Articles
- Page Path
- HOME > Restor Dent Endod > Volume 42(4); 2017 > Article
- Research Article Microhybrid versus nanofill composite in combination with a three step etch and rinse adhesive in occlusal cavities: five year results
-
Safa Tuncer1
 , Mustafa Demirci1
, Mustafa Demirci1 , Evren Öztaş2, Neslihan Tekçe3
, Evren Öztaş2, Neslihan Tekçe3 , Ömer Uysal4
, Ömer Uysal4 -
2017;42(4):-263.
DOI: https://doi.org/10.5395/rde.2017.42.4.253
Published online: August 21, 2017
1Department of Restorative Dentistry, Istanbul University Faculty of Dentistry, Istanbul, Turkey.
2Department of Orthodontics, Istanbul University Faculty of Dentistry, Istanbul, Turkey.
3Department of Restorative Dentistry, Kocaeli University Faculty of Dentistry, Kocaeli, Turkey.
4Department of Biostatistics and Medical Informatics, Bezmialem Vakif University Faculty of Medicine, Istanbul, Turkey.
- Correspondence to Neslihan Tekçe, DDS, PhD. Assistant Professor, Department of Restorative Dentistry, Kocaeli University Faculty of Dentistry, Yuvacik, Basiskele, Kocaeli 41190, Turkey. Tel: +90-262-344-2222, Fax: +90-262-344-2109, neslihan_arslann@hotmail.com
Copyright © 2017. The Korean Academy of Conservative Dentistry
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 1,382 Views
- 6 Download
- 6 Crossref
Abstract
-
Objectives The aim of the study was to evaluate the 5-year clinical performance of occlusal carious restorations using nanofill and microhybrid composites, in combination with 3-step etch-and-rinse adhesives, in patients who were going to commence orthodontic treatment.
-
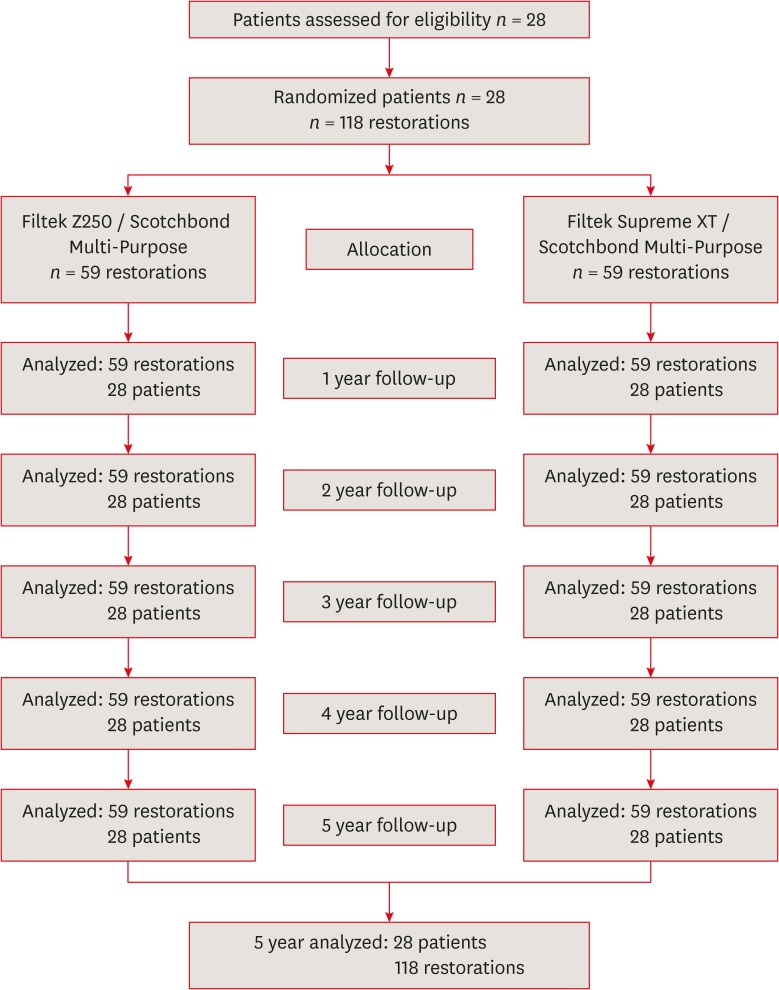
Materials and Methods A total of 118 restorations for occlusal caries were conducted prior to orthodontic treatment. Occlusal restorations were performed both with Filtek Supreme XT (3M ESPE) and Filtek Z250 (3M ESPE) before beginning orthodontic treatment with fixed orthodontic bands. Restorations were clinically evaluated at baseline and at 1, 2, 3, 4, and 5-year recalls.
-
Results None of the microhybrid (Filtek Z250) and nanofill (Filtek Supreme XT) composite restorations was clinically unacceptable with respect to color match, marginal discoloration, wear or loss of anatomical form, recurrent caries, marginal adaptation, or surface texture. A 100% success rate was recorded for both composite materials. There were no statistically significant differences in any of the clinical evaluation criteria between Filtek Z250 and Filtek Supreme XT restorations for each evaluation period.
-
Conclusions The composite restorations showed promising clinical results relating to color matching, marginal discoloration, wear or loss of anatomical form, recurrent caries, marginal adaptation, and surface texture at the end of the 5-year evaluation period.
INTRODUCTION
MATERIALS AND METHODS
The brand names, chemical compositions, application procedures, and manufacturers of the materials used in the study
Inclusion and exclusion criteria
Direct clinical evaluation criteria (modified USPHS criteria) using visual inspection
Direct clinical evaluation criteria (modified Ryge criteria) using explorer
RESULTS
Distribution of occlusal restorations according to composite material type and tooth number
Results of clinical evaluation of 2 different composite restorations using modified USPHS criteria
DISCUSSION
CONCLUSIONS
-
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
-
Author Contributions:
Conceptualization: Tuncer S, Demirci M.
Data curation: Tuncer S, Demirci M, Öztaş E, Tekçe N.
Formal analysis: Uysal Ö.
Funding acquisition: Tuncer S.
Investigation: Tuncer S, Demirci M, Tekçe N.
Methodology: Tuncer S, Demirci M.
Project administration: Tuncer S, Demirci M.
Resources: Demirci M.
Software: Uysal Ö.
Supervision: Demirci M.
Validation: Tuncer S, Demirci M.
Visualization: Demirci M, Tekçe N.
Writing - original draft: Tuncer S, Demirci M.
Writing - review & editing: Tuncer S, Demirci M, Öztaş E, Tekçe N.
- 1. Uribe FA, Chandhoke TK, Nanda R. Individualized orthodontic diagnosis. In: Nanda R, editor. Esthetics and biomechanics in orthodontics. 2nd ed. St. Louis (MA): Elsevier Saunders; 2015. p. 1-32.
- 2. Bourzgui F, Sebbar M, Hamza M. Orthodontics and caries. In: Naretto S, editor. Principles in contemporary orthodontics. Rijeka: INTECH; 2011. p. 309-326.
- 3. Chaussain C, Opsahl Vital S, Viallon V, Vermelin L, Haignere C, Sixou M, Lasfargues JJ. Interest in a new test for caries risk in adolescents undergoing orthodontic treatment. Clin Oral Investig 2010;14:177-185.ArticlePubMedPDF
- 4. Lynch CD, Opdam NJ, Hickel R, Brunton PA, Gurgan S, Kakaboura A, Shearer AC, Vanherle G, Wilson NH; Academy of Operative Dentistry European Section. Guidance on posterior resin composites: Academy of Operative Dentistry - European Section. J Dent 2014;42:377-383.ArticlePubMed
- 5. Ferracane JL. Current trends in dental composites. Crit Rev Oral Biol Med 1995;6:302-318.ArticlePubMedPDF
- 6. Ilie N, Hickel R. Resin composite restorative materials. Aust Dent J 2011;56(Supplement 1):59-66.ArticlePubMed
- 7. de Andrade AK, Duarte RM, Medeiros e Silva FD, Batista AU, Lima KC, Monteiro GQ, Montes MA. Resin composite class I restorations: a 54-month randomized clinical trial. Oper Dent 2014;39:588-594.ArticlePubMedPDF
- 8. Ferracane JL. Resin composite--state of the art. Dent Mater 2011;27:29-38.ArticlePubMed
- 9. Gresnigt MM, Kalk W, Ozcan M. Randomized controlled split-mouth clinical trial of direct laminate veneers with two micro-hybrid resin composites. J Dent 2012;40:766-775.ArticlePubMed
- 10. Wolff D, Kraus T, Schach C, Pritsch M, Mente J, Staehle HJ, Ding P. Recontouring teeth and closing diastemas with direct composite buildups: a clinical evaluation of survival and quality parameters. J Dent 2010;38:1001-1009.ArticlePubMed
- 11. Neves Ade A, Coutinho E, De Munck J, Van Meerbeek B. Caries-removal effectiveness and minimal-invasiveness potential of caries-excavation techniques: a micro-CT investigation. J Dent 2011;39:154-162.ArticlePubMed
- 12. de Souza Costa CA, Teixeira HM, Lopes do Nascimento AB, Hebling J. Biocompatibility of resin-based dental materials applied as liners in deep cavities prepared in human teeth. J Biomed Mater Res B Appl Biomater 2007;81:175-184.PubMed
- 13. Demirci M, Uysal O. Clinical evaluation of a polyacid-modified resin composite (Dyract AP) in Class I cavities: 3-year results. Am J Dent 2006;19:376-381.PubMed
- 14. Barnes DM, Blank LW, Gingell JC, Gilner PP. A clinical evaluation of a resin-modified glass ionomer restorative material. J Am Dent Assoc 1995;126:1245-1253.PubMed
- 15. Ryge G. Clinical criteria. Int Dent J 1980;30:347-358.PubMed
- 16. Cvar JF, Ryge G. Reprint of criteria for the clinical evaluation of dental restorative materials. 1971. Clin Oral Investig 2005;9:215-232.PubMed
- 17. Sakaguchi RL, Powers JM. Craig's restorative dental materials. 13th ed. Philadelphia (PA): Elsevier Mosby; 2012. p. 166-167.
- 18. 3M Dental Products Laboratory (US). Filtek™ Z250 universal restorative system: technical product profile. St. Paul (MN): 3M; 1998.
- 19. Cetin AR, Unlu N, Cobanoglu N. A five-year clinical evaluation of direct nanofilled and indirect composite resin restorations in posterior teeth. Oper Dent 2013;38:E1-E11.ArticlePDF
- 20. Lempel E, Tóth Á, Fábián T, Krajczár K, Szalma J. Retrospective evaluation of posterior direct composite restorations: 10-year findings. Dent Mater 2015;31:115-122.ArticlePubMed
- 21. da Rosa Rodolpho PA, Cenci MS, Donassollo TA, Loguércio AD, Demarco FF. A clinical evaluation of posterior composite restorations: 17-year findings. J Dent 2006;34:427-435.ArticlePubMed
- 22. Manhart J, Chen H, Hamm G, Hickel R. Buonocore Memorial Lecture. Review of the clinical survival of direct and indirect restorations in posterior teeth of the permanent dentition. Oper Dent 2004;29:481-508.PubMed
- 23. Demarco FF, Corrêa MB, Cenci MS, Moraes RR, Opdam NJ. Longevity of posterior composite restorations: not only a matter of materials. Dent Mater 2012;28:87-101.ArticlePubMed
- 24. Bagheri R, Burrow MF, Tyas M. Influence of food-simulating solutions and surface finish on susceptibility to staining of aesthetic restorative materials. J Dent 2005;33:389-398.ArticlePubMed
- 25. Manhart J, Chen HY, Hickel R. Clinical evaluation of the posterior composite Quixfil in class I and II cavities: 4-year follow-up of a randomized controlled trial. J Adhes Dent 2010;12:237-243.PubMed
- 26. Wilder AD Jr, May KN Jr, Bayne SC, Taylor DF, Leinfelder KF. Seventeen-year clinical study of ultraviolet-cured posterior composite Class I and II restorations. J Esthet Dent 1999;11:135-142.ArticlePubMed
- 27. Baldissera RA, Corrêa MB, Schuch HS, Collares K, Nascimento GG, Jardim PS, Moraes RR, Opdam NJ, Demarco FF. Are there universal restorative composites for anterior and posterior teeth? J Dent 2013;41:1027-1035.ArticlePubMed
- 28. Da Rosa Rodolpho PA, Donassollo TA, Cenci MS, Loguércio AD, Moraes RR, Bronkhorst EM, Opdam NJ, Demarco FF. 22-Year clinical evaluation of the performance of two posterior composites with different filler characteristics. Dent Mater 2011;27:955-963.ArticlePubMed
- 29. Schirrmeister JF, Huber K, Hellwig E, Hahn P. Four-year evaluation of a resin composite including nanofillers in posterior cavities. J Adhes Dent 2009;11:399-404.PubMed
REFERENCES
Tables & Figures
REFERENCES
Citations

- Proposal of a Modular Classification System for Direct Dental Resin Composites Based on Clinical Applications
Philippe Francois, Mathieu Izart, Timothy Fasham, Yasmine Smail, Marie Jannot, Stéphane Le Goff, Fleur Beres, Max Troizier-Cheyne, Sara Bergman, Christian Moussally, Sarah Abdel-Gawad, Elisabeth Dursun, Romain Ceinos, Elisa Caussin, Jean-Pierre Attal
Polymers.2025; 17(5): 564. CrossRef - The Application of Nanomaterials for the Rescue of a Single Compromised Tooth with a Multidisciplinary Approach: Case Report and Scoping Review
Riccardo Aiuto, Federico Alcide Villani, Erica Lipani, Aysenur Kara, Daniele Garcovich, Mario Dioguardi, Elisabetta Carli, Dino Re
The Open Dentistry Journal.2024;[Epub] CrossRef - Effect of Sucrose Concentration on Streptococcus mutans Adhesion to Dental Material Surfaces
Anamarija Zore, Franc Rojko, Nives Matijaković Mlinarić, Jona Veber, Aleksander Učakar, Roman Štukelj, Andreja Pondelak, Andrijana Sever Škapin, Klemen Bohinc
Coatings.2024; 14(2): 165. CrossRef - Comparative Evaluation of Shear Bond Strength Of Various Core Build – up Materials In Maxillary Anterior Teeth - An In-Vitro Study
Pavithra Prabakaran, Laxmi Priya C H, Annapoorna B S
Journal of Indian Dental Association.2022;[Epub] CrossRef - A three-year randomized clinical trial evaluating direct posterior composite restorations placed with three self-etch adhesives
Joseph Sabbagh, Layal El Masri, Jean Claude Fahd, Paul Nahas
Biomaterial Investigations in Dentistry.2021; 8(1): 92. CrossRef - Enhanced mechanical properties are possible with urethane dimethacrylate-based experimental restorative dental composite
Aftab Ahmed Khan, Abdulaziz Abdullah AlKhureif, Badreldin A Mohamed, Leonel S J Bautista
Materials Research Express.2020; 7(10): 105307. CrossRef
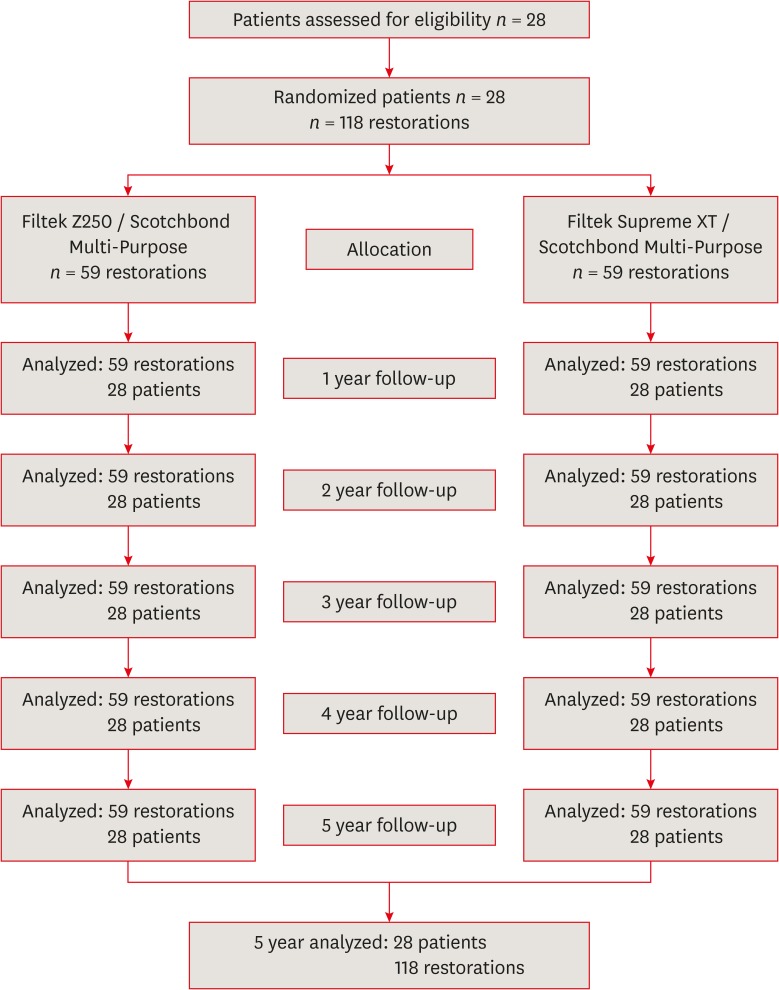
Figure 1
The brand names, chemical compositions, application procedures, and manufacturers of the materials used in the study
| Adhesive | Component | Procedure | Manufacturer |
|---|---|---|---|
| Scotchbond Multi-Purpose | Etchant: 35% H3PO4, water, and silica | Apply the etchant to dentin and enamel for 15 sec. Rinse the surface for 15 sec and dry the surface slightly leaving a visible moist dentin surface. Apply the primer and dry gently for 5 sec. Apply the bond and light cure for 20 sec. | 3M ESPE, St. Paul, MN, USA |
| Primer: 2-hydroxyethylmethacrylate, polyalkenoic acid, copolymer, and water | |||
| Adhesive: 2-hydroxyethylmethacrylate, Bis-GMA, and photoinitiator | |||
| Filtek Supreme XT | Bis-GMA, UDMA, TEGDMA, Bis-EMA, silica filler, zirconia filler, and aggregated zirconia/silica cluster filler | Tooth color to be restored was selected using the corresponding composite guide or custom composite samples before isolating the tooth. The corresponding body shade was selected. In 2 mm layers or less increments of body shade were applied. Each increment was light cured 20 sec. | 3M ESPE, St. Paul, MN, USA |
| Filtek Z250 | Bis-GMA, UDMA, Bis-EMA, silica filler, and zirconia filler | Tooth color to be restored was selected using the corresponding composite guide or custom composite samples before isolating the tooth. Place 3M Filtek Z250 restorative in increments less than 2.5 mm. Light cure each increment for 20 sec. | 3M ESPE, St. Paul, MN, USA |
H3PO4, phosphoric acid; Bis-GMA, bisphenol A glycidyl dimethacrylate; UDMA, urethane dimethacrylate; TEGDMA, triethylene glycol dimethacrylate; Bis-EMA, ethoxylated bisphenol A glycol dimethacrylate.
Inclusion and exclusion criteria
| Criterion | |
|---|---|
| Inclusion criteria | |
| Patients received 2 to 8 restorations for primary caries on the occlusal surface | |
| Occlusal contact with the antagonist tooth | |
| Displayed good oral hygiene | |
| Having no active periodontal or pulpal diseases | |
| Patients were required to have received orthodontic treatment with fixed appliances | |
| Willing to return for follow-up examinations as outlined by the investigators | |
| Exclusion criteria | |
| Patients with uncontrolled parafunction | |
| Presenting insufficient oral hygiene | |
| Pulp exposure during caries removal or cavities with imminent risk of pulp exposure | |
| Spontaneous pain or sensitivity to percussion | |
| Patients were pregnant or nursing | |
| Patients had periodontal or gingival disease | |
Direct clinical evaluation criteria (modified USPHS criteria) using visual inspection
| Criterion | Rating | Aspect |
|---|---|---|
| Color match | Alpha | There is no a mismatch in color, shade and/or translucency between the restoration and the adjacent tooth structure. |
| Bravo | There is a mismatch in color, shade and/or translucency between the restoration and the adjacent tooth structure, but the mismatch is within the normal range of tooth color, shade and/or translucency. | |
| Charlie | The mismatch is between the restoration and the adjacent tooth structure outside the normal range of tooth color, shade and/or translucency. | |
| Cavosurface marginal discoloration | Alpha | There is no discoloration anywhere on the margin between the restoration and the tooth structure. |
| Bravo | There is discoloration anywhere on the margin between the restoration and the tooth structure, but the discoloration has not penetrated along the margin of the restorative material in an enamel direction and can be polished away. | |
| Charlie | The discoloration has penetrated along the margin of the restorative material in an enamel direction. | |
| Wear/anatomic form | Alpha | The restoration is not under-contoured, that is, the restorative material is not discontinuous with existing anatomic form. |
| Bravo | The restoration is under-contoured, that is, the restorative material is discontinuous with existing anatomic form, but sufficient restorative material is not missing so as to expose the enamel or base. | |
| Charlie | Sufficient restorative material is missing so as to expose the enamel or base. | |
| Caries | Alpha | There is no evidence of caries contiguous with the margin of the restoration. |
| Bravo | There is evidence of caries contiguous with the margin of the restoration. |
USPHS, United States Public Health Service.
Direct clinical evaluation criteria (modified Ryge criteria) using explorer
| Criterion | Rating | Aspect |
|---|---|---|
| Marginal adaptation | Alpha | There is no visible evidence of a crevice along the margin into which the explorer will penetrate. |
| Bravo | There is visible evidence of a crevice along the margin into which the explorer will penetrate. The enamel or base is not exposed. | |
| Charlie | There is visible evidence of a crevice along the margin into which the explorer will penetrate. The enamel or base is exposed. | |
| Delta | The restoration is fractured or missing in part or in toto. | |
| Surface texture | Alpha | Surface of restoration is smooth. |
| Bravo | Surface of restoration is slightly rough or pitted, can be refinished. | |
| Charlie | Surface deeply pitted, irregular grooves (not related to anatomy), cannot be refinished. | |
| Delta | Surface is fractured or flaking. |
Distribution of occlusal restorations according to composite material type and tooth number
| Composite/dentin adhesive | No. | Tooth number | |||||||
|---|---|---|---|---|---|---|---|---|---|
| #16 | #17 | #26 | #27 | #36 | #37 | #46 | #47 | ||
| Filtek Z250/Scotchbond Multi-Purpose | 59 | 6 | 8 | 7 | 14 | 2 | 10 | 2 | 10 |
| Filtek Supreme XT/Scotchbond Multi-Purpose | 59 | 6 | 11 | 5 | 11 | 2 | 9 | 6 | 9 |
| Sum of restorations | 118 | 12 | 19 | 12 | 25 | 4 | 19 | 8 | 19 |
Results of clinical evaluation of 2 different composite restorations using modified USPHS criteria
| Observation time/composite | Recall rate | Survival rate | Retention | Color match | Marginal discoloration | Wear/anatomic form | Caries | Marginal adaptation | Surface texture | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | C | A | B | C | A | B | C | A | B | C | A | C | A | B | C | D | A | B | C | D | ||||
| Baseline | ||||||||||||||||||||||||
| Filtek Z250 | 100.0 (59) | 100.0 (59) | 100.0 (59) | - | 100.0 (59) | - | - | 100.0 (59) | - | - | 100.0 (59) | - | - | 100.0 (59) | - | 100.0 (59) | - | - | - | 100.0 (59) | - | - | - | |
| Filtek Supreme XT | 100.0 (59) | 100.0 (59) | 100.0 (59) | - | 100.0 (59) | - | - | 100.0 (59) | - | - | 98.3 (58) | 1.7 (1) | - | 100.0 (59) | - | 100.0 (59) | - | - | - | 100.0 (59) | - | - | - | |
| 1 year | ||||||||||||||||||||||||
| Filtek Z250 | 100.0 (59) | 100.0 (59) | 100.0 (59) | - | 98.3 (58) | 1.7 (1) | - | 98.3 (58) | 1.7 (1) | - | 100.0 (59) | - | 100.0 (59) | - | 98.3 (58) | 1.7 (1) | - | - | 100.0 (59) | - | - | - | ||
| Filtek Supreme XT | 100.0 (59) | 100.0 (59) | 100.0 (59) | - | 98.3 (58) | 1.7 (1) | - | 100.0 (59) | - | - | 98.3 (58) | 1.7 (1) | 100.0 (59) | - | 100.0 (59) | - | - | - | 100.0 (59) | - | - | - | ||
| 2 year | ||||||||||||||||||||||||
| Filtek Z250 | 100.0 (59) | 100.0 (59) | 100.0 (59) | - | 96.6 (57) | 3.4 (2) | - | 95.0 (56) | 5.0 (3) | - | 98.3 (58) | 1.7 (1) | 100.0 (59) | - | 98.3 (58) | 1.7 (1) | - | - | 100.0 (59) | - | - | - | ||
| Filtek Supreme XT | 100.0 (59) | 100.0 (59) | 100.0 (59) | - | 96.6 (57) | 3.4 (2) | - | 100.0 (59) | - | - | 100.0 (59) | - | 100.0 (59) | - | 100.0 (59) | - | - | - | 100.0 (59) | - | - | - | ||
| 3 year | ||||||||||||||||||||||||
| Filtek Z250 | 100.0 (59) | 100.0 (59) | 100.0 (59) | - | 95.0 (56) | 5.0 (3) | - | 88.1 (52) | 11.9 (7) | - | 98.3 (58) | 1.7 (1) | 100.0 (59) | - | 98.3 (58) | 1.7 (1) | - | - | 100.0 (59) | - | - | - | ||
| Filtek Supreme XT | 100.0 (59) | 100.0 (59) | 100.0 (59) | - | 89.8 (53) | 10.2 (6) | - | 95.0 (56) | 5.0 (3) | - | 96.6 (57) | 3.4 (2) | 100.0 (59) | - | 100.0 (59) | - | - | - | 100.0 (59) | - | - | - | ||
| 4 year | ||||||||||||||||||||||||
| Filtek Z250 | 100.0 (59) | 100.0 (59) | 100.0 (59) | - | 93.2 (55) | 6.8 (4) | - | 81.4 (48) | 18.6 (11) | - | 96.6 (57) | 3.4 (2) | 100.0 (59) | - | 98.3 (58) | 1.7 (1) | - | - | 98.3 (58) | 1.7 (1) | - | - | ||
| Filtek Supreme XT | 100.0 (59) | 100.0 (59) | 100.0 (59) | - | 89.8 (53) | 10.2 (6) | - | 89.8 (53) | 10.2 (6) | - | 95.0 (56) | 5.0 (3) | 100.0 (59) | - | 98.3 (58) | 1.7 (1) | - | - | 100.0 (59) | - | - | - | ||
| 5 year | ||||||||||||||||||||||||
| Filtek Z250 | 100.0 (59) | 100.0 (59) | 100.0 (59) | - | 84.7 (50) | 15.3 (9) | - | 71.2 (42) | 28.8 (17) | 96.6 (57) | 3.4 (2) | 100.0 (59) | - | 98.3 (58) | 1.7 (1) | - | - | 98.3 (58) | 1.7 (1) | - | - | |||
| Filtek Supreme XT | 100.0 (59) | 100.0 (59) | 100.0 (59) | - | 88.1 (52) | 11.9 (7) | - | 81.4 (48) | 18.6 (11) | 95.0 (56) | 5.0 (3) | 100.0 (59) | - | 96.6 (57) | 3.4 (2) | - | - | 100.0 (59) | - | - | - | |||
Five-year data of recall rate, survival rate, retention, color match, marginal discoloration, wear or loss of anatomic form, caries, marginal adaptation, and surface texture showed no statistically significant difference (p > 0.05).
USPHS, United States Public Health Service; A, Alpha; B, Bravo; C, Charlie; D, Delta.
H3PO4, phosphoric acid; Bis-GMA, bisphenol A glycidyl dimethacrylate; UDMA, urethane dimethacrylate; TEGDMA, triethylene glycol dimethacrylate; Bis-EMA, ethoxylated bisphenol A glycol dimethacrylate.
USPHS, United States Public Health Service.
Five-year data of recall rate, survival rate, retention, color match, marginal discoloration, wear or loss of anatomic form, caries, marginal adaptation, and surface texture showed no statistically significant difference (
USPHS, United States Public Health Service; A, Alpha; B, Bravo; C, Charlie; D, Delta.

 KACD
KACD
 ePub Link
ePub Link Cite
Cite

