-
Coronal tooth discoloration induced by regenerative endodontic treatment using different scaffolds and intracanal coronal barriers: a 6-month ex vivo study
-
Noushin Shokouhinejad, Hassan Razmi, Maryam Farbod, Marzieh Alikhasi, Josette Camilleri
-
Restor Dent Endod 2019;44(3):e25. Published online July 16, 2019
-
DOI: https://doi.org/10.5395/rde.2019.44.e25
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Objective
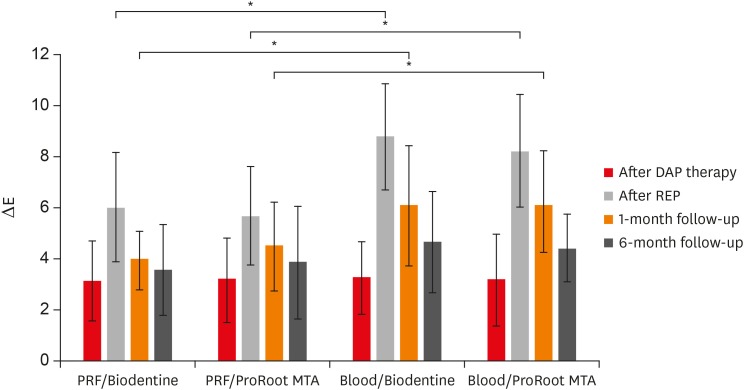
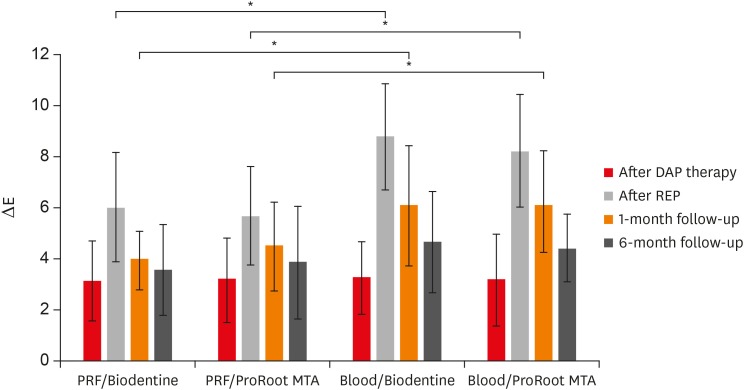
The aim of this study was to evaluate discoloration of teeth undergoing regenerative endodontic procedures (REPs) using blood clot or platelet-rich fibrin (PRF) as the scaffolds and different calcium silicate-based materials as the intracanal coronal barriers in an ex vivo model. Materials and MethodsForty-eight bovine incisors were prepared and disinfected using 1 mg/mL double antibiotic paste (DAP). The specimens were then randomly divided into 2 groups (n = 24) according to the scaffolds (blood or PRF). After placement of scaffolds each group was divided into 2 subgroups (n = 12) according to the intracanal coronal barriers (ProRoot MTA or Biodentine). The pulp chamber walls were sealed with dentin bonding agent before placement of DAP and before placement of scaffolds. The color changes (∆E) were measured at different steps. The data were analyzed using 2-way analysis of variance. ResultsCoronal discoloration induced by DAP was not clinically perceptible (ΔE ≤ 3.3). Regarding the type of the scaffold, coronal discoloration was significantly higher in blood groups compared with PRF groups at the end of REP and after 1 month (p < 0.05). However, no significant difference was found between PRF and blood clot after 6 months (p > 0.05). Considering the type of intracanal coronal barrier, no significant difference existed between ProRoot MTA and Biodentine (p > 0.05). ConclusionsWith sealing the dentinal tubules of pulp chamber with a dentin bonding agent and application of DAP as an intracanal medicament, coronal color change of the teeth following the use of PRF and blood sealed with either ProRoot MTA or Biodentine was not different at 6-month follow-up.
-
Citations
Citations to this article as recorded by  - Impact of Biodentine Placement on Fracture Resistance and its Influence on Discoloration with Different Scaffolds
Evren Sarıyılmaz, Öznur Sarıyılmaz, Burak Çarıkçıoğlu, Gülşah Uslu, Raif Alan
Journal of Endodontics.2025; 51(9): 1199. CrossRef - Effect of pH on the solubility and volumetric change of ready-to-use Bio-C Repair bioceramic material
Luana Raphael da SILVA, Jader Camilo PINTO, Juliane Maria GUERREIRO-TANOMARU, Mário TANOMARU-FILHO
Brazilian Oral Research.2024;[Epub] CrossRef - Efficacy of Potassium Iodide and Glutathione for Correlation of Dentin Discoloration Caused by Silver Diamine Fluoride
Mahsa Samani, Hamid Majzoub, Faramarz Zakavi, Ayyub Mojaddami
Cureus.2024;[Epub] CrossRef - Intracanal medicaments and coronal sealing materials influence on root fracture resistance and coronal discoloration: An in vitro study
Rasoul Sahebalam, Marzie Boskabady, Maryam Naghavi, Samira Dehghanitafti
Saudi Endodontic Journal.2024; 14(2): 199. CrossRef - Potential Crown Discoloration Induced by the Combination of Various Intracanal Medicaments and Scaffolds Applied in Regenerative Endodontic Therapy
NB Altun, A Turkyilmaz
Nigerian Journal of Clinical Practice.2024; 27(7): 897. CrossRef - Evaluation of the effectiveness of different treatment approaches in preventing coronal discoloration caused by regenerative endodontic treatment
Melis Oya Ateş, Zeliha Uğur Aydın
Clinical Oral Investigations.2023; 27(8): 4595. CrossRef - Evaluation of the Effectiveness of Laser‐Assisted Bleaching of the Teeth Discolored due to Regenerative Endodontic Treatment
Noushin Shokouhinejad, Mehrfam Khoshkhounejad, Fatemeh Hamidzadeh, Murilo Baena Lopes
International Journal of Dentistry.2022;[Epub] CrossRef - Effectiveness of Teeth Whitening after Regenerative Endodontics Procedures: An In Vitro Study
Irini Fagogeni, Joanna Metlerska, Tomasz Falgowski, Maciej Górski, Mariusz Lipski, Alicja Nowicka
Journal of Clinical Medicine.2022; 11(23): 7016. CrossRef - Microstructure and color stability of calcium silicate-based dental materials exposed to blood or platelet-rich fibrin
Noushin Shokouhinejad, Ibrahim Abu Tahun, Shima Saber Tahan, Fatemeh Mohandes, Mohammad H. Nekoofar, Paul M. H. Dummer
Clinical Oral Investigations.2022; 27(3): 1193. CrossRef - Spectrophotometric analysis of internal bleaching of traumatized teeth with coronal discoloration following regenerative endodontic procedures
Jaqueline Lazzari, Walbert Vieira, Vanessa Pecorari, Brenda Paula Figueiredo de Almeida Gomes, José Flávio Affonso de Almeida, Adriana De-Jesus-Soares
Brazilian Journal of Oral Sciences.2021;[Epub] CrossRef - Biological parameters, discolouration and radiopacity of calcium silicate‐based materials in a simulated model of partial pulpotomy
Lilian Vieira Oliveira, Gabriela Leite de Souza, Gisele Rodrigues da Silva, Thamara Eduarda Alves Magalhães, Gabrielle Alves Nunes Freitas, Ana Paula Turrioni, Gabriella Lopes de Rezende Barbosa, Camilla Christian Gomes Moura
International Endodontic Journal.2021; 54(11): 2133. CrossRef - Effect of hydrogel-based antibiotic intracanal medicaments on crown discoloration
Rayan B. Yaghmoor, Jeffrey A. Platt, Kenneth J. Spolnik, Tien Min Gabriel Chu, Ghaeth H. Yassen
Restorative Dentistry & Endodontics.2021;[Epub] CrossRef - The effect of different calcium silicate-based pulp capping materials on tooth discoloration: an in vitro study
Ahmad S. Al-Hiyasat, Dana M. Ahmad, Yousef S. Khader
BMC Oral Health.2021;[Epub] CrossRef - Knowledge, attitudes, and practices of undergraduate students concerning Regenerative Endodontics
Ligia B. da Silva, Mariana Gabriel, Márcia M. Marques, Fernanda C. Carrer, Flávia Gonçalves, Giovanna Sarra, Giovanna L. Carvalho, Ana Armas-Vega, Maria S. Moreira
Minerva Stomatologica.2020;[Epub] CrossRef - Coronal Discoloration Related to Bioceramic and Mineral Trioxide Aggregate Coronal Barrier in Non-vital Mature Teeth Undergoing Regenerative Endodontic Procedures
Mazen Doumani, Mohammad Yaman Seirawan, Kinda Layous, Mohammad Kinan Seirawan
World Journal of Dentistry.2020; 11(1): 52. CrossRef
-
1,631
View
-
22
Download
-
15
Crossref
-
Surface microhardness of three thicknesses of mineral trioxide aggregate in different setting conditions
-
Noushin Shokouhinejad, Leila Jafargholizadeh, Mehrfam Khoshkhounejad, Mohammad Hossein Nekoofar, Maryam Raoof
-
Restor Dent Endod 2014;39(4):253-257. Published online August 20, 2014
-
DOI: https://doi.org/10.5395/rde.2014.39.4.253
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
- Objectives
This study aimed to compare the surface microhardness of mineral trioxide aggregate (MTA) samples having different thicknesses and exposed to human blood from one side and with or without a moist cotton pellet on the other side. Materials and MethodsNinety cylindrical molds with three heights of 2, 4, and 6 mm were fabricated. In group 1 (dry condition), molds with heights of 2, 4, and 6 mm (10 molds of each) were filled with ProRoot MTA (Dentsply Tulsa Dental), and the upper surface of the material was not exposed to any additional moisture. In groups 2 and 3, a distilled water- or phosphate-buffered saline (PBS)-moistened cotton pellet was placed on the upper side of MTA, respectively. The lower side of the molds in all the groups was in contact with human blood-wetted foams. After 4 day, the Vickers microhardness of the upper surface of MTA was measured. ResultsIn the dry condition, the 4 and 6 mm-thick MTA samples showed significantly lower microhardness than the 2 mm-thick samples (p = 0.003 and p = 0.001, respectively). However, when a distilled water- or PBS-moistened cotton pellet was placed over the MTA, no significant difference was found between the surface microhardness of samples having the abovementioned three thicknesses of the material (p = 0.210 and p = 0.112, respectively). ConclusionsIt could be concluded that a moist cotton pellet must be placed over the 4 to 6 mm-thick MTA for better hydration of the material. However, this might not be necessary when 2 mm-thick MTA is used.
-
Citations
Citations to this article as recorded by  - Evaluation of the Effects of Different Irrigation Solutions on MTA and Dentin Microhardness
Gokay Buyukcolpan, İdil Özden, Hesna Sazak Öveçoğlu
Clinical and Experimental Health Sciences.2025; 15(3): 524. CrossRef - Retrograde Versus Orthograde Obturation in Relation to Root Resection: Evaluation of Microhardness of Mineral Trioxide Aggregate In Vitro
Lukas Stundžia, Rita Vėberienė, Indrė Graunaitė, Aurelijus Domeika, Neringa Skučaitė, Cesar Rogério Pucci
International Journal of Dentistry.2025;[Epub] CrossRef - MTA as modulator of periapical tissue healing in rat molar: A histological study
Christian Khoswanto, Ira Kusuma Dewi
Journal of Oral Biology and Craniofacial Research.2024; 14(2): 201. CrossRef - An Update on Endodontic Microsurgery of Mandibular Molars: A Focused Review
Sun Mi Jang, Euiseong Kim, Kyung-San Min
Medicina.2021; 57(3): 270. CrossRef - Assessment of Mineral Trioxide Aggregate Setting in Simulated Root Canal with Different Root Canal Wall Thickness: In Vitro Study
Radovan Žižka, Radim Čtvrtlík, Jan Tomáštík, Kamila Fačevicová, Ondřej Vencálek, Jiří Šedý, David Marinčák
Applied Sciences.2021; 11(4): 1727. CrossRef - Evaluation of the bioactivity of fluoride‐enriched mineral trioxide aggregate on osteoblasts
S. Proksch, J. Brossart, K. Vach, E. Hellwig, M. J. Altenburger, L. Karygianni
International Endodontic Journal.2018; 51(8): 912. CrossRef - Antimicrobial and antibiofilm activities of MTA supplemented with bismuth lipophilic nanoparticles
Rene HERNANDEZ-DELGADILLO, Casiano DEL ANGEL-MOSQUEDA, Juan Manuel SOLÍS-SOTO, Silvia MUNGUIA-MORENO, Nayely PINEDA-AGUILAR, Rosa Isela SÁNCHEZ-NÁJERA, Shankararaman CHELLAM, Claudio CABRAL-ROMERO
Dental Materials Journal.2017; 36(4): 503. CrossRef - Carbohydrate-electrolyte drinks exhibit risks for human enamel surface loss
Mary Anne Sampaio de Melo, Vanara Florêncio Passos, Juliana Paiva Marques Lima, Sérgio Lima Santiago, Lidiany Karla Azevedo Rodrigues
Restorative Dentistry & Endodontics.2016; 41(4): 246. CrossRef
-
1,150
View
-
7
Download
-
8
Crossref
|