Articles
- Page Path
- HOME > Restor Dent Endod > Volume 43(4); 2018 > Article
- Case Report Endodontic management of central incisor associated with large periapical lesion and fused supernumerary root: a conservative approach
-
Gautam P. Badole1
 , Pratima R. Shenoi1
, Pratima R. Shenoi1 , Ameya Parlikar2
, Ameya Parlikar2
-
Restor Dent Endod 2018;43(4):e44.
DOI: https://doi.org/10.5395/rde.2018.43.e44
Published online: October 26, 2018
1Department of Conservative Dentistry & Endodontics, VSPM's Dental College & Research Center, Nagpur, MH, India.
2Department of Conservative Dentistry & Endodontics, Rangoonwala Dental College and Research Center, Pune, MH, India.
- Correspondence to Gautam P. Badole, MDS. Reader, Department of Conservative Dentistry & Endodontics, VSPM's Dental College & Research Center, Hingna Road, Digdoh Hills, Nagpur, MH 440019, India. badole_g15@yahoo.co.in
Copyright © 2018. The Korean Academy of Conservative Dentistry
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 2,668 Views
- 23 Download
- 4 Crossref
Abstract
- Fusion and gemination are developmental anomalies of teeth that may require endodontic treatment. Fusion may cause various clinical problems related to esthetics, tooth spacing, and other periodontal complications. Additional diagnostic tools are required for the diagnosis and the treatment planning of fused tooth. The present case report describes a case of unilateral fusion of a supernumerary root to an upper permanent central incisor with large periapical lesion in which a conservative approach was used without extraction of supernumerary tooth and obturated with mineral trioxide aggregate to reach a favorable outcome.
INTRODUCTION
CASE REPORT
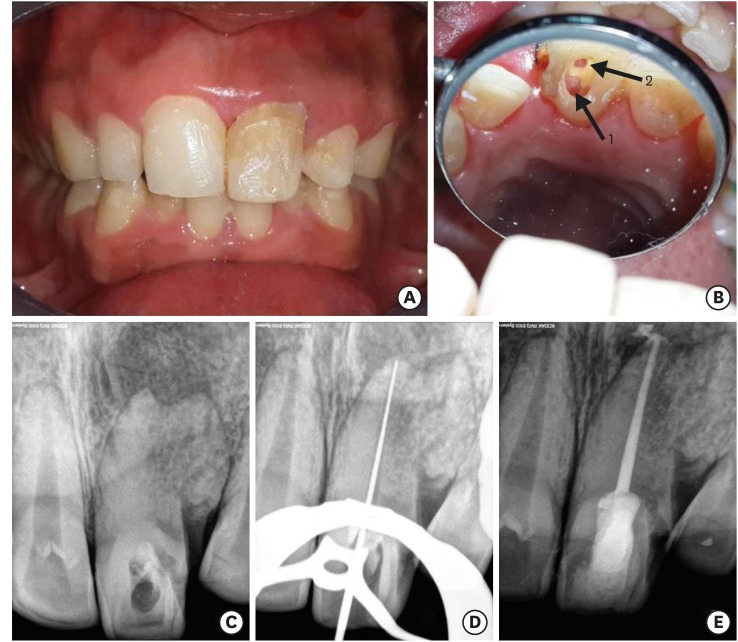
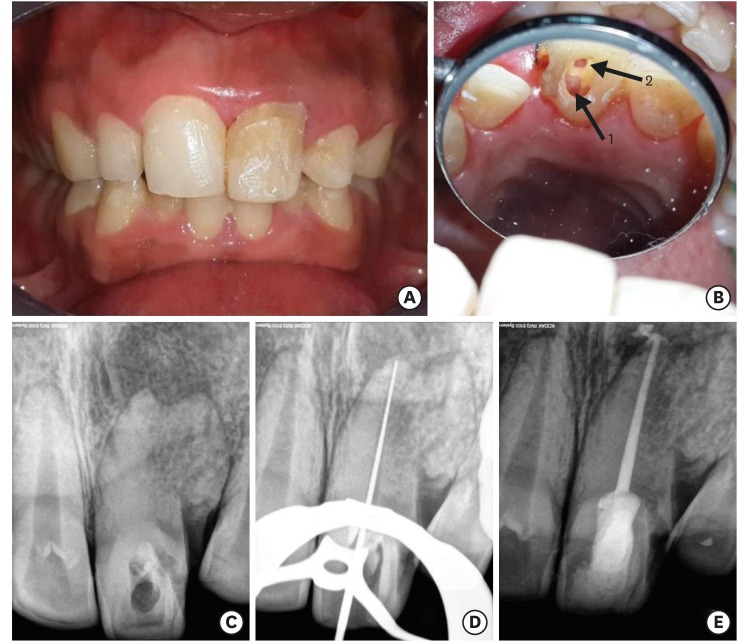
(A) Initial clinical photograph shows discoloration of tooth #21. (B) Canal orifice (1) and labial perforation area extended subgingivally (2) (C) Intraoral radiograph of tooth #21 with periapical lesion and lateral radiopaque shadow. (D) Working length determination radiograph. (E) Post-obturation radiograph of tooth #21.
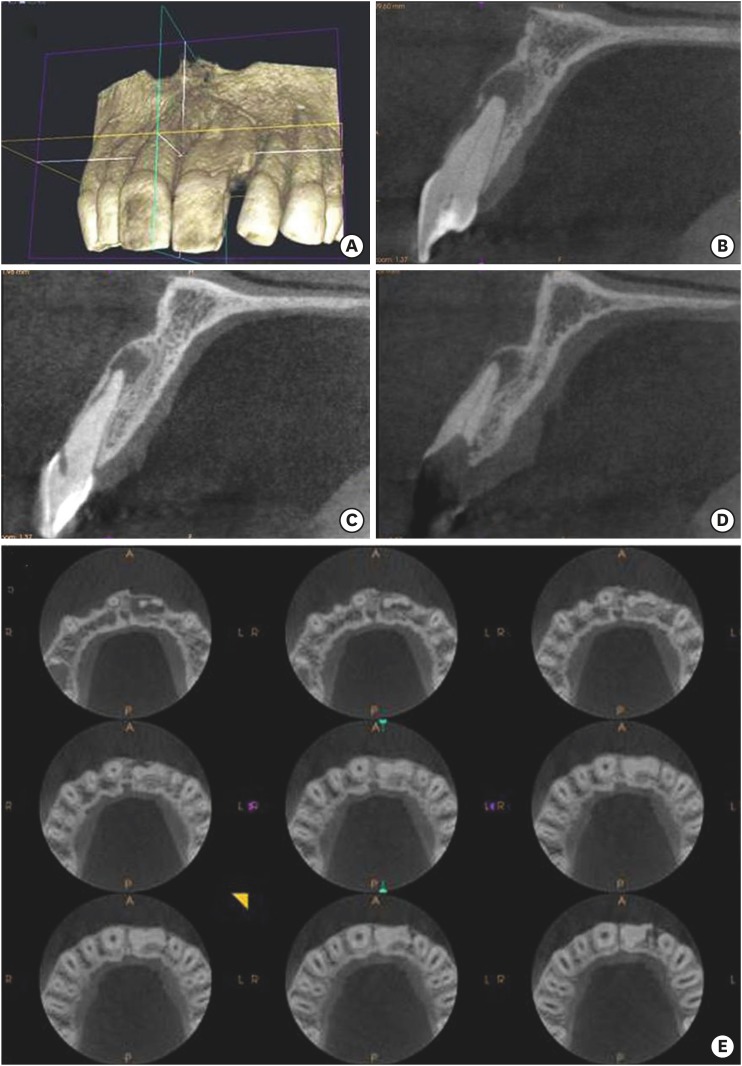
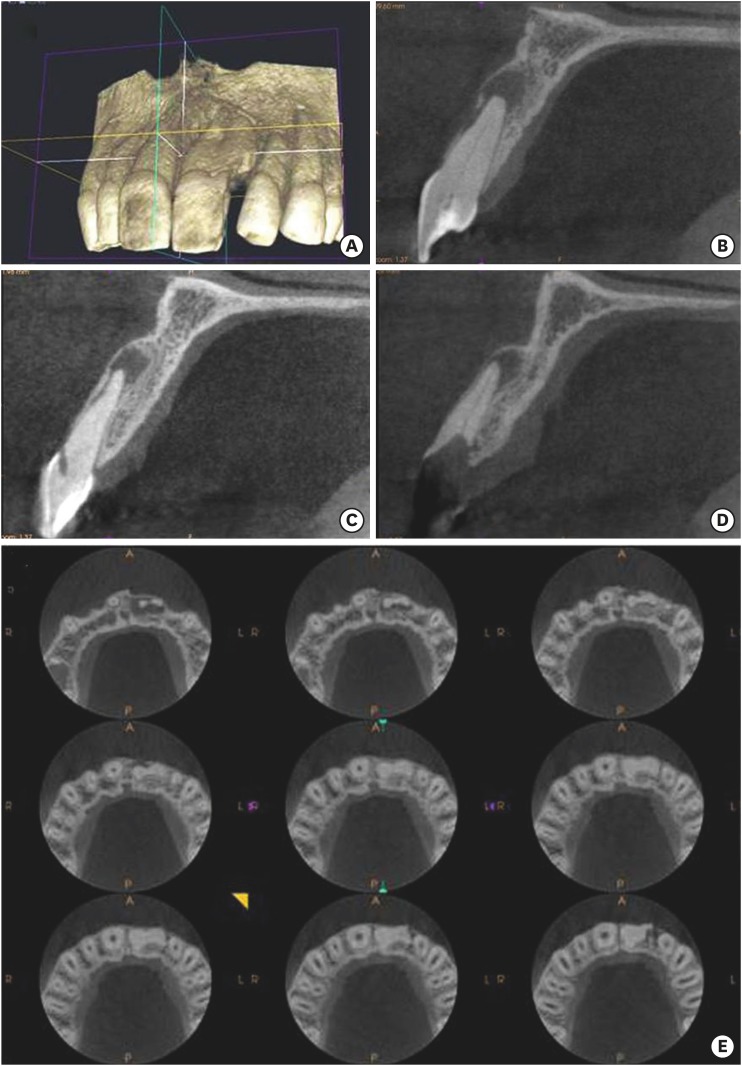
CBCT images showed the presence of extra root fused with the root of tooth #21 bellow cervical line continuing till the apex. (B) Periapical lesion of tooth #21. (C) Perforation area extended to labial surface. (D) Presence of canal in supernumerary root.
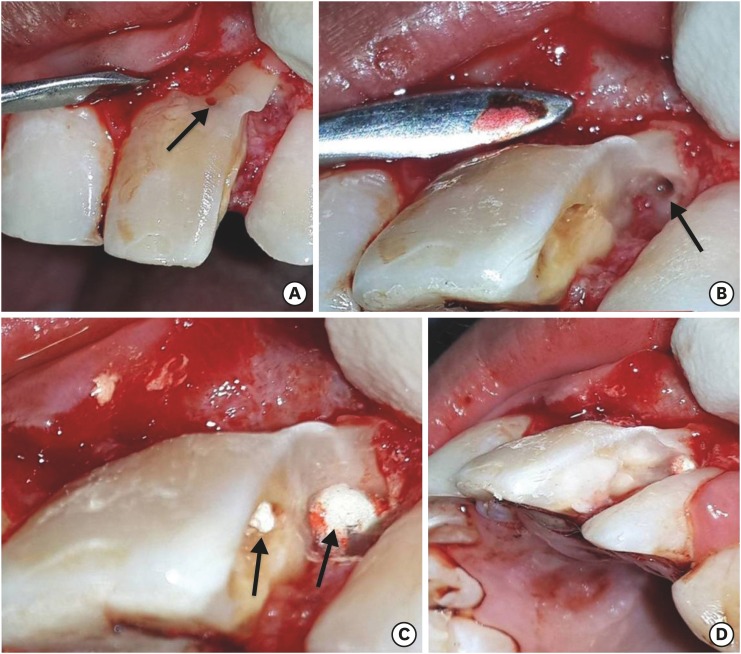
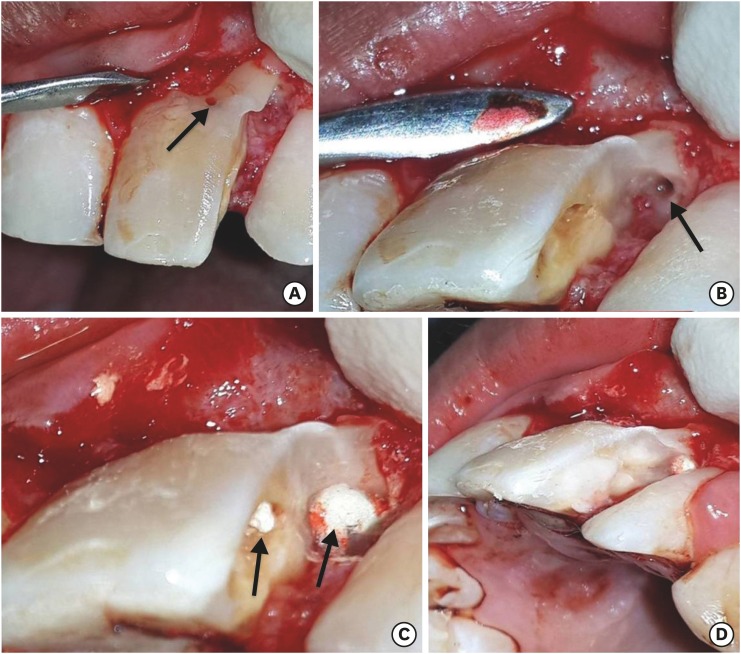
(A) Perforation area was identified on labial surface after flap reflection. (B) Canal found in supernumerary root. (C) Sealed labial perforation area (arrow) and obturated supernumerary root canal with MTA (arrow). (D) Distal access cavity was sealed with resin modified glass ionomer cement.
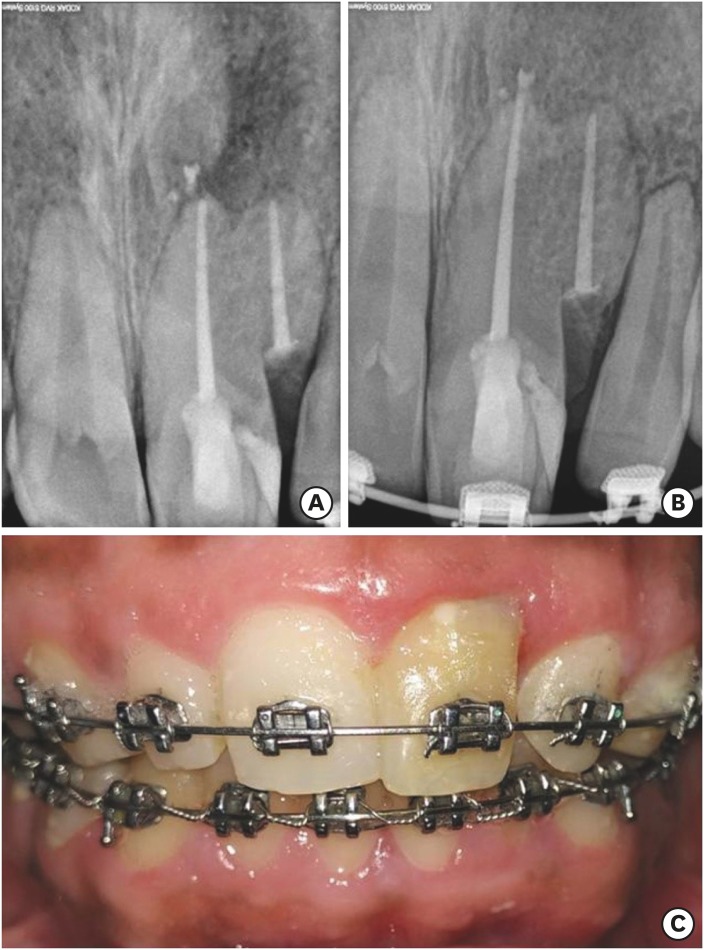
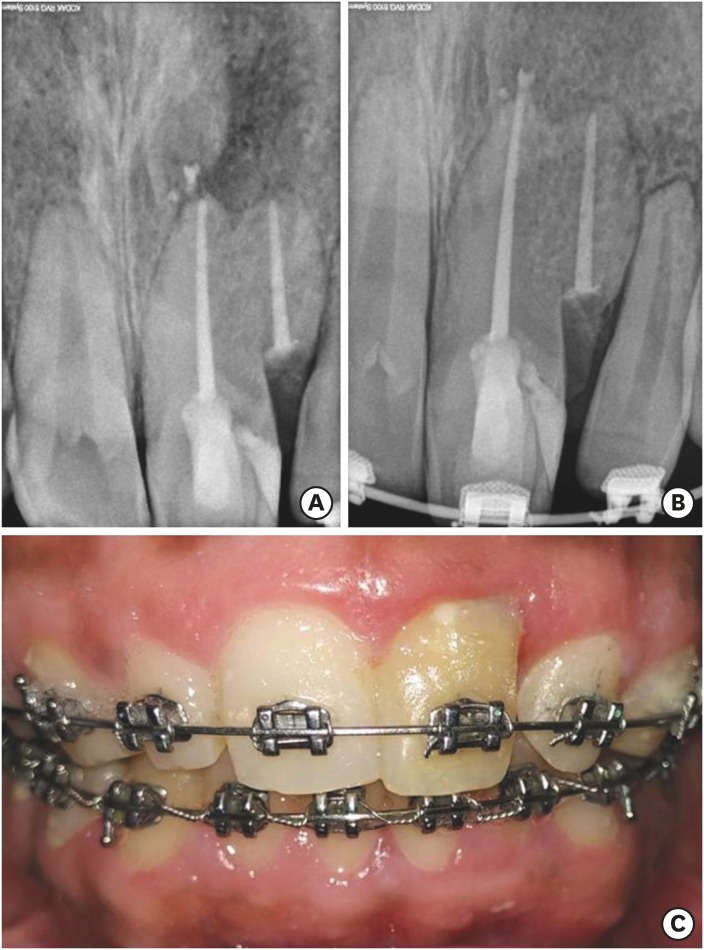
(A) Post treatment radiograph. (B) One year follow-up radiograph. (C) One year follow-up clinical photograph.
DISCUSSION
CONCLUSION
-
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
-
Author Contributions:
Conceptualization: Badole GP.
Data curation: Badole GP, Parlikar A.
Formal analysis: Badole GP, Parlikar A.
Investigation: Shenoi PR, Badole GP, Parlikar A.
Methodology: Shenoi PR, Badole GP, Parlikar A.
Project administration: Shenoi PR.
Supervision: Shenoi PR, Badole GP.
Validation: Shenoi PR, Badole GP.
Writing - original draft: Badole GP.
Writing - review & editing: Shenoi PR, Badole GP, Parlikar A.
- 1. Miles AE. Malformations of the teeth. Proc R Soc Med 1954;47:817-826.ArticlePubMedPMCPDF
- 2. De Jonge TE. Geminate tooth formation: schizodontia and synodontia, abstracted. Dent Abstr 1957;2:41.
- 3. Rani A K, Metgud S, Yakub SS, Pai U, Toshniwal NG, Bawaskar N. Endodontic and esthetic management of maxillary lateral incisor fused to a supernumerary tooth associated with a talon cusp by using spiral computed tomography as a diagnostic aid: a case report. J Endod 2010;36:345-349.ArticlePubMed
- 4. Hagman FT. Anomalies of form and number, fused primary teeth, a correlation of the dentitions. ASDC J Dent Child 1988;55:359-361.PubMed
- 5. Kayalibay H, Uzamis M, Akalin A. The treatment of a fusion between the maxillary central incisor and supernumerary tooth: report of a case. J Clin Pediatr Dent 1996;20:237-240.PubMed
- 6. Velasco LF, de Araujo FB, Ferreira ES, Velasco LE. Esthetic and functional treatment of a fused permanent tooth: a case report. Quintessence Int 1997;28:677-680.PubMed
- 7. Cho KM, Jang JH, Park SH. Clinical management of a fused upper premolar with supernumerary tooth: a case report. Restor Dent Endod 2014;39:319-323.ArticlePubMedPMC
- 8. Mazumdar P, Das UK, Rahaman SM. Endodontic management of geminated tooth: a case report. Int J Sci Res Public 2013;3:1-4.
- 9. Mader CL. Fusion of teeth. J Am Dent Assoc 1979;98:62-64.ArticlePubMed
- 10. Lowell RJ, Solomon AL. Fused Teeth. J Am Dent Assoc 1964;68:762.PubMed
- 11. Hülsmann M, Bahr R, Grohmann U. Hemisection and vital treatment of a fused tooth--literature review and case report. Endod Dent Traumatol 1997;13:253-258.ArticlePubMed
- 12. Kurihara Y. Studies on the teeth from thalidomide baby. Jpn J Pediatr Dent 1963;1:68-74.
- 13. Knudsen PA. Fusion of upper incisors at bud or cap stage in mouse embryos with exencephaly induced by hypervitaminosis A. Acta Odontol Scand 1965;23:549-565.ArticlePubMed
- 14. Scerri E, Gatt G, Camilleri S, Mupparapu M. Morphologic and developmental disturbances of permanent teeth following trauma to primary dentition in a selected group of Maltese children. Quintessence Int 2010;41:717-724.PubMed
- 15. Hattab FN. Double talon cusps on supernumerary tooth fused to maxillary central incisor: review of literature and report of case. J Clin Exp Dent 2014;6:e400-e407.ArticlePubMedPMC
- 16. Schuurs AH, van Loveren C. Double teeth: review of the literature. ASDC J Dent Child 2000;67:313-325.PubMed
- 17. Yuen SW, Chan JC, Wei SH. Double primary teeth and their relationship with the permanent successors: a radiographic study of 376 cases. Pediatr Dent 1987;9:42-48.PubMed
- 18. Maibaum WW. Fusion of confusion? Oral Surg Oral Med Oral Pathol 1990;69:656-657.
- 19. Sivolella S, Bressan E, Mirabal V, Stellini E, Berengo M. Extraoral endodontic treatment, odontotomy and intentional replantation of a double maxillary lateral permanent incisor: case report and 6-year follow-up. Int Endod J 2008;41:538-546.ArticlePubMed
- 20. Nunes E, de Moraes IG, de Novaes PM, de Sousa SM. Bilateral fusion of mandibular second molars with supernumerary teeth: case report. Braz Dent J 2002;13:137-141.ArticlePubMed
- 21. Kim E, Jou YT. A supernumerary tooth fused to the facial surface of a maxillary permanent central incisor: case report. J Endod 2000;26:45-48.ArticlePubMed
- 22. Krishnamurthy M, Kumar VN, Leburu A, Jeddy N. Fusion of maxillary central incisors with mesiodens. J Oral Maxillofac Pathol 2018;22:S131-S134.ArticlePubMedPMC
- 23. Kim SY, Choi SC, Chung YJ. Management of the fused permanent upper lateral incisor: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2011;111:649-652.ArticlePubMed
- 24. Sammartino G, Cerone V, Gasparro R, Riccitiello F, Trosino O. Multidisciplinary approach to fused maxillary central incisors: a case report. J Med Case Reports 2014;8:398.ArticlePubMedPMCPDF
- 25. Aydemir S, Ozel E, Arukaslan G, Tekce N. Clinical management of a fused mandibular lateral incisor with supernumerary tooth: a case report. Dent Res J (Isfahan) 2016;13:80-84.ArticlePubMedPMC
- 26. Samimi P, Shirban MR, Arbabzadeh-Zavareh F. Non-invasive management of fused upper incisors. Dent Res J (Isfahan) 2012;9:107-110.ArticlePubMedPMC
- 27. Kalender WA, Seissler W, Klotz E, Vock P. Spiral volumetric CT with single-breath-hold technique, continuous transport, and continuous scanner rotation. Radiology 1990;176:181-183.ArticlePubMed
- 28. Patel S, Dawood A, Ford TP, Whaites E. The potential applications of cone beam computed tomography in the management of endodontic problems. Int Endod J 2007;40:818-830.ArticlePubMed
- 29. Ludlow JB, Davies-Ludlow LE, Brooks SL, Howerton WB. Dosimetry of 3 CBCT devices for oral and maxillofacial radiology: CB Mercuray, NewTom 3G and i-CAT. Dentomaxillofac Radiol 2006;35:219-226.ArticlePubMed
- 30. Badole GP, Warhadpande MM, Shenoi PR, Lachure C, Badole SG. A rare root canal configuration of bilateral maxillary first molar with 7 root canals diagnosed using cone-beam computed tomographic scanning: a case report. J Endod 2014;40:296-301.ArticlePubMed
- 31. Björn H. Experimental studies on reattachment. Dent Pract Dent Rec 1961;11:351.
- 32. Helsham RW. Some observations of the subject of roots of teeth retained in the jaws as a result of incomplete exodontia. Aust Dent J 1960;5:70-77.
- 33. Rodd HD, Davidson LE, Livesey S, Cooke ME. Survival of intentionally retained permanent incisor roots following crown root fractures in children. Dent Traumatol 2002;18:92-97.ArticlePubMedPDF
- 34. Choi S, Yeo IS, Kim SH, Lee JB, Cheong CW, Han JS. A root submergence technique for pontic site development in fixed dental prostheses in the maxillary anterior esthetic zone. J Periodontal Implant Sci 2015;45:152-155.ArticlePubMedPMCPDF
- 35. Reames RL, Nickel JS, Patterson SS, Boone M, el-Kafrawy AH. Clinical, radiographic, and histological study of endodontically treated retained roots to preserve alveolar bone. J Endod 1975;1:367-373.ArticlePubMed
- 36. Park JB, Lee JH. Use of mineral trioxide aggregate in the open apex of a maxillary first premolar. J Oral Sci 2008;50:355-358.ArticlePubMed
- 37. Badole GP, Warhadpande MM, Bahadure RN, Badole SG. Nonsurgical endodontic treatment of permanent maxillary incisors with immature apex and a large periapical lesion: a case report. Gen Dent 2015;63:58-60.
- 38. Huang GT. Apexification: the beginning of its end. Int Endod J 2009;42:855-866.ArticlePubMed
- 39. Regan JD, Gutmann JL, Witherspoon DE. Comparison of Diaket and MTA when used as root-end filling materials to support regeneration of the periradicular tissues. Int Endod J 2002;35:840-847.PubMed
- 40. Apaydin ES, Shabahang S, Torabinejad M. Hard-tissue healing after application of fresh or set MTA as root-end-filling material. J Endod 2004;30:21-24.ArticlePubMed
REFERENCES
Tables & Figures
REFERENCES
Citations

- A rare case of fusion between a third molar and a distomolar: case report
G. M. Almeida, M.A. H. Duarte, J. R. Carvalho-Junior, R.M. C. Travassos, G. F. Silva, M.F. V. Marceliano-Alves, A. G. Limoeiro, M. P. Alcalde
Endodontics Today.2026;[Epub] CrossRef - Nonsurgical Endodontics and Decompression-Based Management of Extensive Periapical Cystic-Like Lesions: A Comparative and Radiological Study with A Two-Year Follow-Up
Roxana Talpoș-Niculescu, Ioana Veja, Carina Sonia Neagu, Laura Cristina Rusu, Șerban Talpoș-Niculescu, Mălina Popa, Luminița Maria Nica
Journal of Clinical Medicine.2025; 14(17): 6127. CrossRef - Fusion of a Tooth with a Supernumerary Tooth: A Case Report and Literature Review of 35 Cases
Tatsuya Akitomo, Satoru Kusaka, Momoko Usuda, Mariko Kametani, Ami Kaneki, Taku Nishimura, Masashi Ogawa, Chieko Mitsuhata, Ryota Nomura
Children.2023; 11(1): 6. CrossRef - Approche multidisciplinaire d’un cas de fusion incisive centrale maxillaire avec un « talon cusp »
Sonia Terbeche, Kheira Yousfi, Samia Saddat, Souad Larbi Messaoudi, Noureddine Ahmed Fouatih, G. Mer, O. Weissenbach
Revue d'Orthopédie Dento-Faciale.2022; 56(2): 205. CrossRef

 KACD
KACD
 ePub Link
ePub Link Cite
Cite

