Abstract
-
Objectives
This study aims to correlate caries-causing microorganism load, lactic acid estimation, and blood groups to high caries risk in diabetic and non-diabetic individuals and low caries risk in healthy individuals.
-
Materials and Methods
This study includes 30 participants divided into 3 groups: Group A, High-risk caries diabetic individuals; Group B, High-risk caries non-diabetic individuals; and Group C, Low-risk caries individuals. The medical condition, oral hygiene, and caries risk assessment (American Dental Association classification and International Caries Detection and Assessment System scoring) were documented. Each individual’s 3 mL of saliva was analyzed for microbial load and lactic acid as follows: Part I: 2 mL for microbial quantity estimation using nutrient agar and blood agar medium, biochemical investigation, and carbohydrate fermentation tests; Part II: 0.5 mL for lactic acid estimation using spectrophotometric analysis. Among the selected individuals, blood group correlation was assessed. The χ2 test, Kruskal-Wallis test, and post hoc analysis were done using Dunn’s test (p < 0.05).
-
Results
Group A had the highest microbial load and lactic acid concentration, followed by Groups B and C. The predominant bacteria were Lactobacilli (63.00 ± 15.49) and Streptococcus mutans (76.00 ± 13.90) in saliva. Blood Group B is prevalent in diabetic and non-diabetic high-risk caries patients but statistically insignificant.
-
Conclusions
Diabetic individuals are more susceptible to dental caries due to high microbial loads and increased lactic acid production. These factors also lower the executing tendency of neutrophils, which accelerates microbial accumulation and increases the risk of caries in diabetic individuals.
-
Keywords: Diabetes; Dental caries; Microbial load; Lactobacillus; Streptococcus mutans; Lactic acid
INTRODUCTION
Cariogenic microbes colonize the dental biofilm early in life and can eventually grow to cause disease under favorable environmental conditions [
1]. The
Actinomycetes spp.,
Streptococcus mutans, and
Lactobacillus spp. Were the important bacterial species overabundant in the caries active community [
2].
Saliva plays a crucial role in influencing tooth surface sensitivity to dietary carbohydrates and plaque acidity, as well as the microbial composition and reduction of dental plaque pH and cariogenic ability.
S. mutans and
Streptococcus sorbinus have been isolated in higher proportions in such conditions compared to a healthy oral cavity. The original “ecological plaque hypothesis” recognized bacterial function (tolerance of acidic conditions and rapid acid production) and the importance of caries contributing to the environment (low salivary flow and a sugar-rich diet) [
3].
Lactobacilli can be reliably isolated from human caries lesions but are not associated with disease initiation. Many
Lactobacillus species can be identified from carious lesions prevalent elsewhere in the body and fermented foods [
3,
4].
Globally, more than 500 million people have diabetes, which affects men, women, and children of all ages in every nation. In the next 30 years, this figure is expected to more than double to 1.3 billion people, with a rise in every nation [
5]. Diabetes mellitus (DM) affects the metabolism of fat, carbohydrates, and protein. A study has demonstrated that caries indicators, such as decreased salivary flow and increased
S. mutans counts, may be correlated with DM metabolic regulation and affect caries progression [
6]. Diabetes reduces the amount of bicarbonate in all body fluids, resulting in metabolic acidosis and acidic saliva [
7]. Hypothetically, elevated glucose levels in serum and gingival crevicular fluid could stimulate the growth of gram-positive fermenting bacteria such as
Lactobacilli,
Streptococci, and
Actinomycetes [
8].
Even though many bacteria use ABO-specific surface lectins to bind to body surfaces, ABO antigens in saliva may inhibit bacteria’s ability to attach to tooth surfaces [
9]. Dental caries, salivary gland tumors, chickenpox, malaria, oral cancer, hematological malignancies, ischemic heart disease, and cholera significantly correlate with the ABO blood group, as determined by researchers in India and the West [
10,
11,
12,
13]. Regarding the DM associated with blood groups, there is a lack of research evidence. This study therefore correlates the presence of caries-causing microorganisms, lactic acid production, and blood group with high-risk caries in diabetic and non-diabetic individuals and with low-risk caries in healthy individuals.
MATERIALS AND METHODS
The ethics committee of the Institute of Medical Sciences (IMS) & SUM Hospital authorized the study with reference number DRI/IMS.SH/SOA/18131/2020. All participants gave their signed agreement after receiving information (in both English and Odia).
A total of 180 individuals aged 20 to 60 years old who visited the department were screened for the study. Thirty individuals (
n = 10 in each group) were divided into 3 groups based on the caries risk assessment (American Dental Association classification and International Caries Detection and Assessment System scoring). Group A, High-risk caries diabetic individuals (
Table 1), Group B, High-risk caries non-diabetic individuals, and Group C, Low-risk caries healthy individuals (control group) who met the inclusion criteria (high-risk caries diabetic patients, high-risk caries non-diabetic patients, and low-risk caries patients) and exclusion criteria (any other systemic disease other than diabetes; patients having bleeding disorders; chronic systemic conditions; hormonal disorders; under fluoride therapy; and with medication that affects salivary flow rate).
Table 1 Biochemical characterization and sugar fermentation tests for the isolated organisms
|
Biochemical characteristics |
S. mutans
|
Lactobacillus spp. |
S. pyogenes
|
|
Capsule |
+VE |
−VE |
+VE |
|
Catalase |
−VE |
−VE |
−VE |
|
Oxidase |
−VE |
−VE |
−VE |
|
Indole |
−VE |
−VE |
−VE |
|
Methyl red |
−VE |
−VE |
+VE |
|
Voges-Proskauer |
+VE |
−VE |
−VE |
|
Citrate |
+VE |
−VE |
−VE |
|
Urease |
−VE |
−VE |
−VE |
|
Motility |
+VE |
−VE |
−VE |
|
Sugar fermentation tests |
|
|
|
|
Arabinose |
−VE |
+VE |
−VE |
|
Galactose |
+VE |
+VE |
+VE |
|
Glucose |
+VE |
+VE |
+VE |
|
Lactose |
+VE |
+VE |
+VE |
|
Maltose |
+VE |
+VE |
+VE |
|
Mannitol |
+VE |
−VE |
+VE |
|
Starch |
−VE |
+VE |
+VE |
|
Sucrose |
+VE |
+VE |
+VE |
After 30 minutes of eating, 3 mL of unstimulated saliva was collected from each participant and stored in independent vials. Each sample was divided into 2 parts (Part I: 2 mL for microbiological and biochemical investigation and Part II: 0.5 mL for lactic acid estimation).
Microbial and biochemical analysis
Saliva samples (2 mL) were stored in sealed containers at 37°C for 48 hours. Plates of nutrient agar and blood agar were used to cultivate microorganisms. The bacterial population was counted using a nutrient agar (NA) medium and a pour plate technique. An accurate colony counter was used to determine the total number of bacteria.
To detect the presence of cariogenic
S. mutans and
Lactobacillus species, the mixed bacterial culture was then streaked on blood agar and nutrient agar. Randomly selected colonies from plates were re-streaked on individual nutrient agar slants using a sterile loop. The nutrient agar slants were incubated for 24 hours at 37°C and then stored for future use [
14,
15].
Initially, isolated bacteria were identified through morphological features. Color, reverse side color, cell, and spore shape (if present) were among the fundamental tests included. Bacteria were further identified by performing Gram and capsule staining on all samples. To prevent cross-contamination, the following biochemical tests were performed in succession on pure cultures of isolated bacteria: catalase, oxidase, indole, methyl red (MR) test, Voges-Proskauer (VP), citrate, urease, motility, and carbohydrate fermentation tests. (
Table 2) [
16,
17]
Table 2Comparison of an average number of colonies on nutrient agar between the groups
|
Groups |
No. |
Mean |
SD |
SE |
Min |
Max |
F-value |
p value*
|
|
Group A |
10 |
63.00 |
15.49 |
4.89 |
40.00 |
80.00 |
24.685 |
< 0.001†
|
|
Group B |
10 |
33.50 |
9.44 |
2.98 |
20.00 |
50.00 |
|
|
|
Group C |
10 |
5.30 |
2.11 |
0.66 |
2.00 |
10.00 |
|
|
Spectrophotometric determination of salivary lactate
Sigma’s spectrophotometric lactic acid assay kit 826UV was utilized. Each reaction required 0.5 mL of saliva, which was then diluted, and the concentration was multiplied by the dilution factor to attain the final concentration. To make the saliva sample ready for estimation, first, it was centrifuged for 10 minutes at 13,000 rpm to remove any debris, and then it was deproteinized with a 10 kDa MWCO spin filter to remove lactate dehydrogenase.
Assay reaction: 500 µL of the master reaction mixture was added to 500 µL of saliva and incubated at room temperature in the dark for 30 minutes. After incubation, the optical density was measured at 570 nm against a blank without lactate. All readings must subtract background values. The amount of lactate was measured against a standard curve. The concentration of lactate is calculated as:
where Sa represents amount of lactic acid in an unknown sample (N mole) from the standard curve, Sv the sample volume (µL), and C the lactate concentration in the sample.
Blood group analysis
Participants in the study underwent blood group analysis. The database included patients who could provide an ABO blood group. The blood types of uncertain individuals were determined using microplate agglutination.
Statistical analysis
Descriptive and analytical Statistical analysis was done using Statistical Package for Social Sciences version 24.0 (IBM Corporation, Chicago, IL, USA). The χ2 test was used to check the distribution of microbial colonies in nutrient agar and blood agar for differences in proportions and blood group analysis. Continuous variables were expressed as the mean and standard deviation. The normality of continuous data was analyzed by the Shapiro-Wilk test. The Kruskal-Wallis test was used to compare the average number of colonies in nutrient agar and blood agar, lactic acid concentration and mean differences among the groups. Post hoc analysis was done using Dunn’s test. The level of significance was kept at p < 0.05.
RESULTS
The mean age of Group A participants was 50.40 ± 6.91 years, Group B: 46.50 ± 8.50 years, and Group C: 48.20 ± 7.22 years. All samples showed 100% bacterial growth on nutrient and blood agar; gram staining revealed long rods and positive cocci. According to biochemical analysis,
S. mutans,
Lactobacillus spp., and
Streptococcus pyogenes were positive for features and sugar fermentation tests, as in
Table 1. The Kruskal-Wallis’s test showed significant differences (
p < 0.001) in the mean number of colonies on nutrient and blood agar. The distribution of
Lactobacillus was major identifiable colonies on nutrient agar: Group A (63.00 ± 15.49) had more colonies than Group B (33.50 ± 9.44) and Group C had the least colonies (5.300 ± 2.11). When Group A was compared with Group C, a mean difference of 57.70 (95% CI, 46.00–69.39) was found which was statistically significant (
p < 0.001). When Group B was compared with Group C, a mean difference of 28.20 (95% CI, 16.50–39.89) was found which was statistically significant (
p < 0.001). The comparison between Group A was compared with Group B did not show significant differences (
p = 0.697) (
Table 2).
On blood agar, the distribution of samples based on the presence of major identifiable colonies (
S. mutans and
S. pyogenes): Group A (76.00 ± 13.90) showed increased colonies than Group B (34.00 ± 11.25). The control group had the least number of colonies on blood agar (5.70 ± 1.41). The
post hoc pairwise comparative analysis by Dunn’s test showed significant differences in the average number of colonies on blood agar among the 3 groups. All 3 groups showed significant differences (
p < 0.05) in the mean number of colonies on blood agar compared to each other (
Table 3).
Table 3 Comparison of an average number of colonies on blood agar between the groups
|
Groups |
No. |
Mean |
SD |
SE |
Min |
Max |
Z-value |
p value*
|
|
Group A |
10 |
76.00 |
13.90 |
4.39 |
55.00 |
100.00 |
25.893 |
< 0.001†
|
|
Group B |
10 |
34.00 |
11.25 |
3.55 |
20.00 |
50.00 |
|
|
|
Group C |
10 |
5.70 |
1.41 |
0.44 |
4.00 |
8.00 |
|
|
The Kruskal-Wallis test showed significant differences (
p < 0.001) in mean lactic acid concentration. Group A (0.1308 ± 0.0162) had the highest mean lactic acid concentration, followed by Group B (0.0682 ± 0.0122). The control group had the least mean lactic acid concentration (0.0272 ± 0.0116). The
post hoc pairwise comparative analysis by Dunn’s test showed significant differences in mean lactic acid concentration among the 3 groups. There were statistically significant differences (
p < 0.05) in the mean lactic acid concentration between the 3 groups (
Table 4).
Table 4 Comparison of mean lactic acid concentration between the groups
|
Groups |
No. |
Mean |
SD |
SE |
Min |
Max |
F-value |
p value*
|
|
Group A |
10 |
0.1308 |
0.0162 |
0.0051 |
0.1007 |
0.1646 |
25.835 |
< 0.001†
|
|
Group B |
10 |
0.0682 |
0.0122 |
0.0038 |
0.0539 |
0.0880 |
|
|
|
Group C |
10 |
0.0272 |
0.0116 |
0.0003 |
0.0071 |
0.0416 |
|
|
In Group A: there were 3 (30.0%) with Blood Group A, 6 (60.0%) with Blood Group B and 1 (10.0%) with Blood Group O; in Group B: there were 3 (30.0%) with Blood Group A, 5 (50.0%) with Blood Group B and 1 (20.0%) with Blood Group O; Group C: there were 3 (30.0%) with Blood Group A, 4 (40.0%) with Blood Group B and 3 (30.0%) with Blood Group O. The χ2 test showed no significant differences (p = 0.844) in blood group proportions among the 3 study groups.
DISCUSSION
In this study, diabetic individuals had an alarmingly high rate of dental caries. Hyperglycaemia reduces salivation, a characteristic of uncontrolled diabetes. During this time, the precipitation of glucose in the oral cavity can promote the growth of acidic and acidogenic bacteria and caries lesions [
10,
13].
Jones highlighted the potential risk of caries related to DM [
18], which was congruent with our findings, as we observed significantly higher caries risk assessment scores in groups A and B than in group C. Higher blood sugar levels were also associated with a higher
S. mutans and
Lactobacilli count in the study population, indicating a higher risk of dental caries [
13,
19]. Decreased saliva secretion increases the risk of caries. However, superior metabolic control prevents harmful salivary changes, such as increased glucose content and lower pH, and a fiber-rich, simple-carbohydrate-restricted diabetic diet can delay plaque formation and the spread of acidogenic bacterial microorganisms [
20,
21,
22].
Twetman
et al. [
23] noticed that throughout the trial, people with diabetes with poor metabolic control developed 3 times as many lesions as those with excellent metabolic control, corroborating our findings that increased blood sugar levels led to greater
S. mutans counts. Studies indicate that people with diabetes are more prone to dental caries than non-diabetics because of their high salivary glucose levels and reduced neutrophil execution, accelerating microbial accumulation on teeth [
24,
25]. Diabetics’ saliva contains more microorganisms, such as
S. mutans,
S. pyogenes, and
Lactobacilli. This study identified the abovementioned microbes by colony characteristics, biochemical assays, and sugar fermentation tests as predominating in their respective groups. The mean number of colonies on nutrient and blood agar was significantly different (
p < 0.001) between the 3 groups. Group A had more colonies than B.
Individuals with type 1 diabetes had a higher concentration of
S. mutans in their saliva (>105 CFU/ml) than children without diabetes (control) [
26]. An increase in the glucose content of oral fluid promotes the growth of
S. mutans and
Lactobacilli, which increases the frequency and duration of acid attacks. Based on the severity of carious lesions,
Lactobacillus species are linked to dental caries, lending credence to the theory that certain
Lactobacilli are linked to the progression of dental caries. [
2].
In the present study, the mean lactic acid concentration in the 3 groups exhibited significant variations (
p < 0.001). Group A (0.1308 ± 0.0162) had the highest lactic acid concentration, followed by Group B (0.0682 ± 0.0122). The Control group had the lowest mean lactic acid levels (0.0272 ± 0.0116). The correlation between bacteria and lactic acid generation has been shown (
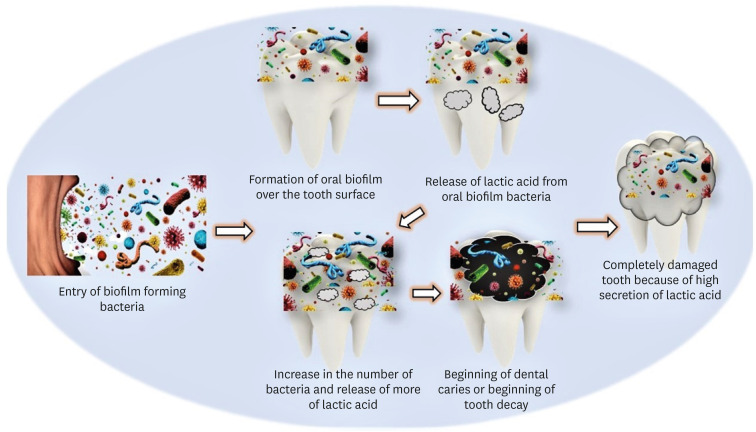
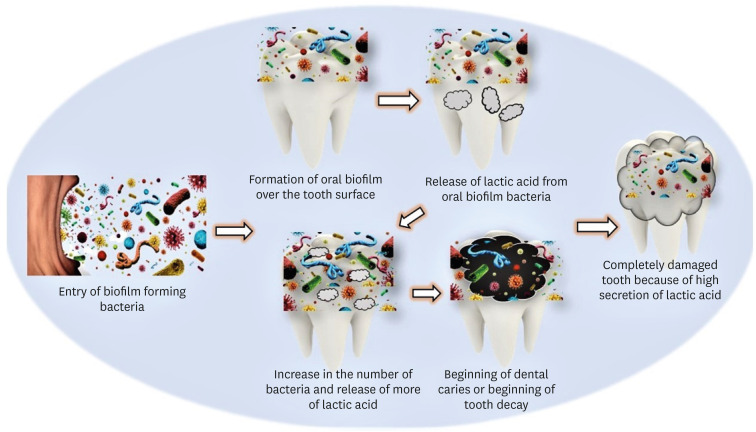
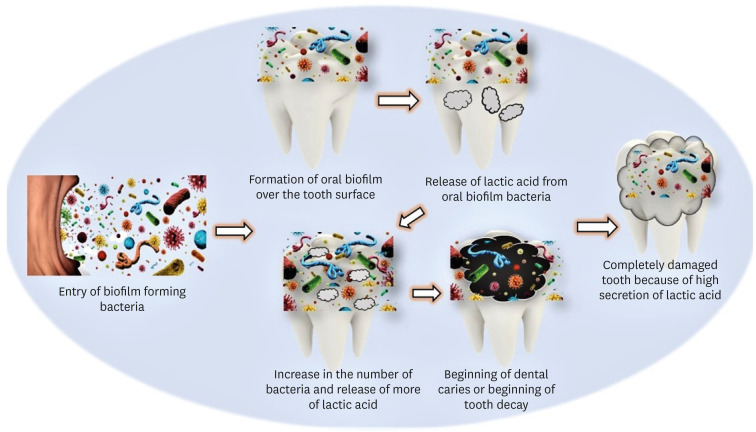
Figure 1). Pathogenic bacteria generally enter the oral cavity to form biofilm over the tooth surface. In the absence of oxygen, bacteria respire anaerobically, producing lactic acid. This over-secretion of lactic acid slowly corrodes the tooth's outer hard surface, leading to dental caries or tooth loss [
27].
Lactobacillus’ cariogenicity may be associated with sugar-fermented lactic acid. Several investigations have demonstrated that
Lactobacillus is an acid-tolerant bacteria that can survive at pH levels below 4.5. They shift the oral pH from neutral to acidic. During caries colonization and maturation, they adhere to dental plaque and dematerialize tooth enamel [
28,
29].
Figure 1 Pathogenic bacteria generally enter the oral cavity to form biofilm over the tooth surface. In the absence of oxygen, bacteria respire anaerobically, producing lactic acid. This over-secretion of lactic acid slowly corrodes the tooth's outer hard surface, leading to dental caries or tooth loss.
This research supports the concept that Lactobacilli colonizing the oral cavity are opportunistic invaders of pre-caries or existing caries lesions. Lactobacilli colonize teeth as they enter the mouth, particularly fissured primary molars and teeth with surface defects or enamel hypoplasia. Pre-caries lesions are caused when
S. mutans and other acidogenic bacteria demineralize enamel in the presence of fermentable carbohydrates [
30].
The current study found no statistically significant variations or differences in blood group proportions between the 3 groups. However, blood Group B had more occurrence in diabetic and non-diabetic high-risk caries individuals. The association between blood groups and dental caries can be explained by the fact that blood group entities synthesized in saliva can cause microorganisms to aggregate and be eliminated from the oral cavity. Bacteria like these use lectins, many of which are ABO (h)-specific, present on their surfaces to adhere to body surfaces. ABO (h) antigens are secreted into saliva, preventing microorganisms from adhering to tooth surfaces [
11]. High-molecular-weight parotid saliva agglutinins and similar proteins in submandibular-sublingual saliva help
S. mutans adhere. In the liquid phase, these proteins promote bacterial aggregation and oral cavity clearance [
9,
29]. Other carbohydrates and blood group-specific sugars prevent bacterial aggregation. In contrast to D-galactose and D-fructose, specific to Blood Groups B and O, respectively, GalNAc, a sugar specific to Blood Group A, prevented bacterial aggregation in saliva [
9]. This may explain the correlation between blood group, secretor status, and dental caries [
31]. Again, since the sample population was small, the findings should not be deduced to the entire population, and further research is needed.
CONCLUSIONS
This research reports that diabetes individuals are susceptible to caries due to an increased microbial load and lactic acid production. High salivary glucose promotes microorganism growth and tooth surface accumulation. Blood Group B is prevalent in diabetic and non-diabetic high-risk caries patients.
ACKNOWLEDGEMENTS
We appreciate the substantial assistance from the “Department of Conservative Dentistry and Endodontics, Institute of Dental Sciences, Siksha ‘O’ Anusandhan, (deemed to be) University”.
-
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
-
Author Contributions:
Conceptualization: Govind S.
Data curation: Mohanty M.
Formal analysis: Mohanty M.
Investigation: Rath S.
Methodology: Govind S.
Validation: Rath S.
Writing - original draft: Govind S.
Writing - review & editing: Mohanty M, Govind S, Rath S.
REFERENCES
- 1. Scanlan CA, Rahmani H, Bowles R, Bennamoun M. Three-dimensional scanning for measurement of bulk density in gravelly soils. Soil Use Manage 2018;34:380-387.ArticlePDF
- 2. van Houte J. Role of micro-organisms in caries etiology. J Dent Res 1994;73:672-681.ArticlePubMedPDF
- 3. Byun R, Nadkarni MA, Chhour KL, Martin FE, Jacques NA, Hunter N. Quantitative analysis of diverse Lactobacillus species present in advanced dental caries. J Clin Microbiol 2004;42:3128-3136.ArticlePubMedPMCPDF
- 4. Chhour KL, Nadkarni MA, Byun R, Martin FE, Jacques NA, Hunter N. Molecular analysis of microbial diversity in advanced caries. J Clin Microbiol 2005;43:843-849.ArticlePubMedPMCPDF
- 5. The Lancet. Diabetes: a defining disease of the 21st century. Lancet 2023;401:2087.ArticlePubMed
- 6. Mohanty S, Mohanty N, Rath S. Analysis of oral health complications in diabetic patients—a diagnostic perspective. J Oral Res 2018;7:278-281.Article
- 7. K M P, Johnson P, Ganesh M, Subhashini AS. Evaluation of salivary profile among adult type 2 diabetes mellitus patients in South India. J Clin Diagn Res 2013;7:1592-1595.PubMedPMC
- 8. Sibyl S, Bennadi D, Kshetrimayum N, Manjunath M. Correlations between gingival crevicular blood glucose and capillary blood glucose: a preliminary report. J Lab Physicians 2017;9:260-263.ArticlePubMedPMC
- 9. Mazumdar P, Das UK, Goswami S. Correlation between blood group and dental caries in 20-60 years age group: a study. Int J Adv Res 2014;2:413-424.
- 10. Orbak R, Simsek S, Orbak Z, Kavrut F, Colak M. The influence of type-1 diabetes mellitus on dentition and oral health in children and adolescents. Yonsei Med J 2008;49:357-365.ArticlePubMedPMC
- 11. Singla S, Verma A, Goyal S, Singla I, Shetty A. Correlation of dental caries and blood group in Western Punjab population in India. Indian J Multidiscip Dent 2015;5:59.Article
- 12. Demir T, Tezel A, Orbak R, Eltas A, Kara C, Kavrut F. The effect of ABO blood types on periodontal status. Eur J Dent 2007;1:139-143.ArticlePubMedPMC
- 13. Goyal D, Kaur H, Jawanda MK, Verma S, Parhar S. Salivary pH and dental caries in diabetes mellitus. Int J Oral Maxillofac Pathol 2012;3:13-17.
- 14. Mondal DP, Panda CS, Rath S, Mohanty N. Comparative study on the efficacy of advanced and conventional methods for detection of Streptococcus mutans in the saliva of dental caries patients. Indian J Public Health Res Dev 2018;9:6-10.
- 15. Alghamdi S. Isolation and identification of the oral bacteria and their characterization for bacteriocin production in the oral cavity. Saudi J Biol Sci 2022;29:318-323.ArticlePubMedPMC
- 16. Shklair IL, Keene HJ. A biochemical scheme for the separation of the five varieties of Streptococcus mutans
. Arch Oral Biol 1974;19:1079-1081.PubMed
- 17. Ahirwar SS, Gupta MK, Gupta G, Singh V. Screening, isolation and identification of Lactobacillus species from dental caries of children. Int J Curr Microbiol Appl Sci 2017;6:497-503.
- 18. Jones RB, McCallum RM, Kay EJ, Kirkin V, McDonald P. Oral health and oral health behaviour in a population of diabetic outpatient clinic attenders. Community Dent Oral Epidemiol 1992;20:204-207.ArticlePubMed
- 19. Seethalakshmi C, Reddy RC, Asifa N, Prabhu S. Correlation of salivary pH, incidence of dental caries and periodontal status in diabetes mellitus patients: a cross-sectional study. J Clin Diagn Res 2016;10:ZC12-ZC14.ArticlePubMedPMC
- 20. Moore PA, Guggenheimer J, Etzel KR, Weyant RJ, Orchard T. Type 1 diabetes mellitus, xerostomia, and salivary flow rates. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001;92:281-291.ArticlePubMed
- 21. Taylor GW, Manz MC, Borgnakke WS. Diabetes, periodontal diseases, dental caries, and tooth loss: a review of the literature. Compend Contin Educ Dent 2004;25:179-184. 186-188. 190.PubMed
- 22. Shiferaw A, Alem G, Tsehay M, Kibret GD. Dental caries and associated factors among diabetic and nondiabetic adult patients attending Bichena Primary Hospital’s Outpatient Department. Front Oral Health 2022;3:938405.ArticlePubMedPMC
- 23. Twetman S, Petersson GH, Bratthall D. Caries risk assessment as a predictor of metabolic control in young type 1 diabetics. Diabet Med 2005;22:312-315.ArticlePubMed
- 24. Moin M, Malik A. Frequency of dental caries and level of risk among type II diabetics. Dentistry (Loma Linda) 2015;5:1000334.
- 25. Malicka B, Kaczmarek U, Ziętek M. Dental caries in adult patients with type 1 and 2 diabetes mellitus. J Stomatol (Brux) 2011;64:9-24.
- 26. Swanljung O, Meurman JH, Torkko H, Sandholm L, Kaprio E, Mäenpää J. Caries and saliva in 12-18-year-old diabetics and controls. Scand J Dent Res 1992;100:310-313.ArticlePubMed
- 27. Rath S, Bal SCB, Dubey D. Oral biofilm: development mechanism, multidrug resistance, and their effective management with novel techniques. Rambam Maimonides Med J 2021;12:e0004.ArticlePubMedPMC
- 28. Ahirwar SS, Gupta MK, Snehi SK. Dental caries and Lactobacillus: role and ecology in the oral cavity. Int J Pharm Sci Res 2019;10:4818-4829.
- 29. Caufield PW, Schön CN, Saraithong P, Li Y, Argimón S. Oral lactobacilli and dental caries: a model for niche adaptation in humans. J Dent Res 2015;94(Supplement):110S-118S.ArticlePubMedPMCPDF
- 30. Sabharwal A, Stellrecht E, Scannapieco FA. Associations between dental caries and systemic diseases: a scoping review. BMC Oral Health 2021;21:472.ArticlePubMedPMCPDF
- 31. Ligtenberg AJ, Veerman EC, de Graaff J, Nieuw Amerongen AV. Influence of the blood group reactive substances in saliva on the aggregation of Streptococcus rattus
. Antonie van Leeuwenhoek 1990;57:97-107.ArticlePubMedPDF
 , Shashirekha Govind2
, Shashirekha Govind2 , Shakti Rath3
, Shakti Rath3


 KACD
KACD
 ePub Link
ePub Link Cite
Cite

