Abstract
-
Objectives
This study evaluated the effects of Biodentine (BD), Bio-C Repair (BCR), and mineral trioxide aggregate (MTA) plug on the fracture resistance of simulated immature teeth with replacement root resorption (RRR) and in vitro-induced osteoclastogenesis.
-
Materials and Methods
Sixty bovine incisors simulating immature teeth and RRR were divided into 5 groups: BD and BCR groups, with samples completely filled with the respective materials; MTA group, which utilized a 3-mm apical MTA plug; RRR group, which received no root canal filling; and normal periodontal ligament (PL) group, which had no RRR and no root canal filling. All the teeth underwent cycling loading, and compression strength testing was performed using a universal testing machine. RAW 264.7 macrophages were treated with 1:16 extracts of BD, BCR, and MTA containing receptor activator of nuclear factor-kappa B ligand (RANKL) for 5 days. RANKL-induced osteoclast differentiation was assessed by staining with tartrate-resistant acid phosphatase. The fracture load and osteoclast number were analyzed using 1-way ANOVA and Tukey’s test (α = 0.05).
-
Results
No significant difference in fracture resistance was observed among the groups (p > 0.05). All materials similarly inhibited osteoclastogenesis (p > 0.05), except for BCR, which led to a lower percentage of osteoclasts than did MTA (p < 0.0001).
-
Conclusions
The treatment options for non-vital immature teeth with RRR did not strengthen the teeth and promoted a similar resistance to fractures in all cases. BD, MTA, and BCR showed inhibitory effects on osteoclast differentiation, with BCR yielding improved results compared to the other materials.
-
Keywords: Fracture strength; Non-vital tooth; Osteoclastogenesis; Root resorption; Silicate cement
INTRODUCTION
Trauma to immature permanent teeth can lead to pulp necrosis, thereby interrupting root development and making root canal treatment challenging. Although pulp necrosis is the most common post-traumatic complication, replacement root resorption (RRR) is the most concerning complication as it may affect the long-term survival of teeth, mainly after lateral luxation and avulsion [
1,
2].
In patients with RRR, new alveolar bone is formed and deposited in the space previously occupied by the periodontal ligament (PL) fibers that were lost, and the root is progressively resorbed and replaced by bone tissue [
3]. Thus, the development of the RRR process invariably leads to the exposure of the filling material to periodontal tissues. Therefore, choosing root canal filling materials with greater biocompatibility is crucial [
4]. Additionally, as resorption is mediated by osteoclasts/odontoclasts, filling the root canal with materials that reduce or inhibit osteoclastic activity could delay the progression of root resorption. This enables dentists to plan adequate rehabilitation for hebiatric patients, in whom the early loss of teeth has a greater psychosocial impact.
Mineral trioxide aggregate (MTA) has been suggested for filling reimplanted teeth due to its sealing ability, biocompatibility, low solubility, ability to inhibit osteoclastogenesis, adequate radiopacity, and high pH [
4]. However, MTA has several disadvantages, including prolonged setting time, potential for coronal staining, and handling difficulties [
5]. Thus, other calcium-silicate based materials (CSM) materials have been suggested as alternatives.
Biodentine (BD; Septodont, Saint Maur-des-Fossés, France) is a tricalcium silicate-based restorative cement indicated as a “dentine replacement” material. This material is comparable to MTA in terms of its biocompatibility and induction of a calcific barrier [
6]. In addition, it has advantages in terms of several other properties, including improved mixing, handling, shorter initial setting time, and less coronal discoloration after its use [
6]. Recently, a new ready-to-use CSM, Bio-C Repair (BCR; Angelus, Londrina, Brazil), has become available for reparative or regenerative endodontic treatments. This material has low cytotoxicity, appropriate biocompatibility, and biomineralization ability [
7,
8,
9,
10].
Although previous studies have evaluated the fracture resistance of immature teeth restored with various intra-radicular filling materials, to our knowledge, no study has evaluated the intra-radicular filling materials in immature permanent teeth in conditions that mimic RRR [
11,
12]. Thus, in this study, we aimed to evaluate the fracture resistance after cyclic loading of simulated immature teeth with RRR filled with BD, BCR, or MTA plugs. Additionally, we evaluated the cytotoxicity and anti-osteoclastic effects of these materials. The null hypothesis tested was: 1) treatment with different intra-radicular filling materials would not affect the fracture resistance of immature permanent teeth with RRR, 2) the tested materials would not affect RAW264.7 macrophage viability, and osteoclast-like maturation.
MATERIALS AND METHODS
This manuscript has been written according to the Preferred Reporting Items for Laboratory Studies in Endodontology (PRILE) 2021 guidelines [
13] (
Supplementary Figure 1).
The three materials used in this study were: BCR, which was ready-to-use (Angelus); BD, which was prepared by adding 5 drops of liquid to the capsule and shaking it for 30 seconds at 4,000 rpm (Septdont); and MTA, which was prepared by mixing the contents of one sachet with one drop of distilled water (Angelus) for 30 seconds. Based on the manufacturers’ instructions, the components of the CSM tested are described in
Table 1.
Table 1Calcium-silicate based materials, chemical compositions, and manufacturers of the materials employed in this study
|
Materials |
Chemical composition |
Manufacturer |
Technical information |
|
Biodentine |
Powder: Tricalcium silicate, zirconium oxide, calcium oxide, calcium carbonate, yellow pigment, red pigment, and brown iron oxide |
Septodont |
Five drops of liquid are placed in the capsule and it is shaken at 4,000 rpm for 30 sec |
|
Liquid: Calcium chloride dihydrate, sand, and purified water |
|
White MTA |
Powder: Silicon dioxide, potassium oxide, aluminum trioxide, sodium oxide, iron trioxide, sulfur oxide, calcium oxide, bismuth oxide, magnesium oxide |
Angelus |
One sachet of powder mixed with one drop of distilled water for 30 sec |
|
Liquid: Water and plasticizer |
|
Bio-C Repair |
Calcium silicate, calcium aluminate, calcium oxide, zirconium oxide, iron oxide, silicon dioxide and dispersing agent |
Angelus |
Product ready for use, mixture not being necessary |
Fracture resistance
Sample size calculation
The sample size was based on the data from Tanalp
et al. [
14] and was calculated using the G*Power version 3.1.9.6 software (
http://www.psycho.uni-duesseldorf.de/abteilungen/aap/gpower3/) to allow for analysis with α = 0.05, power (1−ß prob) = 0.99, and effect size f = 1.52. The analysis of covariance (fixed and main effects, and interactions) statistical test was performed on the data. The type of power analysis was set a priori to compute the required sample size given the α, power, and effect size. Therefore, a minimum of 12 teeth were allocated to each experimental group, with a total of 60 teeth.
Selection of samples
Bovine central incisors (30–36 months) were obtained from a local abattoir (Real, Uberlândia, MG, Brazil), cleaned, and stored in distilled water at 4°C. Using a microscope (D. F. Vasconcellos, Valença, RJ, Brazil) at 3.0 × magnification, the teeth were analyzed for the presence of cracks and fractures. Teeth without cracks, fracture lines, or other deformities underwent measurements of the mesiodistal and buccolingual dimensions of the roots using a digital caliper (Mitutoyo Sul Americana Ltda., Suzano, SP, Brazil). Samples with a maximum deviation of 10% from the mean were included in the study. The selected teeth were stored in distilled water at 4°C until further use.
Simulation of immature permanent teeth
To simulate complicated crown fractures in immature teeth, the samples were sectioned 8 mm above and 12 mm below the cemento-enamel junction (CEJ) while under a water-cooled diamond disc [
8]. The root canals were instrumented with Peeso reamers (size 1–5, Dentsply Maillefer) followed by a 3017 HL diamond bur (KG Sorensen, Barueri, SP, Brazil) to create a standard open apex with a diameter of approximately 2.5 mm [
15]. Next, the root canals were rinsed with 20 mL of 2.5% sodium hypochlorite followed by final irrigation with 3 mL of 17% ethylenediaminetetraacetic acid (EDTA) solution and 5 mL of distilled water [
8]. The samples were re-evaluated for the presence of cracks or defects using the transillumination method. All teeth with cracks were excluded from this study.
Root canal filling and simulation of RRR
The RRR simulation was performed on the palatal surface of the prepared samples based on the protocol previously described by Vieira
et al. [
16]. First, perforations were made perpendicular to the palatal surface in the cervical, middle, and apical thirds of the root using cylindrical drills with diameters of 1.2 mm (1093; KG Sorensen), 1.8 mm (2094; KG Sorensen), and 0.6 mm (1090; KG Sorensen), respectively. The distance between each perforation was approximately 4 mm. Subsequently, the root regions containing the perforations were exposed to an acid demineralization process through treatment with a 5% nitric acid solution for 12 hours, 8% sodium hypochlorite solution for 10 minutes, and 5% nitric acid solution for 12 hours for resorption lesions. The teeth were washed and stored in deionized water to arrest the process. Randomization (blocked random scheme) was performed using the website (
www.sealedenvelope.com). Randomization and allocation of the samples to one of the following five groups (
n = 12) were performed by the same researcher (CCGM), who was not involved in the implementation (GANF) and evaluation (GLS) processes.
• RRR (negative control group): RRR simulated; no apical plug or root canal filling was performed.
• Normal PL (positive control group): no RRR, apical plug, or root canal filling was performed.
• MTA Plug: RRR simulated; MTA was prepared according to the manufacturer’s instructions, placed into the root canals with an MTA carrier, and condensed with hand pluggers to create a 4-mm-thick MTA. After MTA apexification, the root canal was filled with a Bio-C sealer (Angelus) and gutta-percha cones (Dentsply-Malleifer).
• BCR: RRR was simulated, and the root canals were filled with BCR. The ready-to-use cement was inserted incrementally and condensed in the root canal with hand pluggers up to the CEJ.
• BD: RRR-simulated BD was prepared according to the manufacturer’s instructions and inserted into the root canal as described for the previous group, up to the CEJ.
Following the procedures described above, the teeth were radiographed again to confirm the quality of the fillings, and endodontic access was restored using an adhesive system (Adper Single Bond 2; 3M ESPE, St. Paul, MN, USA) and composite resin (Filtek Z350 XT; 3M, Sumaré, SP, Brazil). The samples were stored at 37°C and 100% humidity for 24 hours. After this period, the teeth were inserted into resin cylinders to simulate RRR regions and regions with normal PLs. The external surfaces of the root were then covered with a 0.2–0.3 mm thick wax layer until it reached 2 mm below the CEJ. Subsequently, the wax-covered roots were embedded in polystyrene resin cylinders (Classico, Rio de Janeiro, RJ, Brazil). After resin polymerization, the roots were removed from the cylinder, and all the wax was removed from the root surface, creating a space in the resin cylinder. Next, the polyether impression material Impregum F (3M ESPE) was mixed and distributed over the buccal root surface. Simultaneously, the polystyrene resin was manipulated and distributed over the palatal root surface, filling the regions where the perforations were made and the regions that were perforation-free. According to the procedure by Soares
et al. [
17], the entire roots of the teeth without RRR and with only simulated PLs were soaked in Impregum F (3M). The teeth were then re-inserted into the cylinder, and excess material was removed using a scalpel blade.
Mechanical cycling test and fracture testing
Chewing cycles were simulated to induce mechanical fatigue (Biocycle; Biopdi, São Paulo, SP, Brazil) by immersing the samples in water at 37
oC and cycling 1,200,000 times. A load of 0–50 N at 45° and a frequency of 2 Hz was applied to the palatal surface of the teeth using a stainless-steel cylindrical-shaped tip. Each specimen was arranged in a mounting jig such that the load was applied to the palatal surface at a 45° angle with the long axis of the tooth. The fracture was induced in the specimens by applying compressive loads with crosshead speeds of 0.5 mm/min in a universal testing machine (Instron model 3344, Instron; Norwood, MA, USA) fitted with a 5000 N load cell [
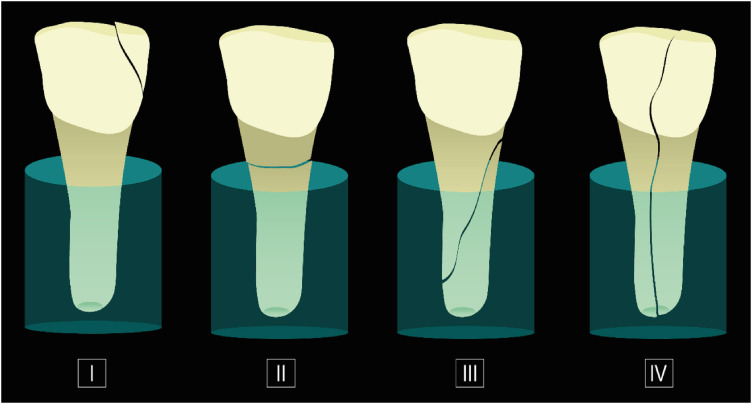
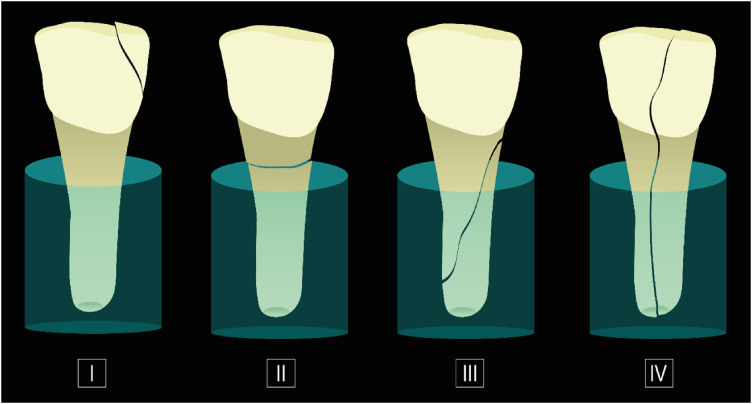
18]. Both the fracture load (N) and the fracture location were recorded. The fracture modes were analyzed using the scale shown in
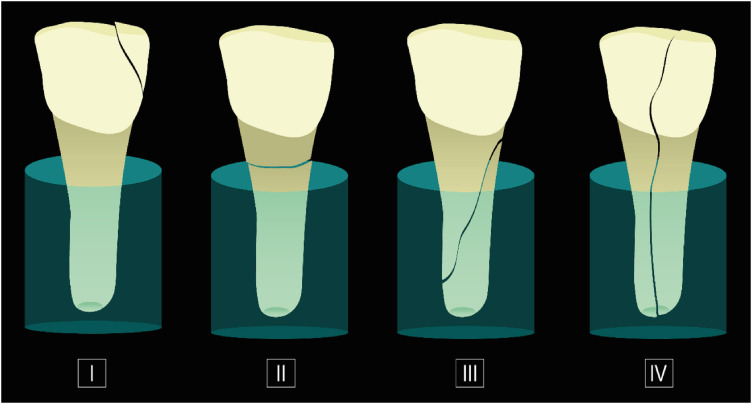
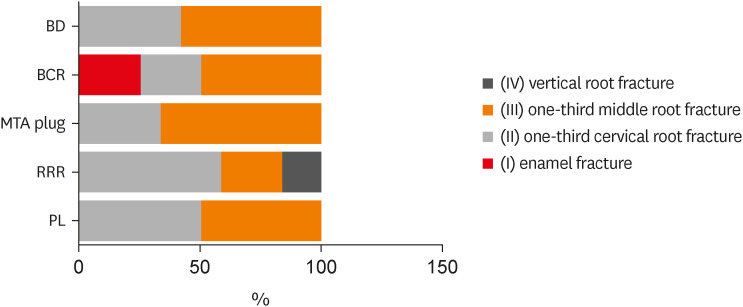
Figure 1.
Figure 1Classification of the fracture modes – (I) enamel fracture; (II) one-third cervical root fracture; (III) one-third middle root fracture; (IV) vertical root fracture.
Cell culture assays
Preparation of material extracts
MTA, BCR, and BD were mixed according to the manufacturers’ instructions under sterile conditions, and the extracts were prepared as previously described [
8]. The materials were shaped in cylindrical polyethylene molds (diameter, 5 mm; height, 2 mm) and incubated under humidified conditions at 37°C for 24 hours to allow for complete setting. After this period, the specimens were immersed in α-minimal essential medium (α-MEM) (LGC Biotechnology, Cotia, SP, Brazil) for 24 hours at 37°C and 5% CO
2 in a humid atmosphere. Following the ISO 10993-5 guidelines, a material surface area/medium volume ratio of approximately 1.5 cm
2/mL was obtained [
19]. After incubation, the original extracts were filtered and serially diluted in cell culture medium to a dilution of 1:16 before testing.
Cell cytotoxicity assay
A murine RAW 264.7 macrophage cell lineage was obtained from the Cell Bank of Rio de Janeiro (Rio de Janeiro, RJ, Brazil). The cells were cultured until confluence in α-MEM supplemented with 10% fetal bovine serum (FBS; Gibco, Invitrogen, Carlsbad, CA, USA) and 1% penicillin-streptomycin (Sigma-Aldrich, St. Louis, MO, USA). After this period, RAW 264.7 cells were seeded in a 96-well plate and exposed or not (control group) to diluted extracts (1:1–1:16) for 24 hours. Next, the 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) reagent (Thermo Fisher Scientific, Waltham, MA, USA) was prepared at 5 mg/mL, and 10% MTT diluted in α-MEM was added to each well for 4 hours. After this period, 100 μL of dimethylsulfoxide (Sigma-Aldrich) was added to each well for approximately 2 minutes. Subsequently, the optical density (OD) at 570 nm of the cells was measured using a microplate reader (Biochrom, Cambridge, UK). Cell viability was expressed as the percentage of OD of the experimental wells relative to that of the control, according to the following formula:
where A = viable cells in the experimental well and B = viable cells in the control well. The assay was performed in quadruplicate (n = 4), and the trial was repeated twice under the same conditions. A dilution that demonstrated a cell viability higher than 80% was used for the osteoclastogenesis assay (1:16).
Osteoclastogenesis induction and exposure to the extracts
RAW 264.7 cells were seeded (2 × 10
4 cells/well) on a 96-well plate in α-MEM supplemented with 10% FBS and 1% penicillin-streptomycin and allowed to adhere overnight. For osteoclast-like formation, the cells were stimulated with 1:16 diluted extracts of materials and 100 ng/mL receptor activator of nuclear factor-kappa B ligand (RANKL) (PeproTech, Rocky Hill, NJ, USA) for 5 days. On day three, the medium and RANKL were changed [
20,
21]. The negative control group contained cells maintained in 10% α-MEM (not induced to differentiation), and the positive control group contained cells kept in RANKL without extract treatment. Samples were then prepared for quantification of tartrate-resistant acid phosphatase (TRAP) activity. The assay was performed in quadruplicate (
n = 4), and the trial was repeated twice under the same conditions.
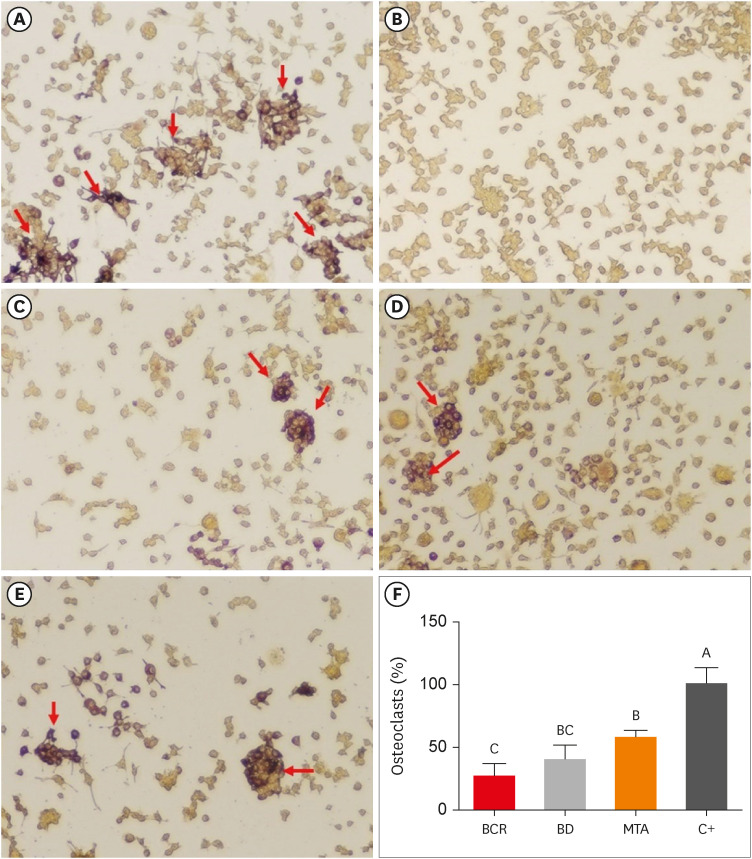
Tartrate-resistant acid phosphatase staining
The cells were washed with phosphate-buffered saline (PBS; Gibco) and fixed for 30 seconds with a liquid containing citrate, acetone, and formaldehyde. Next, the cells were stained using an acid phosphatase leukocyte TRAP kit (Sigma-Aldrich) in accordance with the manufacturer’s recommendations. TRAP-positive cells were evident due to the appearance of cytoplasmic granules marked by dark red to purple deposits. The number of osteoclasts formed per well was represented by TRAP-positive multinucleated cells with 3 or more nuclei [
20,
21]. Four images of each well were taken at the top left, top right, bottom left, and bottom right, with 10 × magnification using a Leica DM IRB-inverted microscope coupled to a DFC490 camera (Leica, Wetzlar, HE, Germany). The results were expressed as the percentage of TRAP-positive cells identified per field in each well compared to that observed in the positive control group [
20].
Statistical analyses were performed using GraphPad Prism 7 (GraphPad Software, San Diego, CA, USA). All data were analyzed for normality and homoscedasticity using Shapiro-Wilk’s and Levene’s tests. Fracture loads and osteoclast numbers were analyzed using 1-way analysis of variance (ANOVA) and Tukey’s multiple comparison test to ascertain any significant differences between groups. The fracture modes were also qualitatively evaluated. To determine cell viability, 2-way ANOVA and Tukey's test were used to compare the data between the treated groups. Dunnett's test was used to compare the experimental groups to the control group. Statistical significance was set at α = 0.05.
RESULTS
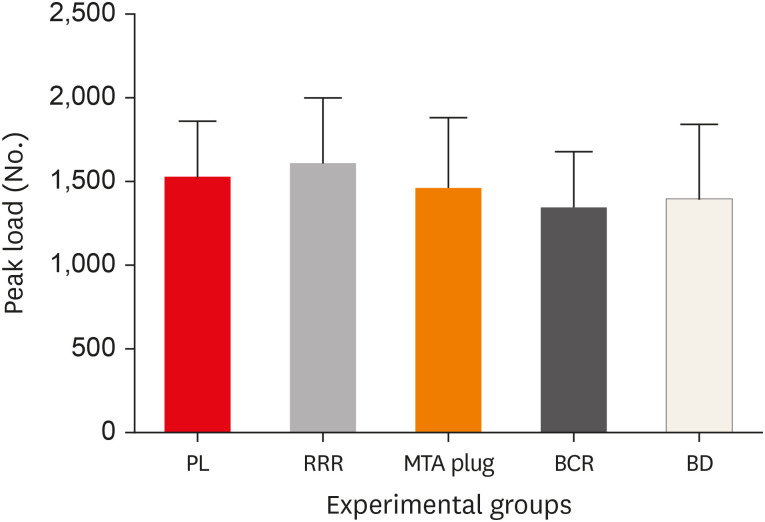
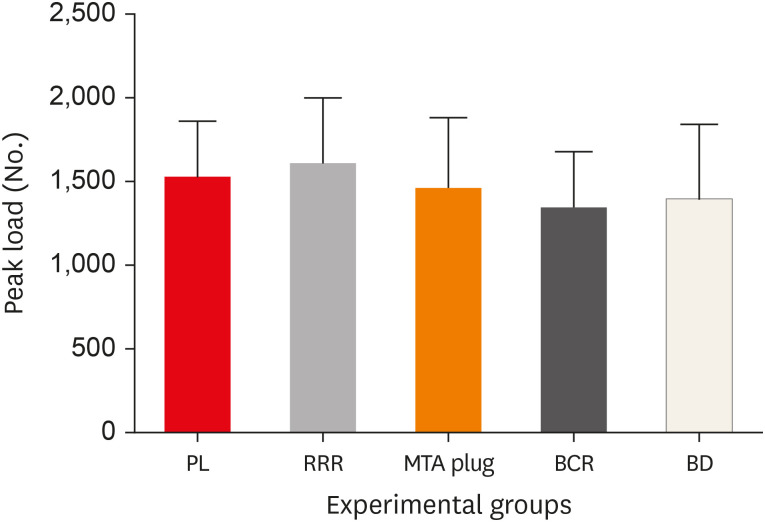
Fracture testing
The results of the fracture testing are presented in
Table 2 and
Figure 2. There were no statistically significant differences in fracture resistance among the 5 groups evaluated (1-way ANOVA, F = 0.872,
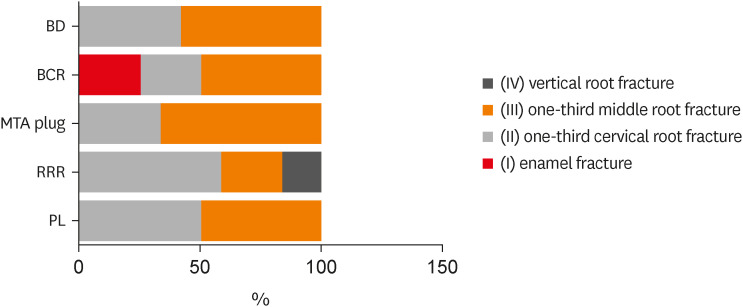
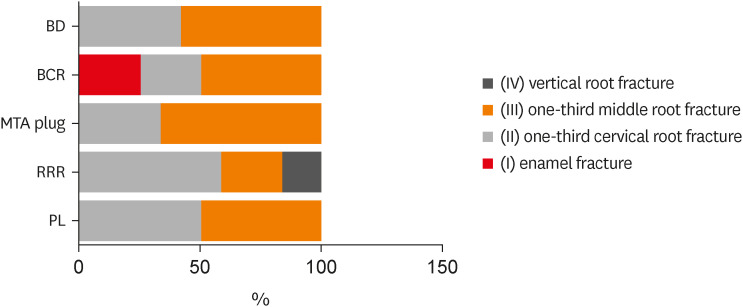
p =0.487). All teeth filled with MTA plugs, BCR, and BD were fractured in the cervical and middle thirds, except for three samples in the BCR group, which showed enamel fractures. In addition, the teeth in the RRR group tended to fracture mainly in the cervical and middle thirds; however, 2 samples had vertical root fractures (
Figure 3).
Table 2Mean ± standard deviation of fracture resistance in the experimental groups
|
Experimental groups |
Values |
|
PL |
1,519 ± 343.3A
|
|
RRR |
1,609 ± 390.5A
|
|
MTA Plug |
1,453 ± 375.5A
|
|
BCR |
1,337 ± 342.3A
|
|
BD |
1,390 ± 354.1A
|
Figure 2
The number of mean peak load and standard deviations required to cause root fractures in each experimental group.
PL: normal periodontal ligament; RRR: replacement root resorption; MTA plug: apical plug with MTA and root canal filling with Bio-C sealer and gutta-percha; BCR: Bio-C repair root canal filling; BD: Biodentine root canal filling.
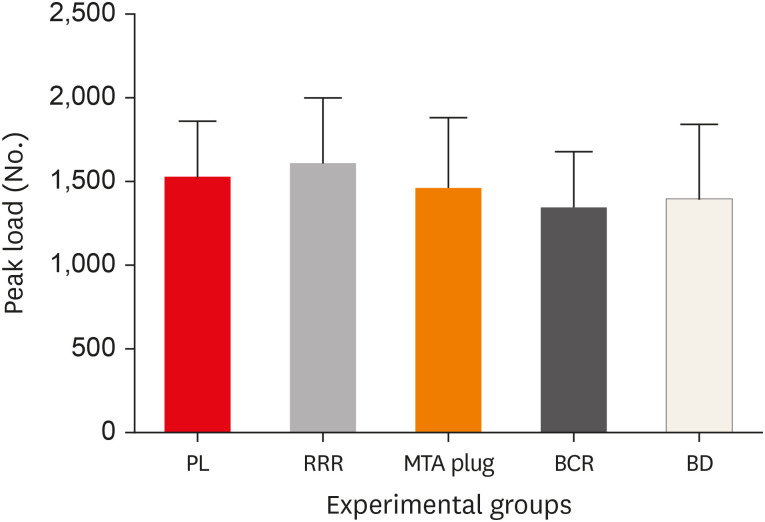
Figure 3
Fracture modes of the specimens after load tests.
BD: Biodentine; BCR: Bio-C Repair; MTA: mineral trioxide aggregate; RRR: replacement root resorption; PL: periodontal ligament.
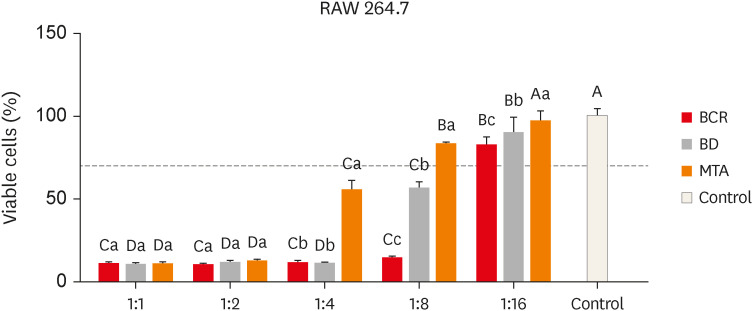
Cell cytotoxicity assay
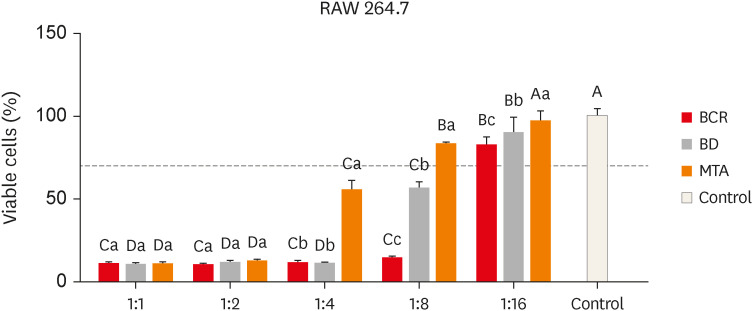
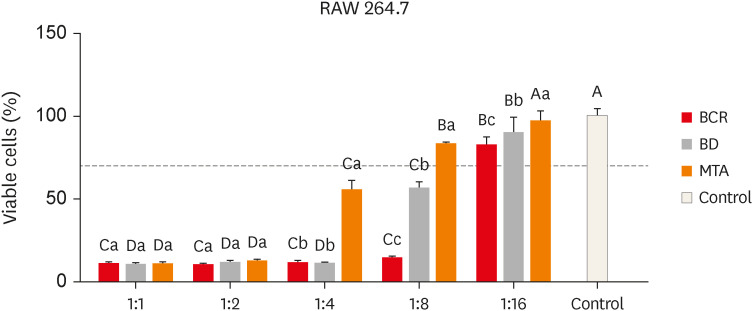
RAW 264.7 viability results of BCR, BD and MTA groups with different extract dilutions are shown in
Figure 4. The “dilution” and “material” factors significantly influenced the viability of macrophages (
p < 0.0001). In addition, the interaction of the factors had a significant effect on the MTT assay result (2-way ANOVA, F = 77.97,
p < 0.0001). There were no statistically significant differences in the viability of the cells exposed to the 1:1 and 1:2 dilutions, regardless of the material evaluated (
p > 0.05). The MTA group showed the highest viability values at dilutions of 1:4, 1:8, and 1:16 (
p < 0.0001). For all the materials evaluated, the highest percentage of viable cells was found with the 1:16 dilution (
p < 0.0001). All the groups showed lower viability than the control group (
p < 0.0001), except for MTA at 1:16 dilution, which showed similar values (
p > 0.05).
Figure 4
Cell viability percentage (%) of RAW 264.7 cells after exposure to extracts. Capital letters indicate comparisons between different material’s dilutions and the control group for each material. Lowercase letters indicate comparisons between materials and dilutions. Groups identified by the same letter are not significantly different (p > 0.05). Two-way analysis of variance and Tukey’s test (p < 0.05).
BCR: Bio-C Repair; BD: Biodentine; MTA: mineral trioxide aggregate.
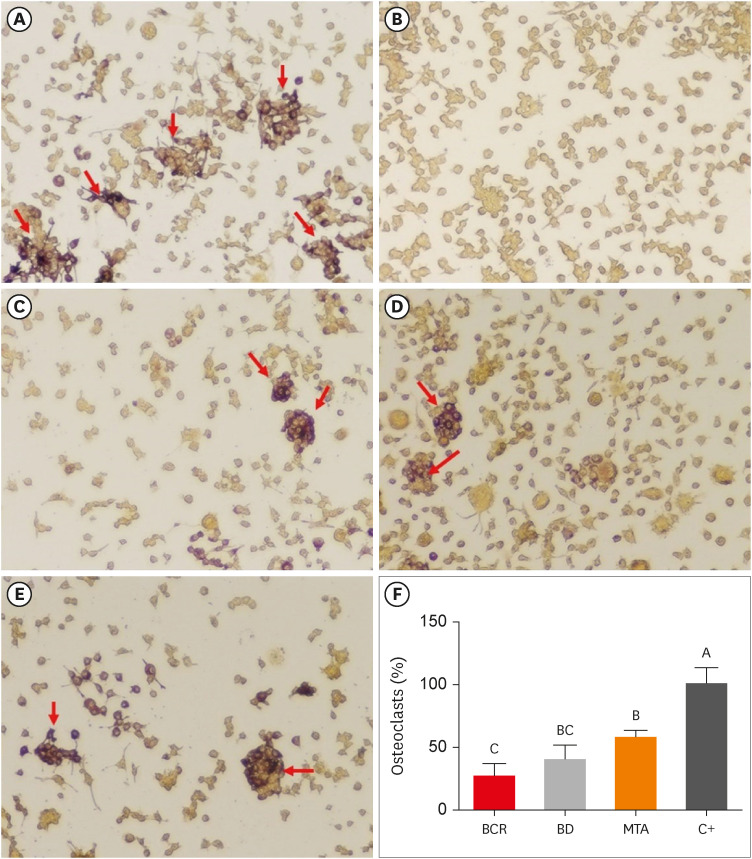
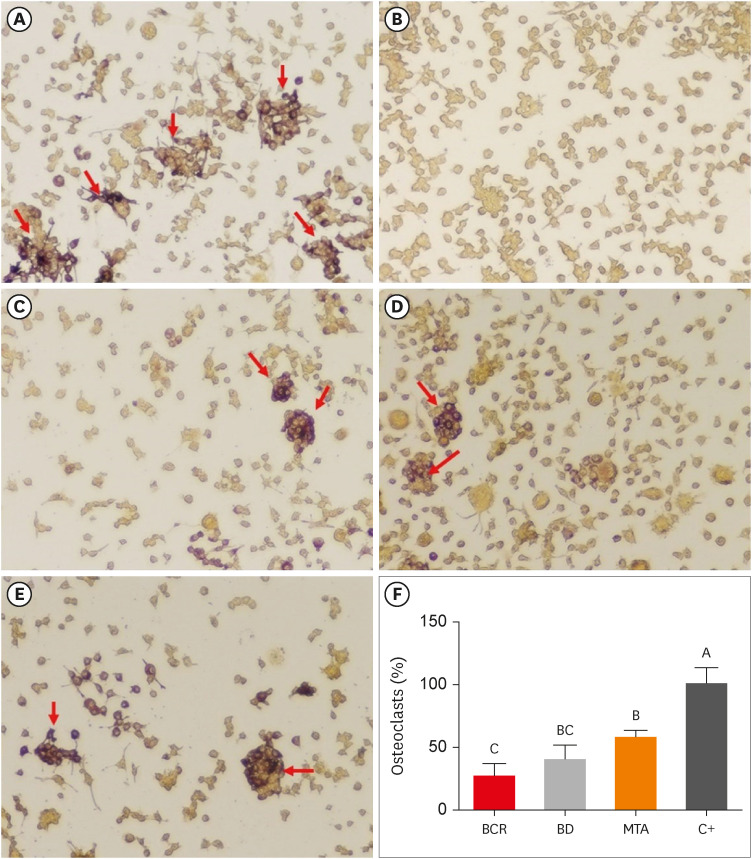
TRAP staining
Compared with the negative control RAW 264.7 cells, the RANKL-induced RAW 264.7 cells differentiated into TRAP-positive multinucleated osteoclasts. However, the number of TRAP-positive osteoclasts decreased after treatment with the extracts (
p < 0.0001). The percentage of TRAP-positive cells was similar comparing BD and MTA, and BD and BCR (
p > 0.05). BCR group showed a lower percentage of osteoclasts than the MTA group (
p < 0.0001) (
Figure 5).
Figure 5
TRAP staining. (A) Positive control (RANKL); (B) Negative control (α-minimal essential medium); (C) Cells treated with Bio-C repair extract; (D) Cells treated with Biodentine extract; (E) Cells treated with MTA extract. TRAP-positive multinucleated cells (arrow); 10× magnification. (F) TRAP activity: capital letters indicate comparisons among the materials tested. Groups identified by the same letter are not significantly different (p > 0.05).
BCR: Bio-C Repair; BD: Biodentine; MTA, mineral trioxide aggregate; TRAP: tartrate-resistant acid phosphatase; RANKL, receptor activator of nuclear factor-kappa B ligand.
DISCUSSION
In this study, the null hypothesis was rejected as significant differences were found between groups treated with different calcium silicate-based materials in the cell culture assays. However, the evaluated materials did not affect the fracture resistance of the immature permanent teeth subjected to RRR. Previous studies have emphasized the importance of strengthening the teeth that are in the early stages of development [
12,
15]. Dentin deposition on the root canals is not enough to reinforce the teeth, which are consequently predisposed to fracture [
22]. Furthermore, it is important that the
in vitro tests can reproduce the bone capacity to absorb masticatory load and support compressive and tangential forces in a fracture resistance test even under adverse conditions such as RRR. In this study, RRR was simulated through a combined protocol employing cylindrical drill wear and acid demineralization, with the selective inclusion of roots with elastomeric impression materials and polystyrene resin [
16]. The biomechanical characteristics of the polystyrene resin differ from those of bone tissue, which represents a limitation of the study. Nonetheless, the simulation was performed in the same manner in all groups, to closely resemble the clinical situation. Furthermore, it is not possible to replicate the irregularities of the resorption cavities and regions with the absence of PL and ankylosis; therefore, the results may vary in clinical situations and should be analyzed with caution.
RRR occurs progressively, and it irregularly advances to the point of complete replacement of the root by bone [
3]. Considering this pattern and the fact that ankylosis occurs significantly more often on the rounded labial and lingual surfaces than on the flat or proximal concave surfaces, this study simulated ankylosis and RRR only on the palatal root surface [
23]. In addition, previous studies have demonstrated that immature maxillary incisors exhibit a high concentration of tensile stress on the palatal root surface, which is located within the structure that is more prone to failure [
15].
In this study, the group with simulated ankylosis and RRR had a fracture load similar to that of the normal PL group. Notably, a previous study showed that teeth embedded directly in polystyrene resin have lower fracture resistance than those in which PDL simulation is performed [
17]. In these cases, PDL acts as a sustaining pad, thereby reducing alveolar bone stress [
24]. When a force is applied, the tooth moves away from the rotation center that is compressing the periodontal fibers and causes bone distortion in the direction of the root movement [
25]. Initially, the resistance of the periodontal fibers against the tooth displacement is low; however, as the tooth is forced within its alveolus, the load progressively increases [
17]. In this study, the PL was partially simulated, which could explain the similarity between the groups.
In a previous study, CSM enhanced the resistance to horizontal root fractures when used as obturating materials for immature teeth [
12]. Nonetheless, our results suggest that these materials cannot increase the fracture resistance of immature teeth with RRR. Moreover, there were no differences between the MTA plug group and the groups filled with the repair materials. These findings are consistent with those of previous studies and may be related to the limited ability of the CSM materials to bond to root dentin [
26,
27,
28]. In addition, a retrospective clinical study demonstrated that immature teeth treated with MTA apexification and filled with gutta-percha or filled with MTA exhibited a similar rate of root fracture [
29]. However, it is important to emphasize that the results of laboratory studies must be considered with caution and cannot be directly compared to those of clinical studies.
The mechanical tests in this study were carried out in bovine teeth because they have similar ultimate tensile strengths, dentine moduli of elasticity, and similar numbers, distributions, and diameters of dentinal tubules to human teeth [
30,
31,
32]. Furthermore, a prior study established that bovine teeth can be used safely as substitutes for human teeth in fracture strength tests [
33].
BCR is a CSM that was launched in the second half of 2019 with a ready-to-use protocol containing calcium silicate, calcium oxide, zirconium oxide, iron oxide, silicon dioxide, and a dispersing agent [
9]. The absence of significant differences between the fracture values of the BD and BCR groups in this study could be attributed to the chemical/molecular similarities between these materials. Although there are no studies evaluating the fracture resistance of teeth filled with BCR, to the best of our knowledge, this material has cytotoxicity and mineralization-inducing abilities similar to those of BD [
7,
10]. However, a recent study showed that the compressive and adhesion strengths of this material are lower than those of BD [
34].
The fractures in this study were mainly concentrated in the cervical and middle thirds of the roots. However, in the group simulating a normal PL, the fracture pattern was more homogeneous compared to that in the groups with RRR. This is because the PL transfers the stresses produced by the application of pressure over the coronal tooth structure to all the root surfaces [
17]. Therefore, the teeth in the RRR, BCR, BD, and MTA plug groups presented more heterogeneous fracture patterns. Despite the similar fracture patterns between the teeth filled with CSM and gutta-percha, previous studies have shown that complete root canal filling with calcium silicate-based materials can be advantageous for an optimal biomechanical response [
35]. This is because filling with CSM creates a monoblock with an interface that extends between the material and the canal walls [
36]. In particular, BD is an ideal dentin replacement material, and it has been reported to decrease stress at the cervical root region by keeping the stress in its center while transferring stress to the mid-coronal region [
35].
In this study, the murine macrophage lineage RAW 264.7 was used for the induction of osteoclastogenesis as these cells express RANK and can indefinitely grow as osteoclast precursors or differentiate into osteoclasts when co-cultured with RANKL. Although the choice of permanent cell lines as study models is controversial, the RAW osteoclasts exhibit the essential characteristics of osteoclasts, notably the expression of TRAP and cathepsin K [
37,
38]. Furthermore, the use of immortalized cell cultures in a preliminary study assessing new materials, such as BCR, allows greater control of variables and easy reproducibility, and has been recommended in the literature [
20,
21].
Although previous studies have evaluated the cytotoxicity of these materials, this parameter is influenced by the cell type evaluated. Therefore, our viability analysis was conducted using RAW 264.7 to define a concentration at which all experimental groups presented with viability parameters > 70% and would not interfere with future osteoclastogenesis assays.
According to ISO 10993-5:2009, biomaterials that cause a reduction in cell viability by more than 30% are considered cytotoxic [
19]. In the present study, the RAW 264.7 lineage showed cell viability rates > 70% only in the 1:16 dilution, suggesting that this cell line can be sensitive to the components present in the materials. These results differ from other studies that employed the same methodology, which reported human dental pulp cells viabilities > 80% even at 1:1 dilutions [
8,
39]. In another study, the biocompatibility and osteogenesis-inducing potential of BD, BCR, and MTA in cultures of human osteoblastic cells (SAOS-2) were evaluated, and the resulting cells demonstrated similar cell viability rates to those of the controls [
10]. Different cell lineages may present divergent biological responses to each other, highlighting the relevance of performing cell viability analyses in different culture models [
10]. Previous studies have shown that MTA did not affect RAW 264.7 viability after 24 hours and that BD and MTA were not cytotoxic to macrophages after 48 hours or 72 hours of incubation [
21,
40]. Despite that, aspects such as setting time, direct or indirect contacts and the preparation of the material extracted can directly influence the biocompatibility and bioactivity of the material, which prevents direct comparisons between studies [
10]. The cell viability analysis method using different materials dilutions has wide support in the literature [
8,
10,
40]. However, this method has its own limitations, as it is not possible to accurately quantify the components released by each CSM in the extracellular fluid.
RAW 264.7 osteoclasts express active TRAP enzymes, which are key markers involved in osteoclastic bone resorption. The results of this study showed that TRAP-positive multinucleated osteoclasts were induced at the highest rate in the positive control group, which is consistent with previous results [
40]. All calcium-silicate cements evaluated showed a reduction in the number of differentiated osteoclasts. This is also in agreement with recent studies that reported that calcium silicate cements prevent osteoclastogenesis and bone resorption, consequently enhancing bone remodeling [
40,
41]. In addition, significant differences were not observed in the number of osteoclasts between the BD and MTA groups, as observed in other studies [
40,
42]. This may be associated with the similarity in the composition of the 2 materials [
7]. Nevertheless, structural differences in osteoclasts, such as osteoclast size, the number of nuclei per cell, and the relationship between the contact of osteoclasts with the bone surface, are parameters directly associated with the cells’ resorptive activity [
43]. Moreover, laboratory studies in rats have demonstrated increased bone losses in regions of furcation perforation sealing when using BD compared to MTA, despite the lack of statistical differences in the number of osteoclasts [
42].
In contrast to the other materials, BCR presented the lowest number of osteoclasts, which may be due to the lower concentration of calcium in its structure and the lower amount of calcium ions released in its solution compared to MTA and BD [
7,
8]. High extracellular calcium concentrations modulate osteoclast differentiation and function, and osteoclastic bone resorption is directly regulated by calcitonin, and locally by ionized calcium (Ca
2+) generated as a result of osteoclastic bone resorption [
44]. Furthermore, high concentrations of extracellular calcium cause cellular changes that markedly inhibit the TRAP enzyme and bone resorption [
21].
A recent study demonstrated that BD microparticles and soluble leachable components at non-cytotoxic concentrations have anti-inflammatory, immunomodulatory effects and osteoprotective properties [
45]. The mechanisms responsible for these included the suppression of several cytokines and the RANKL/Osteoprotegerin (OPG) ratio decrease [
45]. In the clastic maturation process, RANKL binds its cognate RANK receptor on the surface of monocytes and macrophages and triggers their differentiation into mature multinucleated osteoclasts with bone resorption activity [
46]. The action of RANKL is suppressed by its natural inhibitor OPG. OPG blocks RANKL/RANK interaction, and by doing this, it inhibits osteoclast activation and subsequent bone resorption [
46]. In this sense, future studies should evaluate the effects of other materials based on calcium-silicate on the OPG/RANK/RANKL ratio, which could provide important information about the osteoprotective mechanism of these materials.
Traumatized immature permanent teeth have thin walls, are more prone to fracture, are difficult to obturate using conventional methods, and have accelerated resorptive processes. Therefore, it is essential to choose biomaterials that facilitate execution do not affect fracture resistance, and can control the healing process/resorption until the patient completes their craniofacial development.
CONCLUSIONS
In conclusion, the treatment options evaluated for non-vital immature teeth with RRR did not strengthen the teeth and provided similar resistance to fractures. BD, MTA, and BCR showed inhibitory effects on osteoclast differentiation, with BCR yielding more promising results.
ACKNOWLEDGEMENTS
This project was developed at CPBio – Biomechanics, Biomaterials, and Cell Biology Research Center of the Universidade Federal de Uberlândia. The research was financed in part by the Fundação de Amparo à Pesquisa do Estado de Minas Gerais (Finance code: APQ-02660-21; APQ-04262-22), Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES) (Finance code 001).
-
Funding: The research was financed in part by Fundação de Amparo à Pesquisa do Estado de Minas Gerais (Finance code: APQ-02660-21; APQ-04262-22); Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES) (Finance code 001).
-
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
-
Author Contributions:
Conceptualization: Souza GL, Moura CCG, and Soares CJ.
Data curation: Souza GL, Moura CCG, and Soares CJ.
Formal analysis: Souza GL, Moura CCG, and Soares CJ.
Funding acquisition: Moura CCG.
Investigation: Souza GL, Ribeiro MTH, Freitas GAN, and Lemus NXA.
Methodology: Souza GL, Ribeiro MTH, Freitas GAN, and Lemus NXA.
Project administration: Moura CCG.
Resources: Moura CCG.
Software: Souza GL and Ribeiro MTH.
Supervision: Moura CCG.
Validation: Souza GL, Moura CCG, and Soares CJ.
Visualization: Souza GL, Moura CCG, and Soares CJ.
Writing - original draft: Souza GL, Freitas GAN, Ribeiro MTH, Lemus NXA, Soares CJ, and Moura CCG.
Writing - review & editing: Souza GL, Freitas GAN, Ribeiro MTH, Lemus NXA, Soares CJ, and Moura CCG.
SUPPLEMENTARY MATERIAL
REFERENCES
- 1. Rocha Lima TF, Nagata JY, de Souza-Filho FJ, de Jesus Soares A. Post-traumatic complications of severe luxations and replanted teeth. J Contemp Dent Pract 2015;16:13-19.ArticlePubMed
- 2. de Souza BD, Dutra KL, Reyes-Carmona J, Bortoluzzi EA, Kuntze MM, Teixeira CS, Porporatti AL, De Luca Canto G. Incidence of root resorption after concussion, subluxation, lateral luxation, intrusion, and extrusion: a systematic review. Clin Oral Investig 2020;24:1101-1111.ArticlePubMedPDF
- 3. Galler KM, Grätz EM, Widbiller M, Buchalla W, Knüttel H. Pathophysiological mechanisms of root resorption after dental trauma: a systematic scoping review. BMC Oral Health 2021;21:163.ArticlePubMedPMCPDF
- 4. Panzarini SR, Sonoda CK, Saito CT, Hamanaka EF, Poi WR. Delayed tooth replantation: MTA as root canal filling. Braz Oral Res 2014;28:1-7.Article
- 5. Torabinejad M, Parirokh M, Dummer PM. Mineral trioxide aggregate and other bioactive endodontic cements: an updated overview - part II: other clinical applications and complications. Int Endod J 2018;51:284-317.ArticlePubMedPDF
- 6. Kaur M, Singh H, Dhillon JS, Batra M, Saini M. MTA versus Biodentine: review of literature with a comparative analysis. J Clin Diagn Res 2017;11:ZG01-ZG05.ArticlePubMedPMC
- 7. Ghilotti J, Sanz JL, López-García S, Guerrero-Gironés J, Pecci-Lloret MP, Lozano A, Llena C, Rodríguez-Lozano FJ, Forner L, Spagnuolo G. Comparative surface morphology, chemical composition, and cytocompatibility of Bio-C Repair, Biodentine, and ProRoot MTA on hDPCs. Materials (Basel) 2020;13:2189.ArticlePubMedPMC
- 8. Oliveira LV, de Souza GL, da Silva GR, Magalhães TE, Freitas GA, Turrioni AP, de Rezende Barbosa GL, Moura CC. Biological parameters, discolouration and radiopacity of calcium silicate-based materials in a simulated model of partial pulpotomy. Int Endod J 2021;54:2133-2144.ArticlePubMedPDF
- 9. Benetti F, Queiroz ÍO, Cosme-Silva L, Conti LC, Oliveira SH, Cintra LT. Cytotoxicity, biocompatibility and biomineralization of a new ready-for-use Bioceramic repair material. Braz Dent J 2019;30:325-332.ArticlePubMed
- 10. Santiago MC, Gomes-Cornélio AL, de Oliveira LA, Tanomaru-Filho M, Salles LP. Calcium silicate-based cements cause environmental stiffness and show diverse potential to induce osteogenesis in human osteoblastic cells. Sci Rep 2021;11:16784.ArticlePubMedPMCPDF
- 11. Karapinar-Kazandag M, Basrani B, Tom-Kun Yamagishi V, Azarpazhooh A, Friedman S. Fracture resistance of simulated immature tooth roots reinforced with MTA or restorative materials. Dent Traumatol 2016;32:146-152.PubMed
- 12. Linsuwanont P, Kulvitit S, Santiwong B. Reinforcement of simulated immature permanent teeth after mineral trioxide aggregate apexification. J Endod 2018;44:163-167.ArticlePubMed
- 13. Nagendrababu V, Murray PE, Ordinola-Zapata R, Peters OA, Rôças IN, Siqueira JF Jr, Priya E, Jayaraman J, J Pulikkotil S, Camilleri J, Boutsioukis C, Rossi-Fedele G, Dummer PM. PRILE 2021 guidelines for reporting laboratory studies in endodontology: a consensus-based development. Int Endod J 2021;54:1482-1490.ArticlePubMedPDF
- 14. Tanalp J, Dikbas I, Malkondu O, Ersev H, Güngör T, Bayırlı G. Comparison of the fracture resistance of simulated immature permanent teeth using various canal filling materials and fiber posts. Dent Traumatol 2012;28:457-464.ArticlePubMed
- 15. Brito-Júnior M, Pereira RD, Veríssimo C, Soares CJ, Faria-e-Silva AL, Camilo CC, Sousa-Neto MD. Fracture resistance and stress distribution of simulated immature teeth after apexification with mineral trioxide aggregate. Int Endod J 2014;47:958-966.ArticlePubMed
- 16. Vieira HT, Vizzotto MB, da Silveira PF, Arús NA, Corrêa Travessas JA, da Silveira HL. Diagnostic efficacy of different cone beam computed tomography scanning protocols in the detection of chemically simulated external root resorption. Oral Surg Oral Med Oral Pathol Oral Radiol 2020;130:322-327.ArticlePubMed
- 17. Soares CJ, Pizi EC, Fonseca RB, Martins LR. Influence of root embedment material and periodontal ligament simulation on fracture resistance tests. Braz Oral Res 2005;19:11-16.ArticlePubMed
- 18. Mello I, Michaud PL, Butt Z. Fracture resistance of immature teeth submitted to different endodontic procedures and restorative protocols. J Endod 2020;46:1465-1469.ArticlePubMed
- 19. ISO 10993-5 - biological evaluation of medical devices- part 5: tests for in vitro cytotoxicity. Geneva, Switzerland: ISO; 2009.
- 20. Reis MV, de Souza GL, Moura CC, da Silva MV, Souza MA, Soares PB, Soares CJ. Effects of Lectin (ScLL) on osteoclast-like multinucleated giant cells’ maturation: a preliminary in vitro study. Dent Traumatol 2018;34:329-335.PubMed
- 21. Rezende TM, Ribeiro Sobrinho AP, Vieira LQ, Sousa MG, Kawai T. Mineral trioxide aggregate (MTA) inhibits osteoclastogenesis and osteoclast activation through calcium and aluminum activities. Clin Oral Investig 2021;25:1805-1814.ArticlePubMedPDF
- 22. Elnaghy A, Elsaka S. Fracture resistance of simulated immature roots using Biodentine and fiber post compared with different canal-filling materials under aging conditions. Clin Oral Investig 2020;24:1333-1338.ArticlePubMedPDF
- 23. Andreasen JO. Analysis of pathogenesis and topography of replacement root resorption (ankylosis) after replantation of mature permanent incisors in monkeys. Swed Dent J 1980;4:231-240.PubMed
- 24. Fongsamootr T, Suttakul P. Effect of periodontal ligament on stress distribution and displacement of tooth and bone structure using finite element simulation. Eng J (NY) 2015;19:99-108.Article
- 25. Marchionatti AM, Wandscher VF, Broch J, Bergoli CD, Maier J, Valandro LF, Kaizer OB. Influence of periodontal ligament simulation on bond strength and fracture resistance of roots restored with fiber posts. J Appl Oral Sci 2014;22:450-458.ArticlePubMedPMC
- 26. Yasin R, Al-Jundi S, Khader Y. Effect of mineral trioxide aggregate and biodentine™ on fracture resistance of immature teeth dentine over time: in vitro study. Eur Arch Paediatr Dent 2021;22:603-609.ArticlePubMedPDF
- 27. Pandolfo MT, Rover G, Bortoluzzi EA, Teixeira CD, Rossetto HL, Fernades PC, Côrte-Real IS, Carvalho SM, Garcia LD. Fracture resistance of simulated immature teeth reinforced with different mineral aggregate-based materials. Braz Dent J 2021;32:21-31.ArticlePubMed
- 28. de Sá MA, Nunes E, Antunes AN, Brito Júnior M, Horta MC, Amaral RR, Cohen S, Silveira FF. Push-out bond strength and marginal adaptation of apical plugs with bioactive endodontic cements in simulated immature teeth. Restor Dent Endod 2021;46:e53.PubMedPMC
- 29. Danwittayakorn S, Banomyong D, Ongchavalit L, Ngoenwiwatkul Y, Porkaew P. Comparison of the effects of intraradicular materials on the incidence of fatal root fracture in immature teeth treated with mineral trioxide aggregate apexification: a retrospective study. J Endod 2019;45:977-984.e1.ArticlePubMed
- 30. Sano H, Ciucchi B, Matthews WG, Pashley DH. Tensile properties of mineralized and demineralized human and bovine dentin. J Dent Res 1994;73:1205-1211.ArticlePubMedPDF
- 31. Schilke R, Lisson JA, Bauss O, Geurtsen W. Comparison of the number and diameter of dentinal tubules in human and bovine dentine by scanning electron microscopic investigation. Arch Oral Biol 2000;45:355-361.ArticlePubMed
- 32. Reis AF, Giannini M, Kavaguchi A, Soares CJ, Line SR. Comparison of microtensile bond strength to enamel and dentin of human, bovine, and porcine teeth. J Adhes Dent 2004;6:117-121.PubMed
- 33. Soares CJ, Barbosa LM, Santana FR, Soares PB, Mota AS, Silva GR. Fracture strength of composite fixed partial denture using bovine teeth as a substitute for human teeth with or without fiber-reinforcement. Braz Dent J 2010;21:235-240.ArticlePubMed
- 34. Rodrigues MN, Bruno KF, de Alencar AH, Silva JD, de Siqueira PC, Decurcio DA, Estrela C. Comparative analysis of bond strength to root dentin and compression of bioceramic cements used in regenerative endodontic procedures. Restor Dent Endod 2021;46:e59.ArticlePubMedPMCPDF
- 35. Belli S, Eraslan O, Eskitaşcıoğlu G. Effect of different treatment options on biomechanics of immature teeth: a finite element stress analysis study. J Endod 2018;44:475-479.ArticlePubMed
- 36. Tay FR, Pashley DH. Monoblocks in root canals: a hypothetical or a tangible goal. J Endod 2007;33:391-398.ArticlePubMedPMC
- 37. Honegger P. Overview of cell and tissue culture techniques. Curr Protocols Pharmacol 2001;Chapter 12:12.1.ArticlePDF
- 38. Collin-Osdoby P, Osdoby P. RANKL-mediated osteoclast formation from murine RAW 264.7 cells. Methods Mol Biol 2012;816:187-202.ArticlePubMed
- 39. Oliveira LV, da Silva GR, Souza GL, Magalhães TE, Barbosa GL, Turrioni AP, Moura CC. A laboratory evaluation of cell viability, radiopacity and tooth discoloration induced by regenerative endodontic materials. Int Endod J 2020;53:1140-1152.ArticlePubMedPDF
- 40. Kim M, Kim S, Ko H, Song M. Effect of ProRoot MTA® and Biodentine® on osteoclastic differentiation and activity of mouse bone marrow macrophages. J Appl Oral Sci 2019;27:e20180150.ArticlePubMedPMC
- 41. Cheng X, Zhu L, Zhang J, Yu J, Liu S, Lv F, Lin Y, Liu G, Peng B. Anti-osteoclastogenesis of mineral trioxide aggregate through inhibition of the autophagic pathway. J Endod 2017;43:766-773.ArticlePubMed
- 42. da Fonseca TS, Silva GF, Guerreiro-Tanomaru JM, Delfino MM, Sasso-Cerri E, Tanomaru-Filho M, Cerri PS. Biodentine and MTA modulate immunoinflammatory response favoring bone formation in sealing of furcation perforations in rat molars. Clin Oral Investig 2019;23:1237-1252.ArticlePubMedPDF
- 43. Faloni AP, Sasso-Cerri E, Rocha FR, Katchburian E, Cerri PS. Structural and functional changes in the alveolar bone osteoclasts of estrogen-treated rats. J Anat 2012;220:77-85.ArticlePubMed
- 44. Zaidi M, Adebanjo OA, Moonga BS, Sun L, Huang CL. Emerging insights into the role of calcium ions in osteoclast regulation. J Bone Miner Res 1999;14:669-674.ArticlePubMedPDF
- 45. Eraković M, Duka M, Bekić M, Tomić S, Ismaili B, Vučević D, Čolić M. Anti-inflammatory and immunomodulatory effects of Biodentine on human periapical lesion cells in culture. Int Endod J 2020;53:1398-1412.ArticlePubMedPDF
- 46. Petean IB, Küchler EC, Soares IM, Segato RA, Silva LA, Antunes LA, Salles AG, Antunes LS, Sousa-Neto MD. Genetic polymorphisms in RANK and RANKL are associated with persistent apical periodontitis. J Endod 2019;45:526-531.ArticlePubMed
 , Gabrielle Alves Nunes Freitas2
, Gabrielle Alves Nunes Freitas2 , Maria Tereza Hordones Ribeiro3
, Maria Tereza Hordones Ribeiro3 , Nelly Xiomara Alvarado Lemus1
, Nelly Xiomara Alvarado Lemus1 , Carlos José Soares3
, Carlos José Soares3 , Camilla Christian Gomes Moura1
, Camilla Christian Gomes Moura1


 KACD
KACD
 ePub Link
ePub Link Cite
Cite

