Invasive Cervical Root Resorption Using Calcium-enriched Mixture Cement
Saeed Asgary, Ali Nosrat
Journal of Endodontics.2016; 42(8): 1291. CrossRef - Importance of CBCT in the management plan of upper canine with internal resorption
Roberto Fornara, Dario Re Cecconi
Giornale Italiano di Endodonzia.2015; 29(2): 70. CrossRef
-
1,604
View
-
10
Download
-
13
Crossref
-
A preliminary report on histological outcome of pulpotomy with endodontic biomaterials vs calcium hydroxide
-
Ali Nosrat, Ali Peimani, Saeed Asgary
-
Restor Dent Endod 2013;38(4):227-233. Published online November 12, 2013
-
DOI: https://doi.org/10.5395/rde.2013.38.4.227
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Objectives
The purpose of the study was to evaluate human dental pulp response to pulpotomy with calcium hydroxide (CH), mineral trioxide aggregate (MTA), and calcium enriched mixture (CEM) cement. Materials and MethodsA total of nine erupted third molars were randomly assigned to each pulpotomy group. The same clinician performed full pulpotomies and coronal restorations. The patients were followed clinically for six months; the teeth were then extracted and prepared for histological assessments. The samples were blindly assessed by an independent observer for pulp vitality, pulp inflammation, and calcified bridge formation. ResultsAll patients were free of clinical signs/symptoms of pulpal/periradicular diseases during the follow up period. In CH group, one tooth had necrotic radicular pulp; other two teeth in this group had vital uninflamed pulps with complete dentinal bridge formation. In CEM cement and MTA groups all teeth had vital uninflamed radicular pulps. A complete dentinal bridge was formed beneath CEM cement and MTA in all roots. Odontoblast-like cells were present beneath CEM cement and MTA in all samples. ConclusionsThis study revealed that CEM cement and MTA were reliable endodontic biomaterials in full pulpotomy treatment. In contrast, the human dental pulp response to CH might be unpredictable.
-
Citations
Citations to this article as recorded by  - A meta‐analysis of calcium silicate‐based cements and calcium hydroxide as promoters of hard tissue bridge formation
Emmanuel J. N. L. Silva, Karem P. Pinto, Fernanda N. S. J. Riche, Maristela G. H. Carestiato, Jorge N. R. Martins, Henry F. Duncan, Marco A. Versiani, Gustavo De‐Deus
International Endodontic Journal.2025; 58(5): 685. CrossRef - Clinical and radiographic outcomes of pulpotomy materials in permanent teeth: a systematic review of calcium hydroxide, MTA, biodentine, and iRoot BP plus
Anggi Putri Riandani, Arief Cahyanto, Rana Abdelbaset Lotfy Diab, Ratih Widyasari, Atia Nurul Sidiqa, Hendra Dian Adhita Dharsono, Myrna Nurlatifah Zakaria
BMC Oral Health.2025;[Epub] CrossRef - Comprehensive review of composition, properties, clinical applications, and future perspectives of calcium-enriched mixture (CEM) cement: a systematic analysis
Saeed Asgary, Mahtab Aram, Mahta Fazlyab
BioMedical Engineering OnLine.2024;[Epub] CrossRef - Hard tissue formation in pulpotomized primary teeth in dogs with nanomaterials MCM-48 and MCM-48/hydroxyapatite: an in vivo animal study
Sahar Talebi, Nosrat Nourbakhsh, Ardeshir Talebi, Amir Abbas Nourbakhsh, Abbas Haghighat, Maziar Manshayi, Hamid Reza Bakhsheshi, Razieh Karimi, Rahman Nazeri, Kenneth J.D. Mackenzie
BMC Oral Health.2024;[Epub] CrossRef - The Role of Growth Factor Delivery Systems on Cellular Activities of Dental
Stem Cells: A Systematic Review (Part II)
Sayna Shamszadeh, Armin Shirvani, Saeed Asgary
Current Stem Cell Research & Therapy.2024; 19(4): 587. CrossRef - Calcium Silicate-Based Cements in Restorative Dentistry: Vital Pulp Therapy Clinical, Radiographic, and Histological Outcomes on Deciduous and Permanent Dentition—A Systematic Review and Meta-Analysis
Maria Teresa Xavier, Ana Luísa Costa, João Carlos Ramos, João Caramês, Duarte Marques, Jorge N. R. Martins
Materials.2024; 17(17): 4264. CrossRef - Pulpotomy: An alternative treatment modality to conventional root canal treatment
Günther Streit, Martin Vorster, Peet J Van der Vyver
South African Dental Journal.2023; 78(06): 309. CrossRef - A Comparative Histological Analysis of Human Pulp Following Direct Pulp Capping with Propolis or Biodentine
Nehad A Ahmad, Nevin A. Gad, Marwa H. Abdulmonaem
Journal of Nature and Science of Medicine.2022; 5(3): 281. CrossRef - Expression of Matrix Metalloproteinases-8 and Myeloperoxidase in Pulp Tissue after Pulpotomy with Calcium Silicate Cements
Nayara Nery de Oliveira Cunha, Marina Azevedo Junqueira, Leopoldo Cosme-Silva, Laís da Silveira Terra Santos, George Augusto Veloso de Oliveira, Rafael Tobias Moretti Neto, Denismar Alves Nogueira, Maísa Ribeiro Pereira Lima Brigagão, Ana Beatriz da Silve
Pesquisa Brasileira em Odontopediatria e Clínica Integrada.2021;[Epub] CrossRef - Long-term Outcomes of Full Pulpotomy in Permanent Molars for Patients Treated in a Single, Short Session under Special Conditions
Natacha Linas, Nicolas Decerle, Marie-Laure Munoz-Sanchez, Denise Faulks, Valérie Collado, Emmanuel Nicolas, Martine Hennequin, Pierre-Yves Cousson
Journal of Endodontics.2020; 46(11): 1597. CrossRef - Quantitative Assessment of Root Development after Regenerative Endodontic Therapy: A Systematic Review and Meta-Analysis
Teng Kai Ong, Ghee Seong Lim, Maharaj Singh, Alissa V. Fial
Journal of Endodontics.2020; 46(12): 1856. CrossRef - Dexamethasone- loaded polymeric porous sponge as a direct pulp capping agent
Amjad Alagha, Abdulwahab Nourallah, Sahar Alhariri
Journal of Biomaterials Science, Polymer Edition.2020; 31(13): 1689. CrossRef - Postendodontic Pain after Pulpotomy or Root Canal Treatment in Mature Teeth with Carious Pulp Exposure: A Multicenter Randomized Controlled Trial
Mohammad Jafar Eghbal, Ali Haeri, Arash Shahravan, Ali Kazemi, Fariborz Moazami, Mohammad Ali Mozayeni, Eshaghali Saberi, Mohammad Samiei, Mehdi Vatanpour, Alireza Akbarzade Baghban, Mahta Fazlyab, Ardavan Parhizkar, Mahboobe Ahmadi, Nazila Akbarian Rad,
Pain Research and Management.2020; 2020: 1. CrossRef - Vital Pulp Therapy as a Conservative Approach for Management of Invasive Cervical Root Resorption: A Case Series
Saeed Asgary, Mahdieh Nourzadeh, Prashant Verma, M. Lamar Hicks, Ali Nosrat
Journal of Endodontics.2019; 45(9): 1161. CrossRef - Which procedures and materials could be applied for full pulpotomy in permanent mature teeth? A systematic review
M. Zanini, M. Hennequin, PY. Cousson
Acta Odontologica Scandinavica.2019; 77(7): 541. CrossRef - Periodontal healing following non-surgical repair of an old perforation with pocket formation and oral communication
Saeed Asgary, Prashant Verma, Ali Nosrat
Restorative Dentistry & Endodontics.2018;[Epub] CrossRef - Mineral trioxide aggregate and other bioactive endodontic cements: an updated overview – part I: vital pulp therapy
M. Parirokh, M. Torabinejad, P. M. H. Dummer
International Endodontic Journal.2018; 51(2): 177. CrossRef - Treatment Outcomes of 4 Vital Pulp Therapies in Mature Molars
Saeed Asgary, Raheleh Hassanizadeh, Hassan Torabzadeh, Mohammad Jafar Eghbal
Journal of Endodontics.2018; 44(4): 529. CrossRef - A Review of Criteria for the Evaluation of Pulpotomy Outcomes in Mature Permanent Teeth
Marjorie Zanini, Martine Hennequin, Pierre-Yves Cousson
Journal of Endodontics.2016; 42(8): 1167. CrossRef - Calcium-Enriched Mixture Pulpotomy of Primary Molar Teeth with Irreversible Pulpitis. A Clinical Study
Mahtab Memarpour, Soleiman Fijan, Saeed Asgary, Marzieh Keikhaee
The Open Dentistry Journal.2016; 10(1): 43. CrossRef - Endodontie in der unreifen bleibenden Dentition — Maßnahmen zur Vitalerhaltung, Apexifikation und Regeneration der Pulpa
Martin Jung
Oralprophylaxe & Kinderzahnheilkunde.2016; 38(1): 29. CrossRef - Conservative Management of Class 4 Invasive Cervical Root Resorption Using Calcium-enriched Mixture Cement
Saeed Asgary, Ali Nosrat
Journal of Endodontics.2016; 42(8): 1291. CrossRef - Permanent teeth pulpotomy survival analysis: retrospective follow-up
Gustavo Golgo Kunert, Itaborai Revoredo Kunert, Luiz Cesar da Costa Filho, José Antônio Poli de Figueiredo
Journal of Dentistry.2015; 43(9): 1125. CrossRef - Cytocompatibility and Antibacterial Properties of Capping Materials
Claudio Poggio, Carla Renata Arciola, Riccardo Beltrami, Annachiara Monaco, Alberto Dagna, Marco Lombardini, Livia Visai
The Scientific World Journal.2014; 2014: 1. CrossRef - Surgical management of a failed internal root resorption treatment: a histological and clinical report
Saeed Asgary, Mohammad Jafar Eghbal, Leili Mehrdad, Sanam Kheirieh, Ali Nosrat
Restorative Dentistry & Endodontics.2014; 39(2): 137. CrossRef - Effect of Mineral Trioxide Aggregate Surface Treatments on Morphology and Bond Strength to Composite Resin
Joo-Hee Shin, Ji-Hyun Jang, Sang Hyuk Park, Euiseong Kim
Journal of Endodontics.2014; 40(8): 1210. CrossRef
-
1,473
View
-
6
Download
-
26
Crossref
-
Necrosis of intact premolar caused by an adjacent apical infection: a case report
-
Saeed Asgary, Laleh Alim Marvasti
-
Restor Dent Endod 2013;38(2):90-92. Published online May 28, 2013
-
DOI: https://doi.org/10.5395/rde.2013.38.2.90
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
Although periapical inflammatory lesions are usually resulted by infection in the root canal system, this rare case showed that a periapical lesion related to an infected tooth may cause pulpal necrosis in adjacent intact tooth, with no history or clinical signs of caries, disease, trauma or developmental anomaly. This case also suggests that the periapical lesion can be treated conservatively, without surgical intervention. Furthermore, this case highlights the importance of prompt treatment of apical periodontitis before the lesion becomes extensive as well as follows up of large lesions. -
Citations
Citations to this article as recorded by  - Accidentally Extruded Calcium Hydroxide Into a Cystic Lesion Associated With an Adjacent Tooth—A Case Report
Emmanuel Mazinis, Nikolaos Tsanidis, Vasilios Thomaidis
Clinical Case Reports.2025;[Epub] CrossRef - Atypically grown large periradicular cyst affecting adjacent teeth and leading to confounding diagnosis of non‐endodontic pathology
Domenico Ricucci, Massimiliano Amantea, Christian Girone, José F. Siqueira
Australian Endodontic Journal.2020; 46(2): 272. CrossRef
-
1,797
View
-
16
Download
-
2
Crossref
|