-
Pulp revascularization with and without platelet-rich plasma in two anterior teeth with horizontal radicular fractures: a case report
-
Edison Arango-Gómez, Javier Laureano Nino-Barrera, Gustavo Nino, Freddy Jordan, Henry Sossa-Rojas
-
Restor Dent Endod 2019;44(4):e35. Published online August 20, 2019
-
DOI: https://doi.org/10.5395/rde.2019.44.e35
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
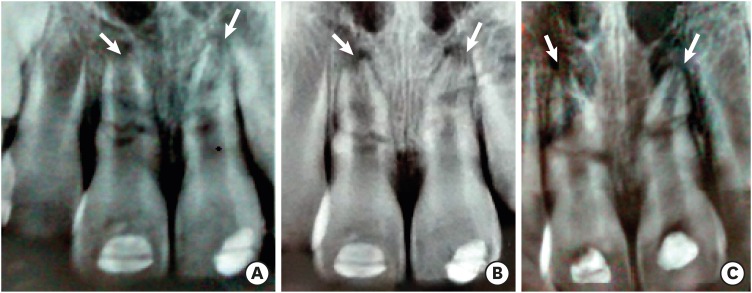
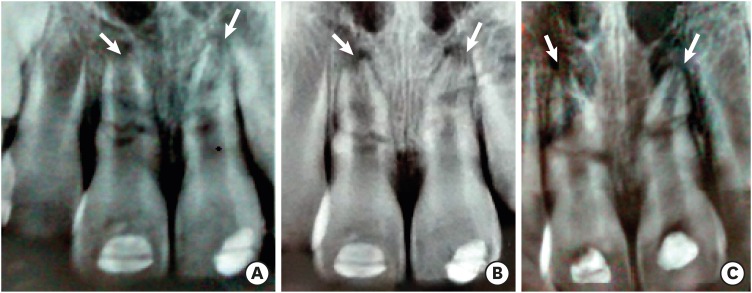
Pulp revascularization is an alternative treatment in immature traumatized teeth with necrotic pulp. However, this procedure has not been reported in horizontal root fractures. This is a case report of a 9-year-old patient with multiple horizontal root fractures in 2 upper central incisors that were successfully treated with pulp revascularization. The patient presented for treatment 2 years after the initial trauma, and revascularization was attempted after the initial treatment with calcium hydroxide had failed. Prior to pulp revascularization, cone-beam computed tomography and autoradiograms demonstrated multiple horizontal fractures in the middle and apical thirds of the roots of the 2 affected teeth. Revascularization was performed in both teeth; platelet-rich plasma (PRP) was used in one tooth (#11) and the conventional method (blood clot) was used in the other tooth (#21). Clinical and radiographic follow-up over 4 years demonstrated pulp calcification in the PRP-treated tooth. Neither of the 2 teeth were lost, and the root canal calcification of tooth #11 was greater than that of tooth #21. This case suggests that PRP-based pulp revascularization may be an alternative for horizontal root fractures. -
Citations
Citations to this article as recorded by  - Dental pulp mesenchymal stem cells-response to fibrin hydrogel reveals ITGA2 and MMPs expression
David Tong, Stéphanie Gobert, Alicia Reuzeau, Jean-Christophe Farges, Marianne Leveque, Marie Bolon, Arthur Costantini, Marielle Pasdeloup, Jérôme Lafont, Maxime Ducret, Mourad Bekhouche
Heliyon.2024; 10(13): e32891. CrossRef - Pulp regeneration treatment using different bioactive materials in permanent teeth of pediatric subjects
Dina Abdellatif, Alfredo Iandolo, Giuseppina De Benedetto, Francesco Giordano, Davide Mancino, Edouard Euvrard, Massimo Pisano
Journal of Conservative Dentistry and Endodontics.2024; 27(5): 458. CrossRef - Retreatment of a Failed Regenerative Endodontic Treatment in an Immature Tooth with a Horizontal Root Fracture: A Case Report
Zaher Marjy, Iris Slutzky-Goldberg
International Journal of Clinical Pediatric Dentistry.2024; 17(10): 1168. CrossRef - The Impact of the Preferred Reporting Items for Case Reports in Endodontics (PRICE) 2020 Guidelines on the Reporting of Endodontic Case Reports
Sofian Youssef, Phillip Tomson, Amir Reza Akbari, Natalie Archer, Fayjel Shah, Jasmeet Heran, Sunmeet Kandhari, Sandeep Pai, Shivakar Mehrotra, Joanna M Batt
Cureus.2023;[Epub] CrossRef - Evaluation of postoperative pain and healing following regenerative endodontics using platelet‐rich plasma versus conventional endodontic treatment in necrotic mature mandibular molars with chronic periapical periodontitis. A randomized clinical trial
Yassmin Elsayed Ahmed, Geraldine Mohamed Ahmed, Angie Galal Ghoneim
International Endodontic Journal.2023; 56(4): 404. CrossRef - Regenerative endodontic procedures for two traumatized mature anterior teeth with transverse root fractures
Jing Lu, Bill Kahler
BMC Oral Health.2022;[Epub] CrossRef - Are platelet concentrate scaffolds superior to traditional blood clot scaffolds in regeneration therapy of necrotic immature permanent teeth? A systematic review and meta-analysis
Qianwei Tang, Hua Jin, Song Lin, Long Ma, Tingyu Tian, Xiurong Qin
BMC Oral Health.2022;[Epub] CrossRef - Platelet-Rich Fibrin Used as a Scaffold in Pulp Regeneration: Case Series
Ceren ÇİMEN, Selin ŞEN, Elif ŞENAY, Tuğba BEZGİN
Cumhuriyet Dental Journal.2021; 24(1): 113. CrossRef - Plasma rico en plaquetas en Odontología: Revisión de la literatura
Hugo Anthony Rosas Rozas, Hugo Leoncio Rosas Cisneros
Yachay - Revista Científico Cultural.2021; 10(1): 536. CrossRef
-
338
View
-
5
Download
-
9
Crossref
-
Surgical management with intentional replantation on a tooth with palato-radicular groove
-
Jorge Forero-López, Luis Gamboa-Martínez, Laura Pico-Porras, Javier Laureano Niño-Barrera
-
Restor Dent Endod 2015;40(2):166-171. Published online December 22, 2014
-
DOI: https://doi.org/10.5395/rde.2015.40.2.166
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader ePub ePub
A palato-radicular groove (PRG) is a developmental anomaly primarily found in the maxillary lateral incisors. It is a potential communication path between the root canal and the periodontium that decreases the survival prognosis of the affected tooth, therefore compromising the stability of the dental structure in the oral cavity. The aim of this case report is to present an original technique where a PRG was treated by means of intracanal disinfection, PRG sealing with glass ionomer, replantation with intentional horizontal 180 degree rotation of the tooth, and an aesthetic veneer placed to provide adequate tooth morphology. The clinical and biological benefits of this novel technique are presented and discussed. -
Citations
Citations to this article as recorded by  - Diagnostic Approaches of Palatogingival Groove: A Systematic Review
Greta Venskutė
Journal of Dental Health and Oral Research.2024; : 1. CrossRef - Palatogingival Groove: A Plaque Trap Leading to Bone Loss in a Maxillary Lateral Incisor – A Rare Case Report
Gayathri Priyadharshini Elangovan, Indra Kumar Periyasamy, Saravana Kumar R, Gopinath Vivekanandhan
Dental Journal of Indira Gandhi Institute of Medical Sciences.2024; 3: 104. CrossRef - Palatogingival Groove: The Known–unknown Devourer
Sandeep Tandon, Rinku Mathur, Ambika S Rathore, Tripti S Rai, Kanchan Kumari Dhaker, Sumedha Gupta
International Journal of Clinical Pediatric Dentistry.2024; 17(S1): S95. CrossRef - Palatal groove associated with periodontal lesions: a systematic review illustrated by a decisional tree for management
Yvan Gaudex, Vianney Gandillot, Isabelle Fontanille, Philippe Bouchard, Stephane Kerner, Maria Clotilde Carra
BMC Oral Health.2024;[Epub] CrossRef - Prevalence of palatogingival groove affecting maxillary anterior teeth in Saudi subpopulation: A cone-beam computed tomographic study with literature review
Ali Ibrahim Aljuailan, Roqayah Aljuailan, Rahul N. Gaikwad, Shaul Hameed Kolarkodi, Nasser Rufaydan Alamri
The Saudi Dental Journal.2023; 35(8): 1039. CrossRef - Interdisciplinary approach for diagnosis and management of the tooth with type III palatogingival groove
Harakh Chand Baranwal, Jyoti Yadav
Saudi Endodontic Journal.2023; 13(2): 211. CrossRef - Management of Palatogingival Groove in Maxillary Lateral Incisor: A Report of a Rare Case With a Brief Review of Literature
Irfan Ansari, Sanjay Miglani, Vijay Yadav, Shamimul Hasan
Cureus.2023;[Epub] CrossRef - Intentional replantation combined root resection therapy for the treatment of type III radicular groove with two roots: A case report
Dan Tan, Shi-Ting Li, Hao Feng, Zhong-Chao Wang, Cai Wen, Min-Hai Nie
World Journal of Clinical Cases.2022; 10(20): 6991. CrossRef - The incidence of radicular groove on maxillary lateral incisors of Saudi population: CBCT evaluation
Sarah M. Alkahtany, Fatemah Alrwais, Asma Altamimi, Sundus M. Bukhary, Amani Mirdad
BMC Oral Health.2022;[Epub] CrossRef - Retrospective Study of Intentional Replantation for Type IIIb Dens Invaginatus with Periapical Lesions
Na Li, Huihui Xu, Cunhui Kan, Jing Zhang, Song Li
Journal of Endodontics.2022; 48(3): 329. CrossRef - Combined Periodontal and Endodontic Management of Palatal Radicular Groove with Platelet-Rich Fibrin and Biodentine®
Arjun Hari Rijal, Bhageshwar Dhami, Pratistha Ghimire, Konstantinos Michalakis
Case Reports in Dentistry.2022; 2022: 1. CrossRef - Intentional Replantation of Single-Rooted and Multi-Rooted Teeth: A Systematic Review
Massimo Pisano, Federica Di Spirito, Stefano Martina, Giuseppe Sangiovanni, Francesco D’Ambrosio, Alfredo Iandolo
Healthcare.2022; 11(1): 11. CrossRef - Management of the palato-radicular groove with a periodontal regenerative procedure and prosthodontic treatment: A case report
Dan-Hua Ling, Wei-Ping Shi, Yan-Hong Wang, Dan-Ping Lai, Yan-Zhen Zhang
World Journal of Clinical Cases.2022; 10(17): 5732. CrossRef - Prevalence and Periodontal Conditions of Developmental Grooves in an Italian School of Dentistry and Dental Hygiene: A Cross-Sectional Study
Giovanna Laura Di Domenico, Simone Fabrizi, Paolo Capparè, Maria Teresa Sberna, Massimo de Sanctis
International Journal of Environmental Research and Public Health.2022; 19(7): 4047. CrossRef - Clinical Observation and Research Progress of Comprehensive Treatment of Palatogingival Groove
华姣 胡
Advances in Clinical Medicine.2021; 11(03): 846. CrossRef - Palato-gingival groove: A silent nidus. Recognition and an innovative management approach: A report of 3 cases
Purushothama Rangaswamy, Sri Harsha Tummala, Samrat R Magarvalli, Sujith Ramachandra, Kavitha Govindappa, Shwetha E
IP Indian Journal of Conservative and Endodontics.2021; 6(2): 114. CrossRef - Periodontal Regenerative Treatment of Intrabony Defects Associated with Palatal Grooves: A Report of Two Cases
Stefano Corbella, Alice Alberti, Beatrice Zotti, Luca Francetti
Case Reports in Dentistry.2019; 2019: 1. CrossRef - Recognition and management of palatogingival groove for tooth survival: a literature review
Hee-Jin Kim, Yoorina Choi, Mi-Kyung Yu, Kwang-Won Lee, Kyung-San Min
Restorative Dentistry & Endodontics.2017; 42(2): 77. CrossRef - The use of Intentional Replantation to Repair an External Cervical Resorptive Lesion not am Enable to Conventional Surgical Repair
Kreena Pa Tel, Federico Foschi, Ioana Pop, Shanon Patel, Francesco Mannocci
Primary Dental Journal.2016; 5(2): 78. CrossRef - Management of apicomarginal defect in esthetic region associated with a tooth with anomalies
Vinayak Venkoosa Meharwade, Dipali Yogesh Shah, Pradyna Prabhakar Mali, Vidya Vinayak Meharwade
Restorative Dentistry & Endodontics.2015; 40(4): 314. CrossRef
-
249
View
-
4
Download
-
20
Crossref
|