Abstract
Endodontic-periodontal lesions (EPLs) complicated by cemental tears present a diagnostic and therapeutic challenge. This case report describes the successful management of a 66-year-old male patient with a mandibular second molar (#18) exhibiting an EPL complicated by a cemental tear. Clinical examination revealed a draining sinus tract, deep periodontal pockets, and radiographic evidence of a “J-shaped” lesion and a radiopaque cemental fragment. The tooth had previously initiated endodontic treatment. A multidisciplinary approach involving endodontic treatment and surgical removal of the cemental tear was implemented. At 24-month follow-up, clinical and radiographic examination revealed significant improvement in periodontal health, bone regeneration, and resolution of the lesion. This case highlights the importance of considering cemental tears in the differential diagnosis of EPLs and demonstrates the efficacy of a combined endodontic-periodontal approach for achieving predictable outcomes.
-
Keywords: Dental cementum; Endodontics; Periodontal diseases; Periodontics; Root canal therapy; Tooth fractures
INTRODUCTION
Endodontic-periodontal lesions (EPLs) present complex challenges in dental practice due to their multifaceted etiology and pathogenesis. These lesions involve both pulpal and periodontal tissues, often necessitating a multidisciplinary approach for effective diagnosis and treatment [
1]. The intricate relationship between endodontic and periodontal tissues is facilitated by various anatomical pathways, including dentinal tubules, lateral and accessory canals, and apical foramina [
1].
Cemental tears, a unique form of root surface fracture, can further complicate the diagnosis and management of EPLs. Defined as the partial or complete detachment of cementum from the cemento-dentinal junction or along incremental lines within the cementum, cemental tears are often overlooked or misdiagnosed [
2]. Their presence can lead to rapid localized periodontal breakdown and may mimic or exacerbate EPLs [
3].
The prevalence of cemental tears is reported to be lower than 2%, with a higher incidence in incisors (74%) and on interproximal surfaces (79%) [
3]. Predisposing factors for cemental tears include age-related changes, occlusal trauma, and periodontal disease [
4]. The diagnosis of cemental tears is challenging, as they often present with clinical and radiographic features similar to primary endodontic diseases, primary periodontal diseases, or combined EPLs [
3].
Treatment of EPLs complicated by cemental tears requires a comprehensive approach. While primary endodontic lesions can often be managed with endodontic treatment alone, cases involving cemental tears typically necessitate both endodontic and periodontal therapies [
5]. Management strategies may include non-surgical periodontal treatment, surgical debridement, and in some cases, regenerative procedures [
2,
5].
This case report highlights the successful diagnosis and management of a mandibular second molar with an EPL complicated by a cemental tear. By presenting this case, we aim to increase awareness of cemental tears among dental professionals and demonstrate the importance of accurate diagnosis and multidisciplinary treatment planning in managing these complex cases [
3–
5].
CASE REPORT
A 66-year-old male patient with an unremarkable medical history and blood pressure of 128/72 mmHg was referred to the endodontist for root canal therapy on tooth #18 (or 37 according to FDI [Fédération Dentaire Internationale] numbering system) by the general dentist. The patient reported that the general dentist had attempted endodontic treatment on the tooth 3 months ago, following which the tooth had been asymptomatic. However, since 2 weeks, the patient had started to experience persistent pain upon biting and chewing.
Clinical examination revealed a large mesial-occlusal-distal composite restoration with #18, which had an endodontic access temporized with a temporary restoration. A draining sinus tract was noted distal to tooth #18, with periodontal probing depths of 3-4-12 (buccal) and 3-4-6 (lingual). Tooth #18 exhibited Miller’s Grade I mobility. It was nonresponsive to cold and tender to percussion and palpation. Tooth #19 had an extracoronal gold restoration, was responsive to cold, and not tender to percussion (
Table 1).
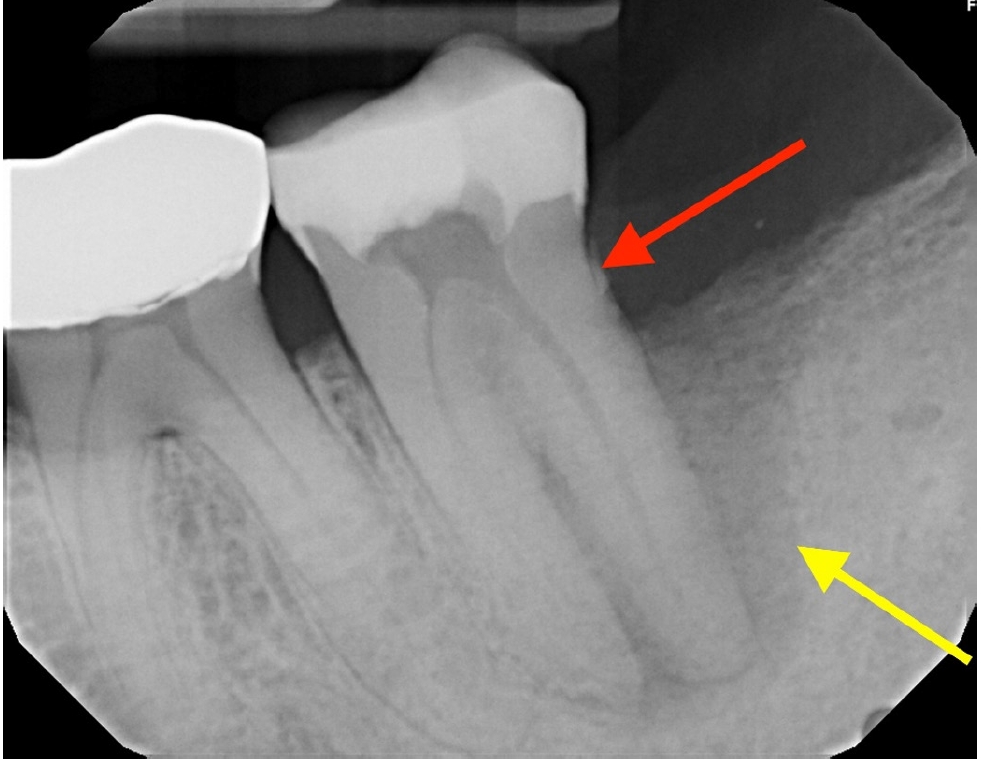
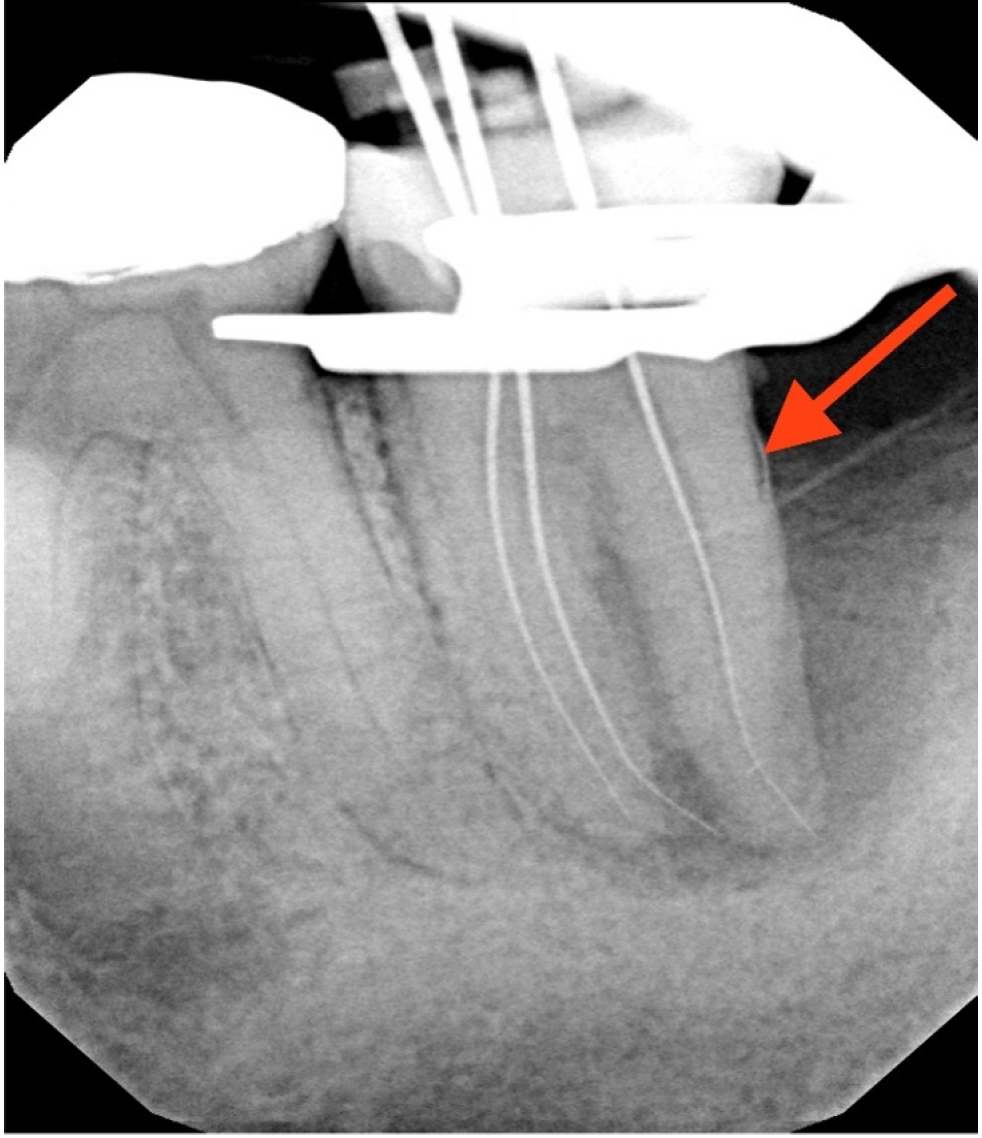
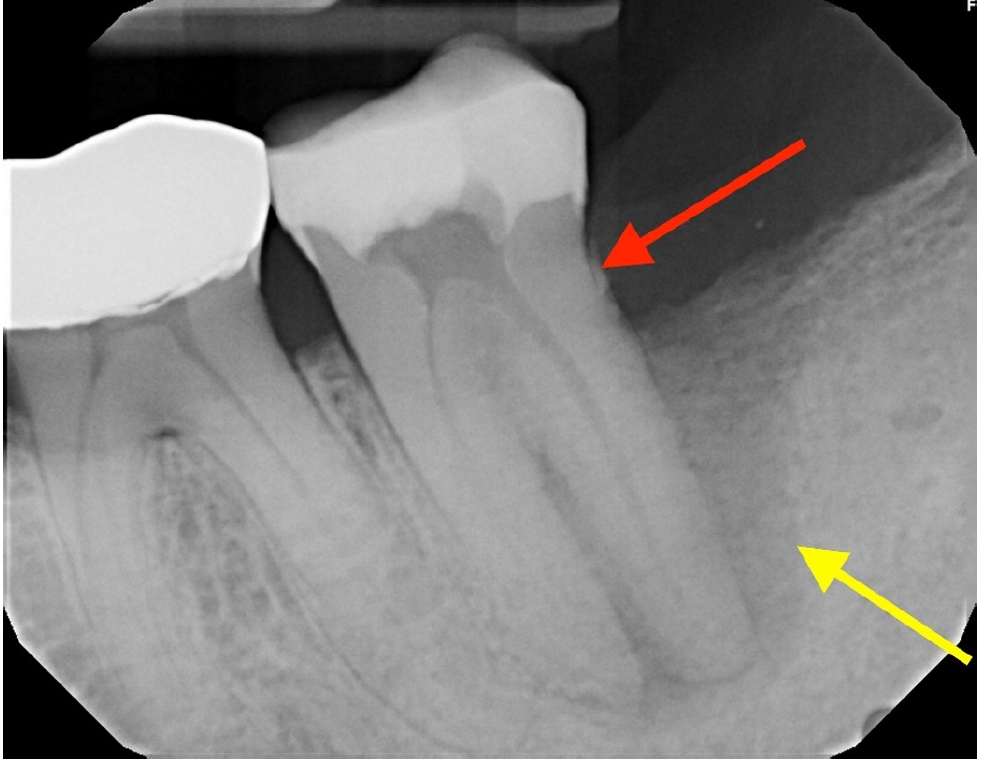
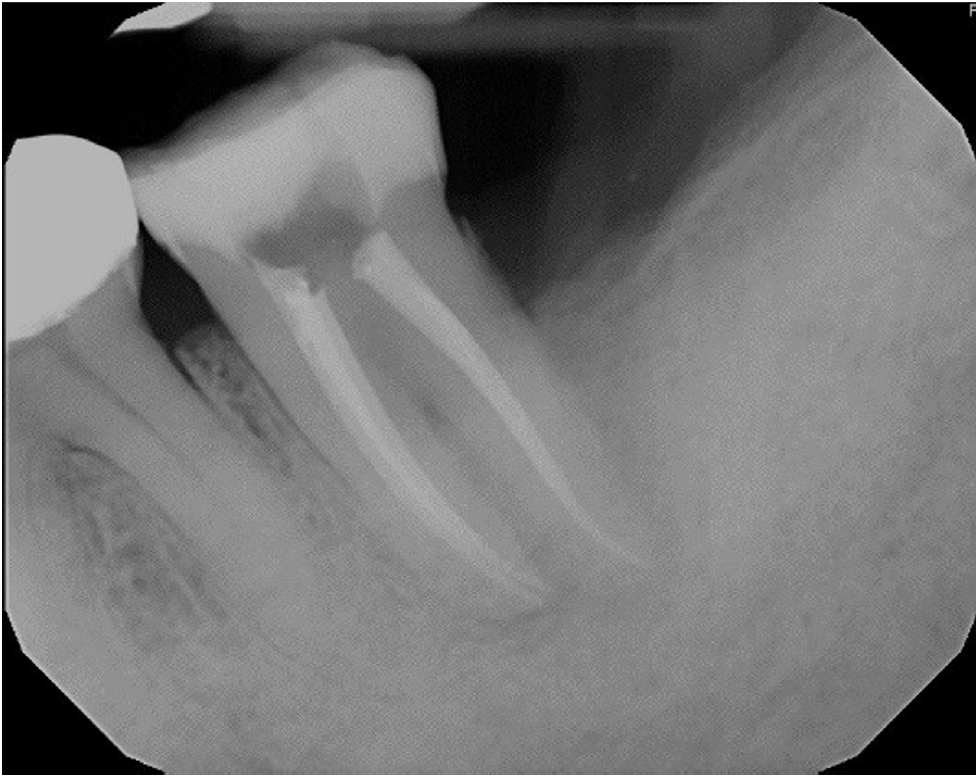
Radiographically, a “J-shaped” lesion was observed along the distal root of #18 (
Figure 1), suggestive of a primary endodontic lesion with secondary periodontal involvement. A radiopaque fragment, consistent with a cemental tear, was identified along the distal root surface (
Figure 1).
Based on the clinical and radiographic findings, a diagnosis of previously initiated therapy with chronic apical abscess was reached for #18. Owing to the advanced periodontal bone loss and deep pockets, a poor prognosis was expected for #18. The patient was informed of the findings and given the options of a multidisciplinary approach combining endodontic treatment and periodontal therapy or an alternative of extraction and prosthodontic replacement. Motivated to preserve his natural dentition, the patient opted for the conservative multidisciplinary treatment plan.
After administering two cartridges of 2% lidocaine with 1:100,000 epinephrine (Patterson Dental, St. Paul, MN, USA) as an inferior alveolar nerve block and a half cartridge as local infiltration, a rubber dam was placed for isolation. Upon access, necrotic pulp was encountered, and the pulp chamber of #18 was examined under a dental operating microscope. The absence of fractures was confirmed with methylene blue dye, and three canals (mesiobuccal, mesiolingual, and distal) were located.
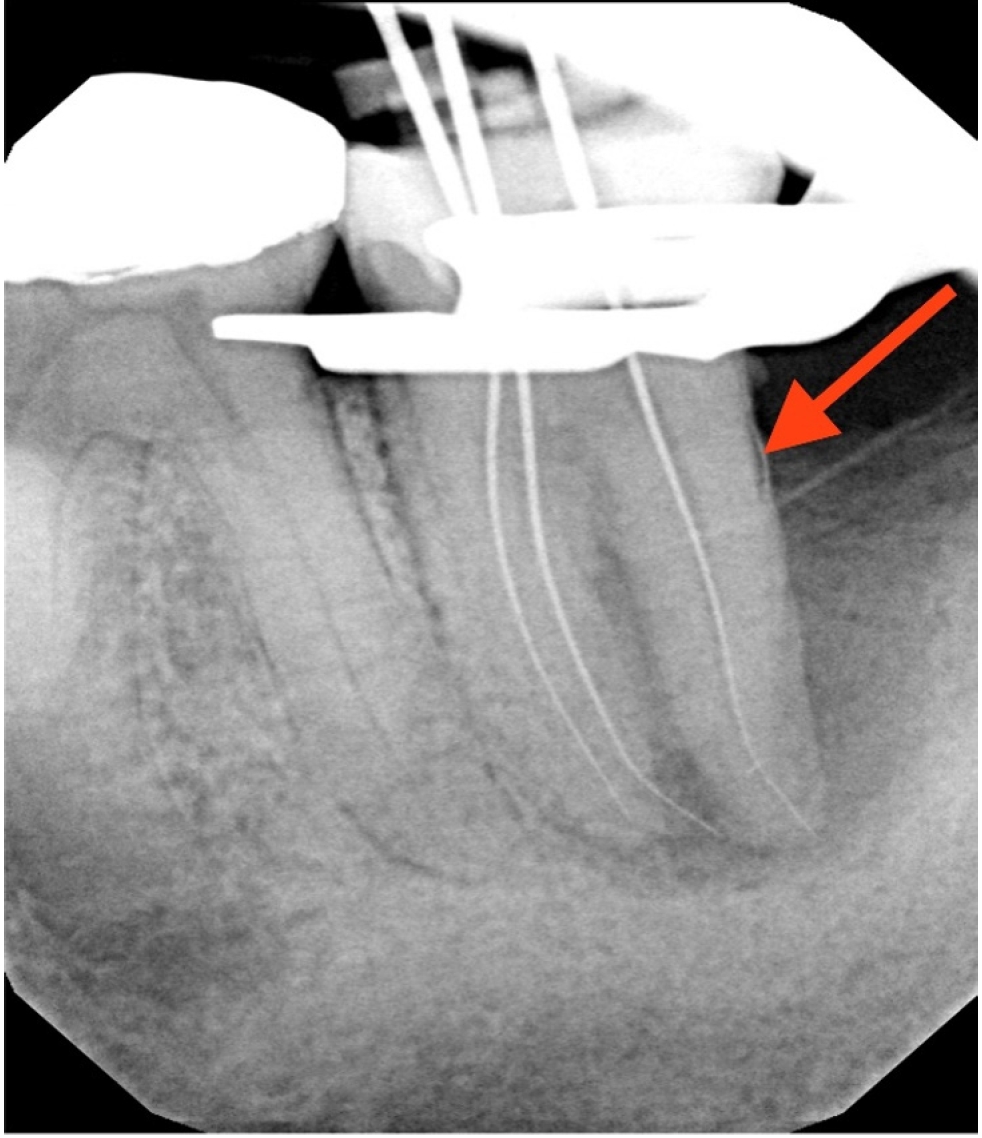
Working lengths were determined using an electronic apex locator (RootZX; J Morita, Kyoto, Japan) and confirmed with a periapical radiograph, which also showed a radiopaque fragment consistent with a cemental tear (
Figure 2). The chamber was flooded with 5% sodium hypochlorite, and the canals were instrumented using size 8, 10, 15, and 20 K files, followed by a 25/.07 Primary Wave One Gold (Dentsply Sirona, Charlotte, NC, USA) reciprocating file. Irrigation was performed with 12 mL of 5% sodium hypochlorite with ultrasonic activation for 30 seconds per canal. Calcium hydroxide was placed as an intracanal medicament with a lentulo spiral, and the tooth was temporized with a sterile sponge and Cavit (3M ESPE, St. Paul, MN, USA). The patient was informed to return in 2 weeks for completion of the root canal.
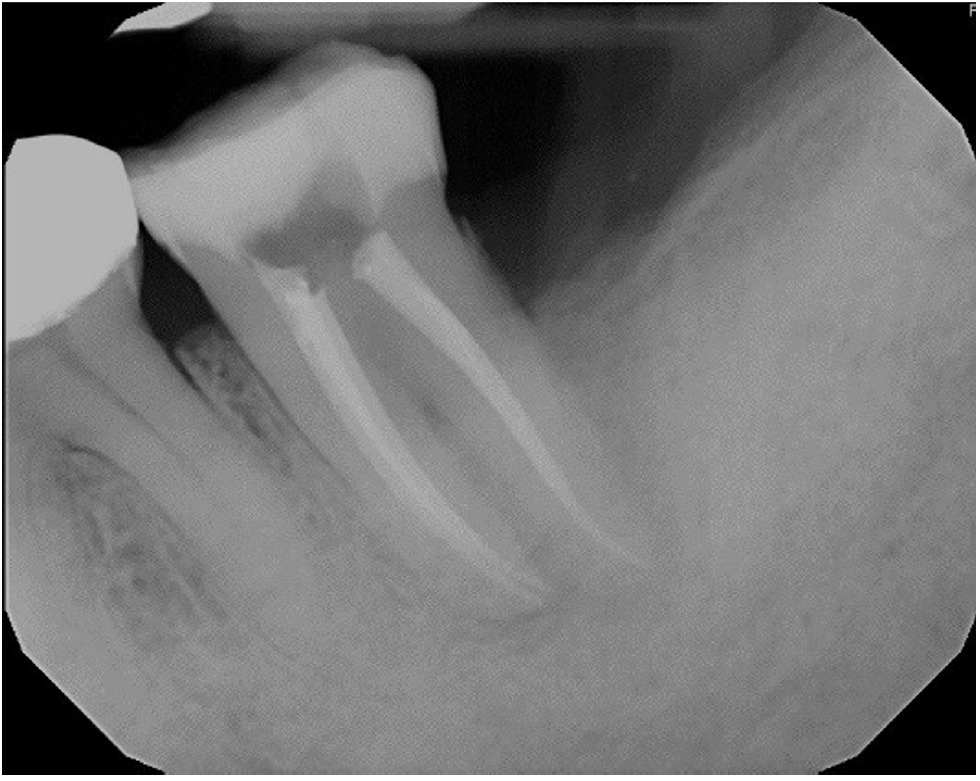
At the 2-week follow-up, the sinus tract had healed. After the same anesthesia and isolation protocol as the first visit, the tooth was accessed through the temporary restoration. Calcium hydroxide was irrigated out with 17% ethylenediaminetetraacetic acid solution, which was ultrasonically activated for 15 seconds in each canal. This was followed by 5% sodium hypochlorite irrigation, which was ultrasonically activated for 15 seconds in each canal, after which cone fit was verified clinically and confirmed with a radiograph (
Figure 3). The canals were then dried with paper points, and obturation was completed using gutta-percha cones and AH Plus sealer (Dentsply DeTrey GmbH, Konstanz, Germany) with the cold lateral condensation technique. The tooth was temporized with a sterile sponge and Cavit (3M ESPE) and a postoperative radiograph was captured (
Figure 4). A referral for periodontal therapy was given to the patient.
The patient reported for the periodontal treatment after 2 months. At this time, periapical radiograph (
Figure 5) indicated reduced periapical radiolucency, but the radiolucency on the distal aspect of the distal root persisted. The tooth was nontender to percussion, but an 11 mm pocket was present along the distal-buccal line angle.
The same protocol of local anesthesia was administered, and a full-thickness flap was raised by placing a sulcular incision with a vertical release mesial to #20 and a crestal incision distal to #18. Scaling and root planing were performed on teeth #18, #19, and #20. The cemental tear fragment was curetted and removed. The surgical site was closed with five interrupted mattress sutures with 4-0 chromic gut sutures. Hemostasis was confirmed. Postoperative instructions were provided, and the patient was scheduled for follow-up visits at 1 month, 3 months, and 9 months.
The patient was lost to follow-up until he reported again at 24 months, at which time clinical examination revealed that a full-coverage restoration on tooth #18 had been placed, restoring form and function (
Figure 6). Clinical gingival health was noted on a reduced periodontium. Draining sinus tract remained resolved, and probing depths were improved to 3–4 mm. The tooth exhibited no mobility. Periapical radiograph (
Figure 7) showed significant resolution of the periapical radiolucency with substantial bone regeneration along the length of the distal root. The patient was greatly appreciative that his natural dentition was conserved, which motivated him to ensure continued dental care maintenance.
DISCUSSION
The successful management of EPLs complicated by cemental tears requires a thorough understanding of their etiology, diagnosis, and contributing factors to treatment success. Cemental tears, though relatively rare, play a significant role in periodontal breakdown and are often misdiagnosed, leading to progressive disease and treatment challenges. Their etiopathogenesis is multifactorial, involving age-related structural changes, occlusal trauma, and periodontal disease, which weaken the attachment between cementum and dentin, resulting in fragmentation [
6,
7]. The prevalence of cemental tears remains low, affecting less than 2% of teeth, with a higher incidence in maxillary and mandibular incisors, particularly on interproximal surfaces [
8]. Their presence can mimic primary periodontal or endodontic lesions, making an accurate differential diagnosis crucial.
Differentiating cemental tears from other endodontic or periodontal pathologies requires a combination of clinical, radiographic, and histologic evaluations. Clinically, cemental tears present as isolated deep periodontal pockets, persistent inflammation despite treatment, and mobility in affected teeth [
2,
7,
9]. Radiographically, a radiopaque fragment adjacent to the root surface, particularly in cases with rapid localized periodontal destruction, should raise suspicion [
9]. Cone-beam computed tomography can enhance diagnostic accuracy, providing detailed three-dimensional imaging of root surfaces and periodontal defects [
10]. In the present case, the presence of a “J-shaped” radiolucency along the distal root and a small radiopaque fragment was suggestive of a cemental tear contributing to the persistent periodontal involvement.
The treatment strategy for EPLs complicated by cemental tears requires a multidisciplinary approach, as endodontic treatment alone is often insufficient. While primary endodontic lesions can typically be resolved with thorough root canal disinfection, intracanal medication, and obturation, cases involving cemental tears necessitate periodontal intervention to remove the fragmented cementum and facilitate healing [
11–
13]. Periodontal therapy, including surgical debridement and root surface conditioning, improves treatment outcomes by reducing pocket depth and promoting periodontal reattachment [
14]. The use of regenerative techniques, such as guided tissue regeneration and biologic mediators, may further enhance periodontal healing in select cases [
6].
Factors contributing to the success of treatment include early diagnosis, complete removal of necrotic cementum, and patient compliance with periodontal maintenance. The ability of periodontal tissues to regenerate is influenced by the severity of attachment loss and bacterial contamination at the affected site [
15]. In this case, the combination of thorough endodontic treatment, surgical removal of the cemental fragment, and postoperative monitoring contributed to significant periodontal improvement and radiographic evidence of bone regeneration. At twenty-four months, probing depths had returned to a healthy range, and the patient was asymptomatic, highlighting the effectiveness of an interdisciplinary approach.
This case underscores the importance of recognizing cemental tears as a potential complicating factor in EPLs. A misdiagnosis or delayed intervention can lead to rapid periodontal deterioration, ultimately resulting in tooth loss [
16]. Advanced imaging modalities, combined with a collaborative approach between endodontists and periodontists, can optimize treatment planning and long-term outcomes [
17]. By increasing awareness of cemental tears and their management, clinicians can improve diagnostic accuracy and enhance treatment success in these challenging cases.
CONCLUSIONS
Effective management of EPLs complicated by cemental tears requires a multidisciplinary approach. Cemental tears, though rare, can complicate diagnosis and treatment, often mimicking other pathologies. This case demonstrates the importance of early diagnosis and intervention, utilizing both endodontic and periodontal therapies to achieve favorable outcomes. Through comprehensive treatment and careful monitoring, significant improvement in periodontal health and bone regeneration was achieved. Recognizing cemental tears as a complicating factor in EPLs can help clinicians improve diagnostic accuracy and treatment success in these complex cases.
-
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
-
FUNDING/SUPPORT
The authors have no financial relationships relevant to this article to disclose.
-
ACKNOWLEDGMENTS
The authors would like to acknowledge the contributions of Dr. Craig Dunlap with manuscript preparation, Dr. Justine Fong for guiding endodontic management, and Dr. Gary Grill for performing the periodontal surgery in the clinical management of this case at the University of the Pacific Arthur A. Dugoni School of Dentistry, San Francisco, CA, USA.
-
AUTHOR CONTRIBUTIONS
Conceptualization, Supervision: Oza S. Data curation, Methodology: Sadhak ND. Software: Pallod A. Writing - original draft: Sadhak ND, Pallod A. Writing - review & editing: Oza S. All authors read and approved the final manuscript.
-
DATA SHARING STATEMENT
The datasets are not publicly available but are available from the corresponding author upon reasonable request.
Figure 1.“J-shaped” lesion observed along the distal root of #18 (yellow arrow). A radiopaque fragment, consistent with a cemental tear, was identified along the distal root surface (red arrow).
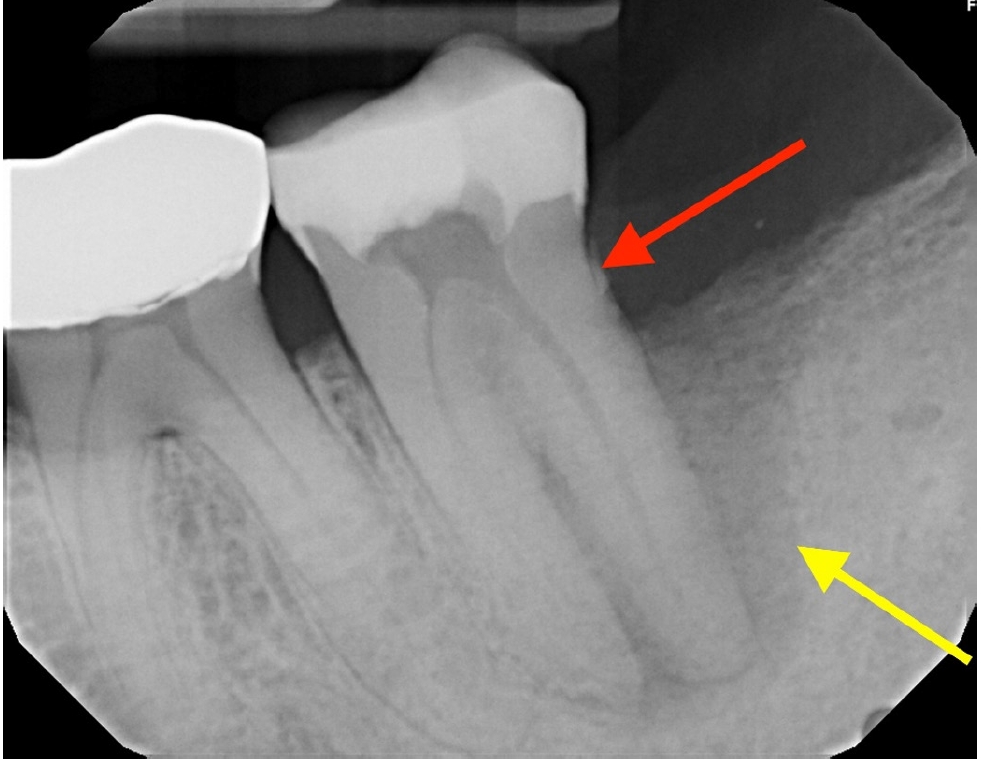
Figure 2.Working length radiograph showing radiopaque fragment consistent with a cemental tear along distal root (red arrow).
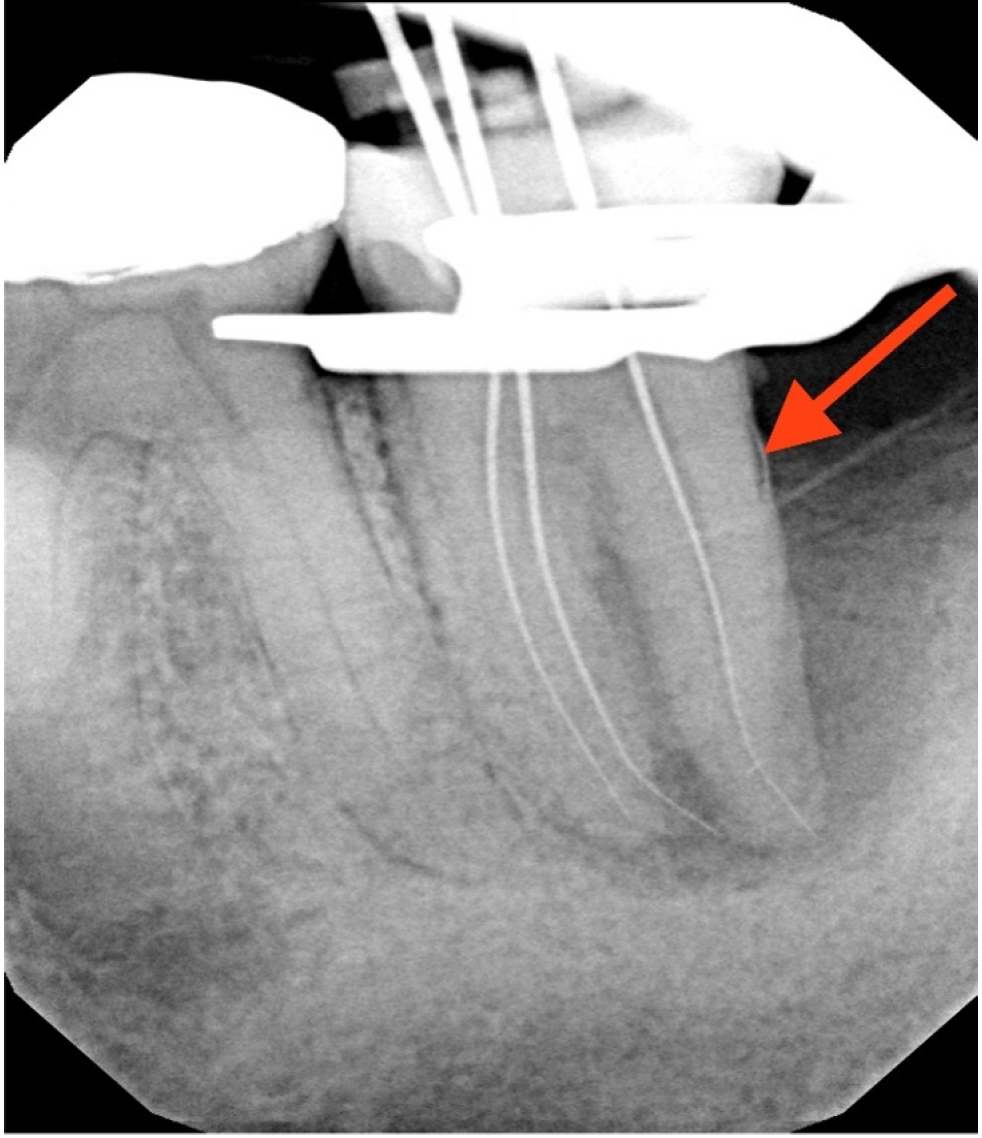
Figure 3.

Figure 4.Immediate postoperative radiograph.

Figure 5.Periapical radiograph at 2 months indicating reduced size of periapical radiolucency and persistent radiolucency along the distal aspect of the distal root.
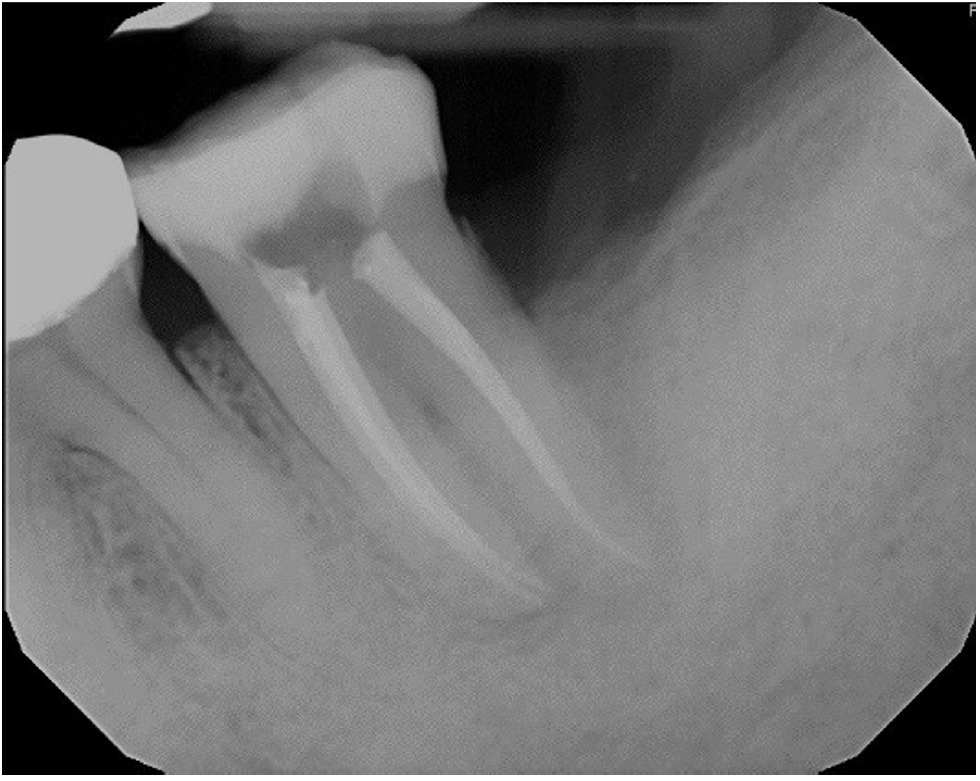
Figure 6.Twenty-four-month recall showing that the tooth has been restored with an extracoronal restoration and absence of draining sinus tract. Gingival health on a reduced periodontium is noted.

Figure 7.Periapical radiograph showed significant resolution of the periapical radiolucency with substantial bone regeneration along the length of the distal root.

Table 1.Endodontic sensibility testing chart
|
Test |
Tooth number
|
|
#18 |
#19 |
#20 |
#31 |
#15 |
|
Cold |
– |
+ |
+ |
+ |
+ |
|
Percussion |
++ |
– |
– |
– |
– |
|
Palpation |
++ |
– |
– |
– |
– |
|
Periodontal probing |
B: 3, 4, 12 |
B: 3, 3, 3 |
B: 3, 2, 3 |
B: 4, 3, 3 |
B: 3, 3, 4 |
|
L: 3, 4, 6 |
L: 3, 3, 3 |
L: 3, 2, 3 |
L: 3, 3, 3 |
L: 3, 3, 3 |
|
Mobility*
|
I |
I |
I |
I |
I |
REFERENCES
- 1. Chen B, Zhu Y, Lin M, Zhang Y, Li Y, Ouyang X, et al. Expert consensus on the diagnosis and therapy of endo-periodontal lesions. Int J Oral Sci 2024;16:55.ArticlePubMedPMCPDF
- 2. Lee AH, Neelakantan P, Dummer PM, Zhang C. Cemental tear: literature review, proposed classification and recommendations for treatment. Int Endod J 2021;54:2044-2073.ArticlePubMedPDF
- 3. Chawla A, Kumar V. Cemental tear: an unusual cause for persisting endodontic periodontal lesion. Indian J Dent Res 2019;30:140-143.ArticlePubMed
- 4. Ordinola-Zapata R, Crepps J, Clarke B. Endodontic-periodontic lesions [Internet]. Chicago: American Association of Endodontists; 2024 [cited 2025 Feb 16]. Available from: https://www.aae.org/specialty/endodontic-periodontic-lesions/
- 5. Tayal A, Ghosh S, Adhikari HD, Ghosh A. Management of an endo-perio lesion: a multidisciplinary approach. IP Indian J Conserv Endod 2021;6:171-175.Article
- 6. Andreasen FM, Andreasen JO, Bayer T. Prognosis of root-fractured permanent incisors--prediction of healing modalities. Endod Dent Traumatol 1989;5:11-22.ArticlePubMed
- 7. Leknes KN, Lie T, Selvig KA. Cemental tear: a risk factor in periodontal attachment loss. J Periodontol 1996;67:583-588.ArticlePubMed
- 8. Lin HJ, Chan CP, Yang CY, Wu CT, Tsai YL, Huang CC, et al. Cemental tear: clinical characteristics and its predisposing factors. J Endod 2011;37:611-618.ArticlePubMed
- 9. Haney JM, Leknes KN, Lie T, Selvig KA, Wikesjö UM. Cemental tear related to rapid periodontal breakdown: a case report. J Periodontol 1992;63:220-224.
- 10. Misch KA, Yi ES, Sarment DP. Accuracy of cone beam computed tomography for periodontal defect measurements. J Periodontol 2006;77:1261-1266.ArticlePubMed
- 11. Ricucci D, Siqueira JF, Bate AL, Pitt Ford TR. Histologic investigation of root canal-treated teeth with apical periodontitis: a retrospective study from twenty-four patients. J Endod 2009;35:493-502.ArticlePubMed
- 12. Lee JH, Kim YT. Periodontal regenerative treatment for maxillary anterior cemental tears: a mid-term cohort study. J Periodontol 2025 Jul 8 [Epub]. https://doi.org/10.1002/jper.11377.
- 13. Jeng PY, Luzi AL, Pitarch RM, Chang MC, Wu YH, Jeng JH, et al. Cemental tear: to know what we have neglected in dental practice. J Formos Med Assoc 2018;117:261-267.ArticlePubMed
- 14. Sculean A, Gruber R, Bosshardt DD. Soft tissue wound healing around teeth and dental implants. J Clin Periodontol 2014;41 Suppl 15:S6-S22.ArticlePubMedPDF
- 15. Mota de Almeida FJ, Arespång A. Cemental tear - a series of 14 cases of surgical periodontal treatments with a follow-up of up to ten years. Br Dent J 2025;238:793-796.ArticlePubMedPDF
- 16. Heithersay GS. Clinical, radiologic, and histopathologic features of invasive cervical resorption. Quintessence Int 1999;30:27-37.PubMed
- 17. Tsesis I, Rosen E, Tamse A, Taschieri S, Kfir A. Diagnosis of vertical root fractures in endodontically treated teeth based on clinical and radiographic indices: a systematic review. J Endod 2010;36:1455-1458.ArticlePubMed
 , Akshaya Pallod2
, Akshaya Pallod2 , Shreyas Oza3,*
, Shreyas Oza3,*








 KACD
KACD


 ePub Link
ePub Link Cite
Cite

