Articles
- Page Path
- HOME > Restor Dent Endod > Volume 48(4); 2023 > Article
- Review Article Disinfectant effectiveness of chlorhexidine gel compared to sodium hypochlorite: a systematic review with meta-analysis
-
Theodoro Weissheimer1
 , Karem Paula Pinto2
, Karem Paula Pinto2 , Emmanuel João Nogueira Leal da Silva2,3
, Emmanuel João Nogueira Leal da Silva2,3 , Lina Naomi Hashizume4
, Lina Naomi Hashizume4 , Ricardo Abreu da Rosa1
, Ricardo Abreu da Rosa1 , Marcus Vinicius Reis Só1
, Marcus Vinicius Reis Só1
-
Restor Dent Endod 2023;48(4):e37.
DOI: https://doi.org/10.5395/rde.2023.48.e37
Published online: October 26, 2023
1Department of Endodontics, School of Dentistry, Federal University of Rio Grande do Sul (UFRGS), Porto Alegre, RS, Brazil.
2Department of Endodontics, School of Dentistry, Rio de Janeiro State University (UERJ), Rio de Janeiro, RJ, Brazil.
3Department of Endodontics, School of Dentistry, Grande Rio University (UNIGRANRIO), Rio de Janeiro, RJ, Brazil.
4Department of Preventive and Social Dentistry, Federal University of Rio Grande do Sul (UFRGS), Porto Alegre, RS, Brazil.
- Correspondence to Theodoro Weissheimer, DDS, MSc. Department of Endodontics, School of Dentistry, Federal University of Rio Grande do Sul (UFRGS), 2492 Ramiro Barcelos Street, Porto Alegre, RS 90035-003, Brazil. theodoro.theo@hotmail.com
Copyright © 2023. The Korean Academy of Conservative Dentistry
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
- This study aimed to compare the disinfectant ability of chlorhexidine (CHX) gel and sodium hypochlorite (NaOCl). Systematic searches were conducted from inception until December 8th, 2022 (MEDLINE/PubMed, Cochrane Library, Web of Science, Scopus, Embase, and Grey Literature databases). Only randomized clinical trials were included. The revised Cochrane risk of bias tools for randomized trials were used to assess the quality of studies. Meta-analyses were performed. The overall quality of evidence was assessed through the Grading of Recommendations Assessment, Development, and Evaluation tool. Six studies were included. Five had a low risk of bias and 1 had some concerns. Three studies assessed bacterial reduction. Two were included in the meta-analysis for bacterial reduction (mean difference, 75.03 [confidence interval, CI, −271.15, 421.22], p = 0.67; I2 = 74%); and 3 in the meta-analysis for cultivable bacteria after chemomechanical preparation (odds ratio, 1.03 [CI, 0.20, 5.31], P = 0.98; I2 = 49%). Five studies assessed endotoxin reduction. Three were included in a meta-analysis (mean difference, 20.59 [CI, −36.41, 77.59], p = 0.48; I2 = 74%). There seems to be no difference in the disinfectant ability of CHX gel and NaOCl, but further research is necessary.
INTRODUCTION
MATERIALS AND METHODS
• Population (P): Adult patients subjected to root canal treatment or retreatment presenting symptomatic or asymptomatic apical periodontitis;
• Intervention (I): Root canal treatment using CHX gel as an adjunct substance during root canal preparation;
• Comparison (C): Root canal preparation using liquid NaOCl;
• Outcome (O): Primary: bacterial and/or endotoxin reduction;
Secondary: periapical healing.
• Study design (S): Only randomized clinical trials (RCTs).
RESULTS
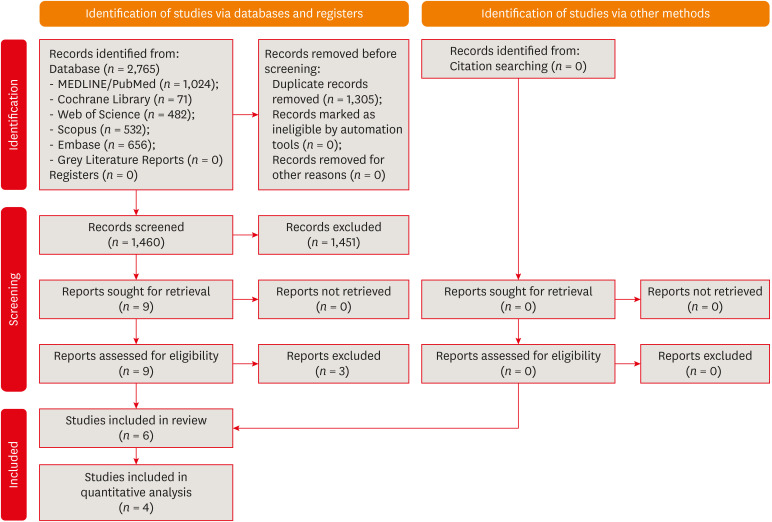
Flow diagram of the systematic search according to Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines.
Characteristics and main findings of the included studies
| Author(s) (year of publication) | Assessed outcome | Sample size (per group) | Teeth evaluated/diagnosis | Intervention | Irrigants/concentration/protocol | Method of endotoxin collection | Method of endotoxin measurement | Method of bacterial collection | Method of bacterial measurement | Moments of evaluation | Outcomes | Main findings | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Barbosa-Ribeiro et al. (2016) [49] | Bacterial and endotoxin (LTA) reduction | 20 (CHX gel – n = 10; NaOCl – n = 10) | Uniradicular teeth with a single root canal/symptomatic or asymptomatic apical periodontitis | Non-surgical retreatment | CHX gel: 2%/1 mL before each instrument and 5 mL saline solution rinse afterward with EndoVac System; NaOCl: 6%/1 mL before the use of each instrument and 5 mL rinse afterward with EndoVac System | Sterile paper point | Enzyme-linked immunosorbent assay | Sterile paper point | CFU technique | S1: Before; S2: and after chemomechanical preparation; S3: After 30 days of intracanal medication (Ca(OH)2 + 2% CHX gel) | S1: All samples presented cultivable bacteria and LTA; S2: 2% CHX gel reduced significantly more bacteria (99.3%–92.1%) and LTA (26.9%–22.6%) than 6% NaOCl; S3: Intracanal medication significantly decreased cultivable bacteria (99.5%) and LTA (38.6%), without differences between groups | Reduction of cultivable bacteria was greater than the reduction of LTA in all phases of endodontic retreatment; intracanal medication favored a greater bacterial and LTA removal | ||
| Gomes et al. (2009) [45] | Endotoxin (LPS) reduction | 54 (CHX gel – n = 27; NaOCl – n = 27) | Uniradicular teeth with a single root canal/asymptomatic apical periodontitis | Non-surgical root canal treatment | CHX gel: 2% /1 mL CHX gel + 4 mL of sterile saline solution before each instrument; NaOCl: 2.5%/5 mL following each instrument used | Sterile/apyrogenic paper point | LAL method, a modified LAL and a synthetic color-producing substrate to detect endotoxin chromogenically | - | - | S1: Before; S2: and after chemomechanical preparation | S1: Endotoxin was present in all samples; S2: Endotoxin reduction per group: 2,5% NaOCl – 57.98%; 2% CHX gel – 47.126% | Both substances were not effective in completely removing endotoxins from primarily infected root canals; NaOCl presented a significantly higher reduction when compared to CHX gel | ||
| Marinho et al. (2014) [47] | Endotoxin (LPS) reduction | 30 (CHX gel – n: 10; NaOCl – n: 10; Saline solution – n: 10) | Uniradicular teeth with a single root canal/asymptomatic apical periodontitis | Non-surgical root canal treatment | CHX gel: 2%/1 mL CHX gel + 5 mL of sterile saline solution following each instrument used; NaOCl: 2.5%/5 mL following each instrument used; Saline Solution (SS): 5 mL following each instrument used | Sterile/apyrogenic paper point | Turbidimetric kinetic limulus amoebocyte lysate (LAL) assay | - | - | S1: Before; S2: and after chemo-mechanical preparation; S3: After 3 minutes of 17% EDTA; S4: After 30 days of intracanal medication (Ca(OH)2 + saline solution) | S1: Endotoxins were present in all samples; S2: Reduction occurred in all groups without differences: 2,5% NaOCl – 99.65%; 2% CHX gel – 94.27%; SS – 96.79%; S3: 17% EDTA did not significantly decrease endotoxins; S4: Intracanal medication significantly reduced residual endotoxins compared to S3 (2,5% NaOCl – 90%; 2% CHX gel – 88.8%; SS: 85.7%), but without differences compared to S2 | No differences were found among substances used during root canal preparation; the use of intracanal medication for 30 days contributed for improvement of the endotoxin reduction | ||
| Marinho et al. (2015) [48] | Endotoxin (LPS) reduction | 30 (CHX gel – n: 10; NaOCl – n: 10; Saline solution – n: 10) | Uniradicular teeth with a single root canal/asymptomatic apical periodontitis | Non-surgical root canal treatment | CHX gel: 2% / 1 mL CHX gel + 5 mL of sterile saline solution following each instrument used; NaOCl: 2.5%/5 mL following each instrument used; Saline Solution (SS): 5 mL following each instrument used | Sterile/apyrogenic paper point | Turbidimetric kinetic LAL assay | - | - | S1: Before; S2: and after chemo-mechanical preparation; S3: After 3 minutes of 17% EDTA; S4: After 30 days of intracanal medication (Ca(OH)2 + saline solution); S5: Before root canal obturation | S1: Endotoxin was present in all samples; S2: Significant higher reduction was achieved with 2,5% NaOCl when compared to 2% CHX gel and SS; S3: 17% EDTA significantly improved endotoxin reduction in 2% CHX gel and SS groups, without differences between them; S4: Intracanal medication for 30 days significantly reduced endotoxins; S5: No differences were found between 2,5% NaOCl and 2% CHX gel groups, only when compared to SS group | The greatest endotoxin reduction occurred after chemomechanical preparation; intracanal medication enhanced endotoxin reduction | ||
| Vianna et al. (2006) [44] | Bacterial reduction | 32 (CHX gel – n = 16; NaOCl – n = 16) | Uniradicular teeth with a single root canal/asymptomatic apical periodontitis | Non-surgical root canal treatment | CHX gel: 2%/1 mL CHX gel + 4 mL of sterile saline solution after each instrument; NaOCl: 2.5%/5 mL following each instrument used | - | - | Sterile paper points | S1: Before; S2: and after chemomechanical preparation | RTQ-PCR results: | NaOCl has presented a higher capacity to kill microorganisms and to remove cells from the root canal | |||
| S1: Bacterial loads of both groups were comparable; S2: Bacterial reduction was significantly different between groups, irrespective of the detection system (SYBR Green/TaqMan): NaOCl group -99.99%/99.63%; CHX gel group - 96.62%/96.60%; | ||||||||||||||
| CFU results: | ||||||||||||||
| S1: Microorganisms were detected in all samples; S2: Mean bacterial reduction was similar in both groups: NaOCl group -99.93%; CHX gel group – 99.69% | ||||||||||||||
| Xavier et al. (2013) [46] | Endotoxin (LPS) and bacterial reduction | 48 (CHX gel – n = 12; CHX gel + calcium hydroxide dressing – n = 12; NaOCl – n = 12; NaOCl + calcium hydroxide dressing – n = 12) | Uniradicular teeth with a single root canal/asymptomatic apical periodontitis | Non-surgical root canal treatment | CHX gel: 2%/1 mL CHX gel + 4 mL of sterile saline solution before each instrument; NaOCl: 1%/5 mL following each instrument used; | Sterile/apyrogenic paper points | Kinetic chromogenic LAL assay | Sterile/apyrogenic paper points | CFU technique | 1-visit groups: | Endotoxins: | 1- and 2-visit root canal treatment protocols were effective in reducing bacteria and endotoxins, but did not completely eliminate them; 2-visit treatment was more effective in reducing endotoxins than 1-visit treatment. | ||
| S1: Before; S2: and after chemomechanical preparation | Detected in all samples; 1- and 2-visit treatment significantly reduced endotoxins: 1% NaOCl: 86.33%;/98.01%; 2% CHX gel: 84.77%/96.81%; 2-visit treatment reduced more endotoxins than 1-visit | |||||||||||||
| 2-visit groups: | Bacteria: | |||||||||||||
| S1: Before chemomechanical preparation; S2: after calcium hydroxide removal | Detected in all samples; 1- and 2-visit treatment significantly reduced bacteria, without differences: 1% NaOCl: 99.97%/99.90%; 2% CHX gel: 99.75%/96.62% | |||||||||||||
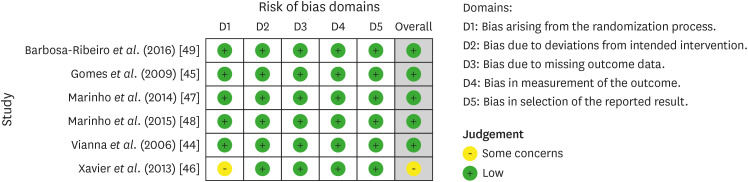
Quality assessment of the included studies according to the Cochrane Collaboration common scheme for bias and RoB 2 tool.
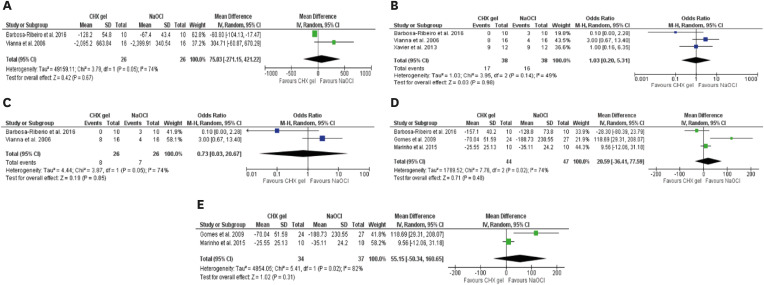
Meta-analysis results. (A) Forest plot of bacterial reduction after chemomechanical preparation with chlorhexidine gel and sodium hypochlorite; (B) Forest plot of cultivable bacteria after chemomechanical preparation with chlorhexidine gel and sodium hypochlorite; (C) Forest plot of cultivable bacteria after sensitivity analysis that excluded values from Xavier et al. [46]; (D) Forest plot of endotoxin reduction after chemomechanical preparation with chlorhexidine gel and sodium hypochlorite; (E) Forest plot of endotoxin reduction after sensitivity analysis that considered only studies that performed root canal treatments.
Assessment of quality of evidence of the included studies
DISCUSSION
CONCLUSION
-
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
-
Author Contributions:
Conceptualization: Weissheimer T, Só MVR.
Data curation: Weissheimer T, Pinto KP, da Silva EJNL, Só MVR.
Formal analysis: Weissheimer T, Pinto KP.
Investigation: Weissheimer T, Pinto KP.
Methodology: Weissheimer T, Pinto KP.
Project administration: da Rosa RA, Só MVR.
Supervision: Só MVR.
Writing - original draft: Weissheimer T.
Writing - review & editing: Hashizume LN.
SUPPLEMENTARY MATERIAL
- 1. Siqueira JF Jr, Rôças IN. Clinical implications and microbiology of bacterial persistence after treatment procedures. J Endod 2008;34:1291-1301.e3.ArticlePubMed
- 2. Machado FP, Khoury RD, Toia CC, Flores Orozco EI, de Oliveira FE, de Oliveira LD, et al. Primary versus post-treatment apical periodontitis: microbial composition, lipopolysaccharides and lipoteichoic acid levels, signs and symptoms. Clin Oral Investig 2020;24:3169-3179.ArticlePubMedPDF
- 3. Mazzi-Chaves JF, Silva-Sousa YTC, Leoni GB, Silva-Sousa AC, Estrela L, Estrela C, et al. Micro-computed tomographic assessment of the variability and morphological features of root canal system and their ramifications. J Appl Oral Sci 2020;28:e20190393.ArticlePubMedPMC
- 4. Almeida BM, Provenzano JC, Marceliano-Alves MF, Rôças IN, Siqueira JF Jr. Matching the dimensions of currently available instruments with the apical diameters of mandibular molar mesial root canals obtained by micro–computed tomography. J Endod 2019;45:756-760.ArticlePubMed
- 5. Siqueira Junior JF, Rôças IDN, Marceliano-Alves MF, Pérez AR, Ricucci D. Unprepared root canal surface areas: causes, clinical implications, and therapeutic strategies. Braz Oral Res 2018;32:e65.PubMed
- 6. Siqueira JF Jr, Pérez AR, Marceliano-Alves MF, Provenzano JC, Silva SG, Pires FR, et al. What happens to unprepared root canal walls: a correlative analysis using micro-computed tomography and histology/scanning electron microscopy. Int Endod J 2018;51:501-508.ArticlePubMedPDF
- 7. Del Carpio-Perochena AE, Bramante CM, Duarte MAH, Cavenago BC, Villas-Boas MH, Graeff MS, et al. Biofilm dissolution and cleaning ability of different irrigant solutions on intraorally infected dentin. J Endod 2011;37:1134-1138.ArticlePubMed
- 8. Ordinola-Zapata R, Bramante CM, Cavenago B, Graeff MSZ, Gomes de Moraes I, Marciano M, et al. Antimicrobial effect of endodontic solutions used as final irrigants on a dentine biofilm model. Int Endod J 2012;45:162-168.ArticlePubMed
- 9. Ordinola-Zapata R, Bramante CM, Garcia RB, de Andrade FB, Bernardineli N, de Moraes IG, et al. The antimicrobial effect of new and conventional endodontic irrigants on intra-orally infected dentin. Acta Odontol Scand 2013;71:424-431.ArticlePubMed
- 10. Estrela C, Estrela CRA, Barbin EL, Spanó JCE, Marchesan MA, Pécora JD. Mechanism of action of sodium hypochlorite. Braz Dent J 2002;13:113-117.ArticlePubMed
- 11. Petridis X, Busanello FH, So MVR, Dijkstra RJB, Sharma PK, van der Sluis LWM. Factors affecting the chemical efficacy of 2% sodium hypochlorite against oral steady-state dual-species biofilms: exposure time and volume application. Int Endod J 2019;52:1182-1195.ArticlePubMedPMCPDF
- 12. Petridis X, Busanello FH, So MVR, Dijkstra RJB, Sharma PK, van der Sluis LWM. Chemical efficacy of several NaOCl concentrations on biofilms of different architecture: new insights on NaOCl working mechanisms. Int Endod J 2019;52:1773-1788.ArticlePubMedPMCPDF
- 13. Zehnder M. Root canal irrigants. J Endod 2006;32:389-398.ArticlePubMed
- 14. Busanello FH, Petridis X, So MVR, Dijkstra RJB, Sharma PK, van der Sluis LWM. Chemical biofilm removal capacity of endodontic irrigants as a function of biofilm structure: optical coherence tomography, confocal microscopy and viscoelasticity determination as integrated assessment tools. Int Endod J 2019;52:461-474.ArticlePubMedPDF
- 15. Mohammadi Z, Abbott PV. The properties and applications of chlorhexidine in endodontics. Int Endod J 2009;42:288-302.ArticlePubMed
- 16. Gomes BPFA, Vianna ME, Zaia AA, Almeida JFA, Souza-Filho FJ, Ferraz CCR. Chlorhexidine in endodontics. Braz Dent J 2013;24:89-102.ArticlePubMed
- 17. Boutsioukis C, Arias-Moliz MT, Chávez de Paz LE. A critical analysis of research methods and experimental models to study irrigants and irrigation systems. Int Endod J 2022;55(Supplement 2):295-329.ArticlePubMedPMCPDF
- 18. Basrani B, Lemonie C. Chlorhexidine gluconate. Aust Endod J 2005;31:48-52.ArticlePubMed
- 19. Prado M, Silva EJNL, Duque TM, Zaia AA, Ferraz CCR, Almeida JFA, et al. Antimicrobial and cytotoxic effects of phosphoric acid solution compared to other root canal irrigants. J Appl Oral Sci 2015;23:158-163.ArticlePubMedPMC
- 20. Khanifam P, Pullisaar H, Risheim H. Local facial atrophy and permanent anesthesia of right upper lip following subcutaneous extrusion of chlorhexidine digluconate. Oral and Maxillofacial Surgery Cases 2019;5:100087.Article
- 21. Okino LA, Siqueira EL, Santos M, Bombana AC, Figueiredo JAP. Dissolution of pulp tissue by aqueous solution of chlorhexidine digluconate and chlorhexidine digluconate gel. Int Endod J 2004;37:38-41.ArticlePubMed
- 22. Siqueira JF Jr, Rôças IN, Paiva SSM, Guimarães-Pinto T, Magalhães KM, Lima KC. Bacteriologic investigation of the effects of sodium hypochlorite and chlorhexidine during the endodontic treatment of teeth with apical periodontitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;104:122-130.ArticlePubMed
- 23. Sousa ELR, Martinho FC, Nascimento GG, Leite FRM, Gomes BPFA. Quantification of endotoxins in infected root canals and acute apical abscess exudates: monitoring the effectiveness of root canal procedures in the reduction of endotoxins. J Endod 2014;40:177-181.ArticlePubMed
- 24. Freire LG, Carvalho CN, Ferrari PHP, Siqueira EL, Gavini G. Influence of dentin on pH of 2% chlorhexidine gel and calcium hydroxide alone or in combination. Dent Traumatol 2010;26:276-280.ArticlePubMed
- 25. Signoretti FGC, Gomes BPFA, Montagner F, Barrichello Tosello F, Jacinto RC. Influence of 2% chlorhexidine gel on calcium hydroxide ionic dissociation and its ability of reducing endotoxin. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2011;111:653-658.ArticlePubMed
- 26. Ordinola-Zapata R, Bramante CM, Minotti PG, Cavenago BC, Garcia RB, Bernardineli N, et al. Antimicrobial activity of triantibiotic paste, 2% chlorhexidine gel, and calcium hydroxide on an intraoral-infected dentin biofilm model. J Endod 2013;39:115-118.ArticlePubMed
- 27. Fiorillo L. Chlorhexidine gel use in the oral district: a systematic review. Gels 2019;5:1-16.ArticlePubMedPMC
- 28. Sena NT, Gomes BPFA, Vianna ME, Berber VB, Zaia AA, Ferraz CC, et al. In vitro antimicrobial activity of sodium hypochlorite and chlorhexidine against selected single-species biofilms. Int Endod J 2006;39:878-885.PubMed
- 29. Gomes BP, Ferraz CC, Vianna ME, Berber VB, Teixeira FB, Souza-Filho FJ. In vitro antimicrobial activity of several concentrations of sodium hypochlorite and chlorhexidine gluconate in the elimination of Enterococcus faecalis. Int Endod J 2001;34:424-428.PubMed
- 30. Gonçalves LS, Rodrigues RCV, Andrade Junior CV, Soares RG, Vettore MV. The effect of sodium hypochlorite and chlorhexidine as irrigant solutions for root canal disinfection: a systematic review of clinical trials. J Endod 2016;42:527-532.ArticlePubMed
- 31. Neelakantan P, Herrera DR, Pecorari VGA, Gomes BPFA. Endotoxin levels after chemomechanical preparation of root canals with sodium hypochlorite or chlorhexidine: a systematic review of clinical trials and meta-analysis. Int Endod J 2019;52:19-27.ArticlePubMedPDF
- 32. Ruksakiet K, Hanák L, Farkas N, Hegyi P, Sadaeng W, Czumbel LM, et al. Antimicrobial efficacy of chlorhexidine and sodium hypochlorite in root canal disinfection: a systematic review and meta-analysis of randomized controlled trials. J Endod 2020;46:1032-1041.e7.ArticlePubMed
- 33. Fedorowicz Z, Nasser M, Sequeira-Byron P, de Souza RF, Carter B, Heft M. Irrigants for non-surgical root canal treatment in mature permanent teeth. Cochrane Database Syst Rev 2012;(9):CD008948.ArticlePubMedPMC
- 34. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann T, Mulrow CD, et al. Mapping of reporting guidance for systematic reviews and meta-analyses generated a comprehensive item bank for future reporting guidelines. J Clin Epidemiol 2020;118:60-68.ArticlePubMed
- 35. Maia LC, Antonio AG. Systematic reviews in dental research. A guideline. J Clin Pediatr Dent 2012;37:117-124.ArticlePubMedPDF
- 36. Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015;4:1.PubMedPMC
- 37. Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898.ArticlePubMed
- 38. Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Pge MJ, et al. Cochrane handbook for systematic reviews of interventions version 6.2. updated February, 2022]. February 20, 2023]. Available from: www.training.cochrane.org/handbook.
- 39. Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-560.ArticlePubMedPMC
- 40. Page MJ, Higgins JPT, Sterne JAC. Assessing risk of bias due to missing results in a synthesis. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane handbook for systematic reviews of interventions version 6.2. UK, Chichester: John Wiley & Sons; 2021.
- 41. Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 2011;64:383-394.ArticlePubMed
- 42. Provenzano JC, Rôças IN, Tavares LFD, Neves BC, Siqueira JF Jr. Short-chain fatty acids in infected root canals of teeth with apical periodontitis before and after treatment. J Endod 2015;41:831-835.ArticlePubMed
- 43. Barbosa-Ribeiro M, Arruda-Vasconcelos R, de-Jesus-Soares A, Zaia AA, Ferraz CCR, de Almeida JF, et al. Effectiveness of calcium hydroxide-based intracanal medication on infectious/inflammatory contents in teeth with post-treatment apical periodontitis. Clin Oral Investig 2019;23:2759-2766.ArticlePubMedPDF
- 44. Vianna ME, Horz HP, Gomes BPFA, Conrads G. In vivo evaluation of microbial reduction after chemo-mechanical preparation of human root canals containing necrotic pulp tissue. Int Endod J 2006;39:484-492.PubMed
- 45. Gomes BPFA, Martinho FC, Vianna ME. Comparison of 2.5% sodium hypochlorite and 2% chlorhexidine gel on oral bacterial lipopolysaccharide reduction from primarily infected root canals. J Endod 2009;35:1350-1353.ArticlePubMed
- 46. Xavier ACC, Martinho FC, Chung A, Oliveira LD, Jorge AOC, Valera MC, et al. One-visit versus two-visit root canal treatment: effectiveness in the removal of endotoxins and cultivable bacteria. J Endod 2013;39:959-964.ArticlePubMed
- 47. Marinho ACS, Martinho FC, Zaia AA, Ferraz CC, Gomes BPFA. Monitoring the effectiveness of root canal procedures on endotoxin levels found in teeth with chronic apical periodontitis. J Appl Oral Sci 2014;22:490-495.ArticlePubMedPMC
- 48. Marinho ACS, Martinho FC, Leite FRM, Nascimento GG, Gomes BPFA. Proinflammatory activity of primarily infected endodontic content against macrophages after different phases of the root canal therapy. J Endod 2015;41:817-823.ArticlePubMed
- 49. Barbosa-Ribeiro M, De-Jesus-Soares A, Zaia AA, Ferraz CCR, Almeida JFA, Gomes BPFA. Quantification of lipoteichoic acid contents and cultivable bacteria at the different phases of the endodontic retreatment. J Endod 2016;42:552-556.ArticlePubMed
- 50. McGuinness LA, Higgins JPT. Risk-of-bias VISualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods 2021;12:55-61.ArticlePubMedPDF
- 51. Buck RA, Cai J, Eleazer PD, Staat RH, Hurst HE. Detoxification of endotoxin by endodontic irrigants and calcium hydroxide. J Endod 2001;27:325-327.ArticlePubMed
- 52. Tanomaru JMG, Leonardo MR, Tanomaru Filho M, Bonetti Filho I, Silva LAB. Effect of different irrigation solutions and calcium hydroxide on bacterial LPS. Int Endod J 2003;36:733-739.ArticlePubMedPDF
- 53. Silva LAB, Leonardo MR, Assed S, Tanomaru Filho M. Histological study of the effect of some irrigating solutions on bacterial endotoxin in dogs. Braz Dent J 2004;15:109-114.ArticlePubMed
- 54. de Oliveira LD, Jorge AOC, Carvalho CAT, Koga-Ito CY, Valera MC. In vitro effects of endodontic irrigants on endotoxins in root canals. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;104:135-142.PubMed
- 55. Marinho ACS, To TT, Darveau RP, Gomes BPFA. Detection and function of lipopolysaccharide and its purified lipid A after treatment with auxiliary chemical substances and calcium hydroxide dressings used in root canal treatment. Int Endod J 2018;51:1118-1129.ArticlePubMedPDF
- 56. Akobeng AK. Understanding type I and type II errors, statistical power and sample size. Acta Paediatr 2016;105:605-609.PubMed
- 57. Tronstad L, Sunde PT. The evolving new understanding of endodontic infections. Endod Topics 2003;6:57-77.Article
- 58. Neelakantan P, Romero M, Vera J, Daood U, Khan AU, Yan A, et al. Biofilms in endodontics—current status and future directions. Int J Mol Sci 2017;18:1748-1769.ArticlePubMedPMC
- 59. Arias-Moliz MT, Ordinola-Zapata R, Baca P, Ruiz-Linares M, García García E, Hungaro Duarte MA, et al. Antimicrobial activity of chlorhexidine, peracetic acid and sodium hypochlorite/etidronate irrigant solutions against Enterococcus faecalis biofilms. Int Endod J 2015;48:1188-1193.ArticlePubMed
- 60. Byström A, Sundqvist G. Bacteriologic evaluation of the efficacy of mechanical root canal instrumentation in endodontic therapy. Scand J Dent Res 1981;89:321-328.ArticlePubMed
- 61. Gazzaneo I, Vieira GCS, Pérez AR, Alves FRF, Gonçalves LS, Mdala I, et al. Root canal disinfection by single- and multiple-instrument systems: Effects of sodium hypochlorite volume, concentration, and retention time. J Endod 2019;45:736-741.ArticlePubMed
- 62. Guyatt GH, Oxman AD, Vist G, Kunz R, Brozek J, Alonso-Coello P, et al. GRADE guidelines: 4. Rating the quality of evidence--study limitations (risk of bias). J Clin Epidemiol 2011;64:407-415.ArticlePubMed
- 63. Guyatt GH, Oxman AD, Kunz R, Brozek J, Alonso-Coello P, Rind D, et al. GRADE guidelines 6. Rating the quality of evidence--imprecision. J Clin Epidemiol 2011;64:1283-1293.ArticlePubMed
- 64. Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, et al. GRADE guidelines: 7. Rating the quality of evidence--inconsistency. J Clin Epidemiol 2011;64:1294-1302.ArticlePubMed
- 65. Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, et al. GRADE guidelines: 8. Rating the quality of evidence--indirectness. J Clin Epidemiol 2011;64:1303-1310.ArticlePubMed
- 66. Guyatt GH, Oxman AD, Sultan S, Glasziou P, Akl EA, Alonso-Coello P, et al. GRADE guidelines: 9. Rating up the quality of evidence. J Clin Epidemiol 2011;64:1311-1316.ArticlePubMed
REFERENCES
Tables & Figures
REFERENCES
Citations

- Bactericidal Effects of Ultraviolet-C Light-Emitting Diode Prototype Device Through Thin Optical Fiber
Mi-Jeong Jeon, Yu-Sung Choi, Deog-Gyu Seo
Applied Sciences.2025; 15(8): 4504. CrossRef - Effectiveness of Irrigation Protocols in Endodontic Therapy: An Umbrella Review
Manuel J. Orozco-Gallego, Eliana L. Pineda-Vélez, Wilder J. Rojas-Gutiérrez, Martha L. Rincón-Rodríguez, Andrés A. Agudelo-Suárez
Dentistry Journal.2025; 13(6): 273. CrossRef - In Vitro Evaluation of Disinfectants on Gutta-Percha Cones: Antimicrobial Efficacy Against Enterococcus faecalis and Candida albicans
Tringa Kelmendi, Donika Bajrami Shabani, Aida Meto, Hani Ounsi
Journal of Clinical Medicine.2025; 14(19): 6846. CrossRef - Preparing porcine lens to mimic human lens capsule
Yajing Pei, Shaofeng Han, Mingfeng Lu, Yang Yang, Ke Ma
Journal of Cataract & Refractive Surgery.2024; 50(9): 963. CrossRef - Comparative Evaluation of Disinfection Protocols for Dental Impressions in Prosthodontics
Subhash Sonkesriya, Ghanshyam Gaur, Akanksha Maheshwari, Arun Kumar Ashahiya, Simran Kaur Aulakh, Amit Kumar, Bhumika Kamal Badiyani
Cureus.2024;[Epub] CrossRef
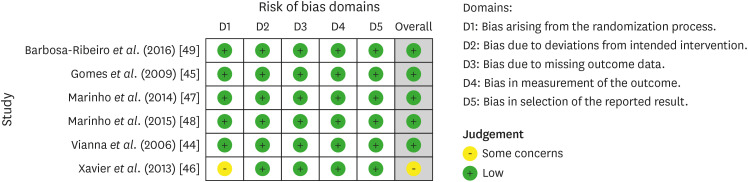
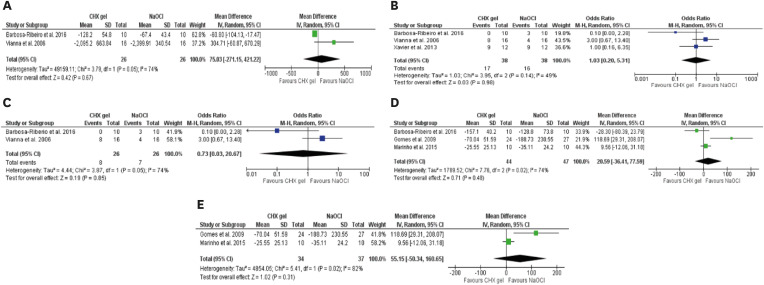
Figure 1
Figure 2
Figure 3
Characteristics and main findings of the included studies
| Author(s) (year of publication) | Assessed outcome | Sample size (per group) | Teeth evaluated/diagnosis | Intervention | Irrigants/concentration/protocol | Method of endotoxin collection | Method of endotoxin measurement | Method of bacterial collection | Method of bacterial measurement | Moments of evaluation | Outcomes | Main findings | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Barbosa-Ribeiro | Bacterial and endotoxin (LTA) reduction | 20 (CHX gel – | Uniradicular teeth with a single root canal/symptomatic or asymptomatic apical periodontitis | Non-surgical retreatment | CHX gel: 2%/1 mL before each instrument and 5 mL saline solution rinse afterward with EndoVac System; NaOCl: 6%/1 mL before the use of each instrument and 5 mL rinse afterward with EndoVac System | Sterile paper point | Enzyme-linked immunosorbent assay | Sterile paper point | CFU technique | S1: Before; S2: and after chemomechanical preparation; S3: After 30 days of intracanal medication (Ca(OH)2 + 2% CHX gel) | S1: All samples presented cultivable bacteria and LTA; S2: 2% CHX gel reduced significantly more bacteria (99.3%–92.1%) and LTA (26.9%–22.6%) than 6% NaOCl; S3: Intracanal medication significantly decreased cultivable bacteria (99.5%) and LTA (38.6%), without differences between groups | Reduction of cultivable bacteria was greater than the reduction of LTA in all phases of endodontic retreatment; intracanal medication favored a greater bacterial and LTA removal | ||
| Gomes | Endotoxin (LPS) reduction | 54 (CHX gel – | Uniradicular teeth with a single root canal/asymptomatic apical periodontitis | Non-surgical root canal treatment | CHX gel: 2% /1 mL CHX gel + 4 mL of sterile saline solution before each instrument; NaOCl: 2.5%/5 mL following each instrument used | Sterile/apyrogenic paper point | LAL method, a modified LAL and a synthetic color-producing substrate to detect endotoxin chromogenically | - | - | S1: Before; S2: and after chemomechanical preparation | S1: Endotoxin was present in all samples; S2: Endotoxin reduction per group: 2,5% NaOCl – 57.98%; 2% CHX gel – 47.126% | Both substances were not effective in completely removing endotoxins from primarily infected root canals; NaOCl presented a significantly higher reduction when compared to CHX gel | ||
| Marinho | Endotoxin (LPS) reduction | 30 (CHX gel – n: 10; NaOCl – n: 10; Saline solution – n: 10) | Uniradicular teeth with a single root canal/asymptomatic apical periodontitis | Non-surgical root canal treatment | CHX gel: 2%/1 mL CHX gel + 5 mL of sterile saline solution following each instrument used; NaOCl: 2.5%/5 mL following each instrument used; Saline Solution (SS): 5 mL following each instrument used | Sterile/apyrogenic paper point | Turbidimetric kinetic limulus amoebocyte lysate (LAL) assay | - | - | S1: Before; S2: and after chemo-mechanical preparation; S3: After 3 minutes of 17% EDTA; S4: After 30 days of intracanal medication (Ca(OH)2 + saline solution) | S1: Endotoxins were present in all samples; S2: Reduction occurred in all groups without differences: 2,5% NaOCl – 99.65%; 2% CHX gel – 94.27%; SS – 96.79%; S3: 17% EDTA did not significantly decrease endotoxins; S4: Intracanal medication significantly reduced residual endotoxins compared to S3 (2,5% NaOCl – 90%; 2% CHX gel – 88.8%; SS: 85.7%), but without differences compared to S2 | No differences were found among substances used during root canal preparation; the use of intracanal medication for 30 days contributed for improvement of the endotoxin reduction | ||
| Marinho | Endotoxin (LPS) reduction | 30 (CHX gel – n: 10; NaOCl – n: 10; Saline solution – n: 10) | Uniradicular teeth with a single root canal/asymptomatic apical periodontitis | Non-surgical root canal treatment | CHX gel: 2% / 1 mL CHX gel + 5 mL of sterile saline solution following each instrument used; NaOCl: 2.5%/5 mL following each instrument used; Saline Solution (SS): 5 mL following each instrument used | Sterile/apyrogenic paper point | Turbidimetric kinetic LAL assay | - | - | S1: Before; S2: and after chemo-mechanical preparation; S3: After 3 minutes of 17% EDTA; S4: After 30 days of intracanal medication (Ca(OH)2 + saline solution); S5: Before root canal obturation | S1: Endotoxin was present in all samples; S2: Significant higher reduction was achieved with 2,5% NaOCl when compared to 2% CHX gel and SS; S3: 17% EDTA significantly improved endotoxin reduction in 2% CHX gel and SS groups, without differences between them; S4: Intracanal medication for 30 days significantly reduced endotoxins; S5: No differences were found between 2,5% NaOCl and 2% CHX gel groups, only when compared to SS group | The greatest endotoxin reduction occurred after chemomechanical preparation; intracanal medication enhanced endotoxin reduction | ||
| Vianna | Bacterial reduction | 32 (CHX gel – | Uniradicular teeth with a single root canal/asymptomatic apical periodontitis | Non-surgical root canal treatment | CHX gel: 2%/1 mL CHX gel + 4 mL of sterile saline solution after each instrument; NaOCl: 2.5%/5 mL following each instrument used | - | - | Sterile paper points | S1: Before; S2: and after chemomechanical preparation | RTQ-PCR results: | NaOCl has presented a higher capacity to kill microorganisms and to remove cells from the root canal | |||
| S1: Bacterial loads of both groups were comparable; S2: Bacterial reduction was significantly different between groups, irrespective of the detection system (SYBR Green/TaqMan): NaOCl group -99.99%/99.63%; CHX gel group - 96.62%/96.60%; | ||||||||||||||
| CFU results: | ||||||||||||||
| S1: Microorganisms were detected in all samples; S2: Mean bacterial reduction was similar in both groups: NaOCl group -99.93%; CHX gel group – 99.69% | ||||||||||||||
| Xavier | Endotoxin (LPS) and bacterial reduction | 48 (CHX gel – | Uniradicular teeth with a single root canal/asymptomatic apical periodontitis | Non-surgical root canal treatment | CHX gel: 2%/1 mL CHX gel + 4 mL of sterile saline solution before each instrument; NaOCl: 1%/5 mL following each instrument used; | Sterile/apyrogenic paper points | Kinetic chromogenic LAL assay | Sterile/apyrogenic paper points | CFU technique | 1-visit groups: | Endotoxins: | 1- and 2-visit root canal treatment protocols were effective in reducing bacteria and endotoxins, but did not completely eliminate them; 2-visit treatment was more effective in reducing endotoxins than 1-visit treatment. | ||
| S1: Before; S2: and after chemomechanical preparation | Detected in all samples; 1- and 2-visit treatment significantly reduced endotoxins: 1% NaOCl: 86.33%;/98.01%; 2% CHX gel: 84.77%/96.81%; 2-visit treatment reduced more endotoxins than 1-visit | |||||||||||||
| 2-visit groups: | Bacteria: | |||||||||||||
| S1: Before chemomechanical preparation; S2: after calcium hydroxide removal | Detected in all samples; 1- and 2-visit treatment significantly reduced bacteria, without differences: 1% NaOCl: 99.97%/99.90%; 2% CHX gel: 99.75%/96.62% | |||||||||||||
LTA, lipoteichoic acid; CHX, chlorhexidine; NaOCl, sodium hypochlorite; LPS, lipopolysaccharide; CFU, colony forming unit; LAL, limulus amoebocyte lysate; EDTA, ethylenediaminetetraacetic acid; RTQ-PCR, real-time quantitative-polymerase chain reaction.
Assessment of quality of evidence of the included studies
| No. of studies (study design) | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | Overall certainty of evidence |
|---|---|---|---|---|---|---|
| 6 randomized trials | Not serious | Serious* | Not serious | Very serious† | None | ⨁◯◯◯ |
| VERY LOW |
*Substantial heterogeneity was observed among studies; †Optimal information size was not met (pooled sample size of 300) and confidence intervals were under 0.75 or above 1.25.
LTA, lipoteichoic acid; CHX, chlorhexidine; NaOCl, sodium hypochlorite; LPS, lipopolysaccharide; CFU, colony forming unit; LAL, limulus amoebocyte lysate; EDTA, ethylenediaminetetraacetic acid; RTQ-PCR, real-time quantitative-polymerase chain reaction.
*Substantial heterogeneity was observed among studies; †Optimal information size was not met (pooled sample size of 300) and confidence intervals were under 0.75 or above 1.25.

 KACD
KACD
 ePub Link
ePub Link Cite
Cite

