Search
- Page Path
- HOME > Search
- Cytotoxicity and biocompatibility of high mol% yttria containing zirconia
- Gulsan Ara Sathi Kazi, Ryo Yamagiwa
- Restor Dent Endod 2020;45(4):e52. Published online October 14, 2020
- DOI: https://doi.org/10.5395/rde.2020.45.e52
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
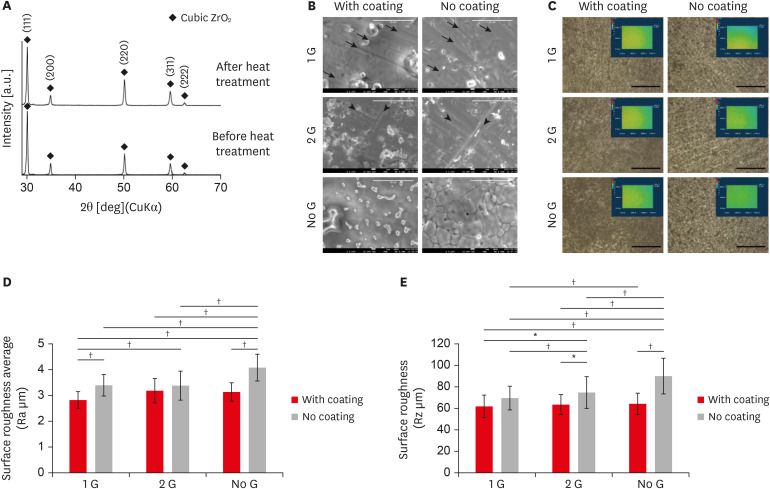
ePub Objectives Yttria-stabilized tetragonal phase zirconia has been used as a dental restorative material for over a decade. While it is still the strongest and toughest ceramic, its translucency remains as a significant drawback. To overcome this, stabilizing the translucency zirconia to a significant cubic crystalline phase by increasing the yttria content to more than 8 mol% (8YTZP). However, the biocompatibility of a high amount of yttria is still an important topic that needs to be investigated.
Materials and Methods Commercially available 8YTZP plates were used. To enhance cell adhesion, proliferation, and differentiation, the surface of the 8YTZP is sequentially polished with a SiC-coated abrasive paper and surface coating with type I collagen. Fibroblast-like cells L929 used for cell adherence and cell proliferation analysis, and mouse bone marrow-derived mesenchymal stem cells (BMSC) used for cell differentiation analysis.
Results The results revealed that all samples, regardless of the surface treatment, are hydrophilic and showed a strong affinity for water. Even the cell culture results indicate that simple surface polishing and coating can affect cellular behavior by enhancing cell adhesion and proliferation. Both L929 cells and BMSC were nicely adhered to and proliferated in all conditions.
Conclusions The results demonstrate the biocompatibility of the cubic phase zirconia with 8 mol% yttria and suggest that yttria with a higher zirconia content are not toxic to the cells, support a strong adhesion of cells on their surfaces, and promote cell proliferation and differentiation. All these confirm its potential use in tissue engineering.
-
Citations
Citations to this article as recorded by- Comparative Evaluation of the Effects of Yttrium Stabilized Zirconia Nanoparticles (YSZrO2- NP) and Porcelain Particles on Property Enhancement of Polymethylmethacrylate (PMMA) Denture Composites
Ihuoma V. Diwe, Henry E. Mgbemere, Olurotimi A. Adeleye, Bolanle Akinboboye
Journal of Biomimetics, Biomaterials and Biomedical Engineering.2026; 70: 21. CrossRef - Phase-separated Zr70-Al12.5Fe17.5Y (x = 0–25 at.%) metallic glasses with suitable mechanical properties for possible implant applications
Devinder Singh, Parthiban Ramasamy, Anna Sophie Jelinek, Verena Maier-Kiener, Rahul Bhattacharya, Zhuo Chen, Elham Sharifikolouei, Alessandro Calogero Scalia, Ziba Najmi, Andrea Cochis, Simon Fellner, Eray Yüce, Christoph Gammer, Zaoli Zhang, Jürgen Ecker
Journal of Materials Research and Technology.2025; 35: 6468. CrossRef - Rapid and straightforward preparation of sturdy ZrO2-Y2O3@N-GDs inorganic-organic nanohybrid for boosted biomedical applications
S. Kumaraguru, L. Ragunath, J. Suresh, K. Gopinath
Inorganic Chemistry Communications.2025; 182: 115433. CrossRef - Thermal barrier coatings of YSZ developed by plasma sprayed technique and its effective use in orthopedic and dental application
Aishwariya Rajendiran, Vijayalakshmi Uthirapathy
Journal of Materials Science: Materials in Medicine.2025;[Epub] CrossRef - Extreme temperature gradient promoting oxygen diffusion in yttria‐stabilized zirconia: A molecular dynamics study
Jian Guo, Yan Yin, Min Yi
Journal of the American Ceramic Society.2024; 107(10): 6783. CrossRef - Bioceramics: a review on design concepts toward tailor-made (multi)-functional materials for tissue engineering applications
Ritesh Kumar, Ipsita Pattanayak, Pragyan Aparajita Dash, Smita Mohanty
Journal of Materials Science.2023; 58(8): 3460. CrossRef - In Vitro Degradation of Mg-Doped ZrO2 Bioceramics at the Interface with Xerostom® Saliva Substitute Gel
Liliana Bizo, Marieta Mureşan-Pop, Réka Barabás, Lucian Barbu-Tudoran, Antonela Berar
Materials.2023; 16(7): 2680. CrossRef - Processing of gelatine coated composite scaffolds based on magnesium and strontium doped hydroxyapatite and yttria-stabilized zirconium oxide
Aleksa Galic, Tamara Matic, Natasa Obradovic, Zvezdana Bascarevic, Djordje Veljovic
Science of Sintering.2023; 55(4): 469. CrossRef - Biocompatibility of ZrO2 vs. Y-TZP Alloys: Influence of Their Composition and Surface Topography
Alex Tchinda, Laëtitia Chézeau, Gaël Pierson, Richard Kouitat-Njiwa, B H Rihn, Pierre Bravetti
Materials.2022; 15(13): 4655. CrossRef - Influence of oxygen vacancy compensation on the structure, electronic and mechanical properties of yttrium stabilized tetragonal zirconia
Zhou Fan, Yang Wang, Yidong Zhang, Jianyi Liu
Materials Science in Semiconductor Processing.2021; 135: 106082. CrossRef
- Comparative Evaluation of the Effects of Yttrium Stabilized Zirconia Nanoparticles (YSZrO2- NP) and Porcelain Particles on Property Enhancement of Polymethylmethacrylate (PMMA) Denture Composites
- 1,914 View
- 20 Download
- 10 Crossref

- Comparison of bond strengths of ceramic brackets bonded to zirconia surfaces using different zirconia primers and a universal adhesive
- Ji-Yeon Lee, Jaechan Ahn, Sang In An, Jeong-won Park
- Restor Dent Endod 2018;43(1):e7. Published online January 22, 2018
- DOI: https://doi.org/10.5395/rde.2018.43.e7
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
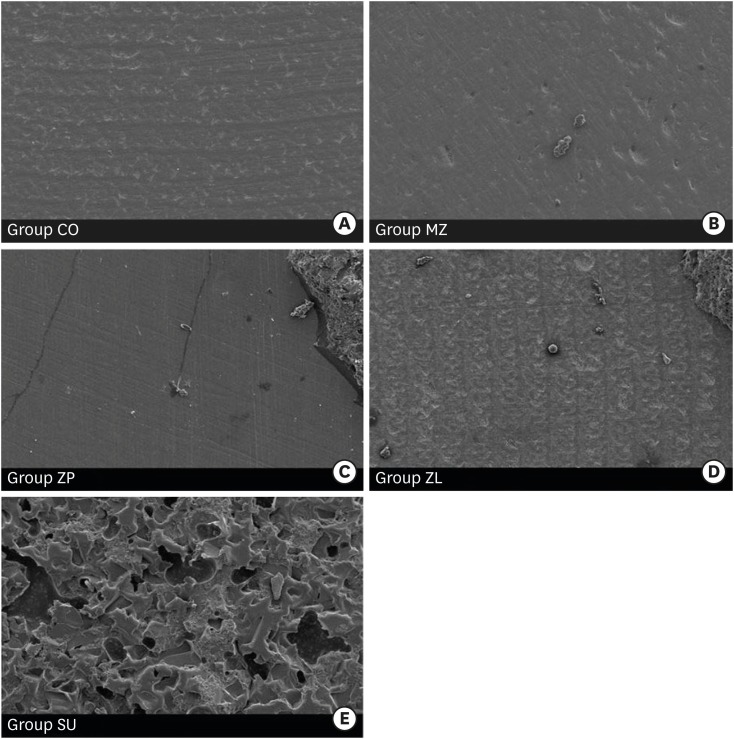
ePub Objectives The aim of this study is to compare the shear bond strengths of ceramic brackets bonded to zirconia surfaces using different zirconia primers and universal adhesive.
Materials and Methods Fifty zirconia blocks (15 × 15 × 10 mm, Zpex, Tosoh Corporation) were polished with 1,000 grit sand paper and air-abraded with 50 µm Al2O3 for 10 seconds (40 psi). They were divided into 5 groups: control (CO), Metal/Zirconia primer (MZ, Ivoclar Vivadent), Z-PRIME Plus (ZP, Bisco), Zirconia Liner (ZL, Sun Medical), and Scotchbond Universal adhesive (SU, 3M ESPE). Transbond XT Primer (used for CO, MZ, ZP, and ZL) and Transbond XT Paste was used for bracket bonding (Gemini clear ceramic brackets, 3M Unitek). After 24 hours at 37°C storage, specimens underwent 2,000 thermocycles, and then, shear bond strengths were measured (1 mm/min). An adhesive remnant index (ARI) score was calculated. The data were analyzed using one-way analysis of variance and the Bonferroni test (
p = 0.05).Results Surface treatment with primers resulted in increased shear bond strength. The SU group showed the highest shear bond strength followed by the ZP, ZL, MZ, and CO groups, in that order. The median ARI scores were as follows: CO = 0, MZ = 0, ZP = 0, ZL = 0, and SU = 3 (
p < 0.05).Conclusions Within this experiment, zirconia primer can increase the shear bond strength of bracket bonding. The highest shear bond strength is observed in SU group, even when no primer is used.
-
Citations
Citations to this article as recorded by- Effectiveness of universal adhesives for orthodontic bonding to enamel and restorative materials: A systematic review
Claire-Adeline Dantagnan, Maureen Boudrot, Julia Bosco, Gauthier Dot, Ali Nassif, Philippe François, Jean-Pierre Attal
International Orthodontics.2026; 24(2): 101089. CrossRef - State-of-the-Art Zirconia and Glass–Ceramic Materials in Restorative Dentistry: Properties, Clinical Applications, Challenges, and Future Perspectives
Sorin Gheorghe Mihali, Adela Hiller
Applied Sciences.2025; 15(23): 12841. CrossRef - Shear bond strength and ARI scores of metal brackets to glazed glass ceramics and zirconia: an in vitro study investigating surface treatment protocols
Claire Pédemay, Philippe François, Vincent Fouquet, Sarah Abdel-Gawad, Jean-Pierre Attal, Claire-Adeline Dantagnan
BMC Oral Health.2024;[Epub] CrossRef - Impact of different pretreatments and attachment materials on shear bond strength of indirectly bonded brackets using CAD/CAM transfer trays to monolithic zirconia
Rebecca Jungbauer, Christian M. Hammer, Daniel Edelhoff, Peter Proff, Bogna Stawarczyk
Dental Materials.2023; 39(2): 170. CrossRef - Mechanical and chemical surface treatment enhances bond strength between zirconia and orthodontic brackets: an in vitro study
Nareudee Limpuangthip, Atikom Surintanasarn, Ploylada Vitavaspan
BDJ Open.2023;[Epub] CrossRef - Effect of Different Surface Treatments and Orthodontic Bracket Type on Shear Bond Strength of High‐Translucent Zirconia: An In Vitro Study
Yasamin Babaee Hemmati, Hamid Neshandar Asli, Mehran Falahchai, Sina Safary, Sandrine Bittencourt Berger
International Journal of Dentistry.2022;[Epub] CrossRef - Does Surface Treatment With Different Primers Increase The Shear Bond Strength Between Metallic Bracket and Monolithic Zirconia?
Emine Begüm BÜYÜKERKMEN, Ayşe Selenge AKBULUT, Murat KEÇECİ
Selcuk Dental Journal.2022; 9(2): 451. CrossRef - Effect of Different Surface Treatments on the Surface Roughness and Orthodontic Bond Strength of Partially-stabilized Zirconia
Mustafa Borga Dönmez, Betül Ballı Demirel, Münir Demirel, Yasemin Gündoğdu, Hamdi Şükür Kılıç
Meandros Medical and Dental Journal.2022; 23(3): 335. CrossRef - Shear Bond Strength of Polypropylene Fiber in Orthodontic Adhesive on Glazed Monolithic Zirconia
Dhanabhol Riowruangsanggoon, Apiwat Riddhabhaya, Nattisa Niyomtham, Irin Sirisoontorn
Polymers.2022; 14(21): 4627. CrossRef - Effects of Three Novel Bracket Luting Agents Containing Zirconia Primer on Shear Bond Strength of Metal Orthodontic Brackets Attached to Monolithic Zirconia Crowns: A Preliminary In Vitro Study
Milad Shamohammadi Heidari, Mehrnaz Moradinejad, Hamed Tabatabaei, Vahid Rakhshan, Dinesh Rokaya
International Journal of Dentistry.2022;[Epub] CrossRef - Impact of different pretreatments and attachment materials on shear bond strength between monolithic zirconia restorations and metal brackets
Rebecca Jungbauer, Peter Proff, Daniel Edelhoff, Bogna Stawarczyk
Scientific Reports.2022;[Epub] CrossRef - Bracket Bonding to All-Ceramic Materials with Universal Adhesives
Cecilia Goracci, Giuseppe Di Bello, Lorenzo Franchi, Chris Louca, Jelena Juloski, Jovana Juloski, Alessandro Vichi
Materials.2022; 15(3): 1245. CrossRef - Effect of enamel-surface modifications on shear bond strength using different adhesive materials
Bo-wen Zheng, Shan Cao, Majedh Abdo Ali Al-Somairi, Jia He, Yi Liu
BMC Oral Health.2022;[Epub] CrossRef - The effect of various mechanical and chemical surface conditioning on the bonding of orthodontic brackets to all ceramic materials
Dalia A. Abuelenain, Amal I. Linjawi, Ahmed S. Alghamdi, Fahad M. Alsadi
Journal of Dental Sciences.2021; 16(1): 370. CrossRef - The Performance of Universal Adhesives on Orthodontic Bracket Bonding
Muhittin Ugurlu, Muhammed Hilmi Buyukcavus
European Journal of General Dentistry.2021; 10(01): 019. CrossRef - A comparison of shear bond strength of brackets bonded to zirconia
Hannah Knott, Xiaoming Xu, Edwin Kee, Qingzhao Yu, Paul Armbruster, Richard Ballard
Australasian Orthodontic Journal.2021; 37(1): 62. CrossRef - Influence of Surface Treatment and Resin Cements on the Bond Strength between the Y-TZP Zirconia and Composite Resin Interface
Lucas Campagnaro Maciel, Amanda Pádua Proeza, Hélyda Coelho Guimarães Balbino, Marcela Moráo Corteletti, Ricardo Huver De Jesus, Laís Regiane da Silva Concílio
Journal of Health Sciences.2019; 21(5): 477. CrossRef - Effect of Simplified Bonding on Shear Bond Strength between Ceramic Brackets and Dental Zirconia
Ga-Youn Ju, Soram Oh, Bum-Soon Lim, Hyun-Seung Lee, Shin Hye Chung
Materials.2019; 12(10): 1640. CrossRef
- Effectiveness of universal adhesives for orthodontic bonding to enamel and restorative materials: A systematic review
- 2,280 View
- 16 Download
- 18 Crossref

- Cytotoxicity and biocompatibility of Zirconia (Y-TZP) posts with various dental cements
- Hyeongsoon Shin, Hyunjung Ko, Miri Kim
- Restor Dent Endod 2016;41(3):167-175. Published online May 30, 2016
- DOI: https://doi.org/10.5395/rde.2016.41.3.167
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives Endodontically treated teeth with insufficient tooth structure are often restored with esthetic restorations. This study evaluated the cytotoxicity and biological effects of yttria partially stabilized zirconia (Y-TZP) blocks in combination with several dental cements.
Materials and Methods Pairs of zirconia cylinders with medium alone or cemented with three types of dental cement including RelyX U200 (3M ESPE), FujiCEM 2 (GC), and Panavia F 2.0 (Kuraray) were incubated in medium for 14 days. The cytotoxicity of each supernatant was determined using 3-(4,5-dimethylthiazole-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assays on L929 fibroblasts and MC3T3-E1 osteoblasts. The levels of interleukin-6 (IL-6) mRNA were evaluated by reverse transcription polymerase chain reaction (RT-PCR), and IL-6 protein was evaluated by enzyme-linked immunosorbent assays (ELISA). The data were analyzed using one-way ANOVA and Tukey
post-hoc tests. Ap < 0.05 was considered statistically significant.Results The MTT assays showed that MC3T3-E1 osteoblasts were more susceptible to dental cements than L929 fibroblasts. The resin based dental cements increased IL-6 expression in L929 cells, but reduced IL-6 expression in MC3T3-E1 cells.
Conclusions Zirconia alone or blocks cemented with dental cement showed acceptable biocompatibilities. The results showed resin-modified glass-ionomer based cement less produced inflammatory cytokines than other self-adhesive resin-based cements. Furthermore, osteoblasts were more susceptible than fibroblasts to the biological effects of dental cement.
-
Citations
Citations to this article as recorded by- Digital light processing 3D printing of yttria stabilized zirconia ceramics: microstructures, characterizations, and cytocompatibility
Luke Wadle, Mena Asha Krishnan, Ryan Wall, Lanh Trinh, Bin Duan, Bai Cui
Emergent Materials.2025; 8(2): 1023. CrossRef - Doping of casted silk fibroin membranes with extracellular vesicles for regenerative therapy: a proof of concept
Sandra Fuest, Amanda Salviano-Silva, Cecile L. Maire, Yong Xu, Christian Apel, Audrey Laure Céline Grust, Arianna Delle Coste, Martin Gosau, Franz L. Ricklefs, Ralf Smeets
Scientific Reports.2024;[Epub] CrossRef - 3D printing of ceramics: Advantages, challenges, applications, and perspectives
Susmita Bose, Enver Koray Akdogan, Vamsi K. Balla, Sushant Ciliveri, Paolo Colombo, Giorgia Franchin, Nicholas Ku, Priya Kushram, Fangyong Niu, Joshua Pelz, Andrew Rosenberger, Ahmad Safari, Zachary Seeley, Rodney W. Trice, Lionel Vargas‐Gonzalez, Jeffrey
Journal of the American Ceramic Society.2024; 107(12): 7879. CrossRef - A Review on Biocompatibility of Dental Restorative and Reconstruction Materials
Pune Nina Paqué, Mutlu Özcan
Current Oral Health Reports.2024; 11(1): 68. CrossRef - Enhancement of Human Gingival Fibroblasts Bioactivity and Proliferation on Plasma Sprayed Yttria-Stabilised Zirconia/TiO2 Surface Coating of Titanium Alloys: An In-Vitro Study
Afida Jemat, Masfueh Razali, Yuichi Otsuka, Mariyam Jameelah Ghazali
Coatings.2023; 13(10): 1746. CrossRef - Material extrusion-based additive manufacturing of zirconia toughened alumina: Machinability, mechanical properties and biocompatibility
Tianyu Yu, Xiaolong Zhu, Hongwei Yu, Pan Wu, Chun Li, Xiaoxiao Han, Mingjun Chen
Journal of Manufacturing Processes.2023; 94: 120. CrossRef - Green synthesis and characterization of zirconium nanoparticlefor dental implant applications
Mohammad Asaduzzaman Chowdhury, Nayem Hossain, Md. Golam Mostofa, Md. Riyad Mia, Md. Tushar, Md. Masud Rana, Md. Helal Hossain
Heliyon.2023; 9(1): e12711. CrossRef - The role of Y2O3 in the bioactivity of YSZ/PLLA composites
Elia Marin, Giada Bassi, Orion Yoshikawa, Francesco Boschetto, Wenliang Zhu, Arianna Rossi, Alex Lanzutti, Huaizhong Xu, Monica Montesi, Silvia Panseri, Giuseppe Pezzotti
Journal of Materials Science.2023; 58(27): 11218. CrossRef - Nano-β-tricalcium phosphate incorporated root dentin adhesive in the bonding interface of yttria-stabilized tetragonal zirconia polycrystalline post
Amal S. Al-Qahtani, Huda I. Tulbah, Mashael Binhasan, Mai M. Alhamdan, Imran Farooq, Fahim Vohra, Tariq Abduljabbar
Applied Nanoscience.2022; 12(11): 3489. CrossRef - Outcome of teeth restored with CAD/CAM zirconium dioxide post-cores: a retrospective study with a follow-up period of 3–6 years
Shunv Ying, Song Chen, Siyuan Wang, Lingli Xu, Xiaofeng Wang, Fuming He, Wei Liu
BMC Oral Health.2022;[Epub] CrossRef - Review of Physical, Mechanical, and Biological Characteristics of 3D-Printed Bioceramic Scaffolds for Bone Tissue Engineering Applications
Mahendran Thangavel, Renold Elsen Selvam
ACS Biomaterials Science & Engineering.2022; 8(12): 5060. CrossRef - Comparison of Regular and Speed Sintering on Low-Temperature Degradation and Fatigue Resistance of Translucent Zirconia Crowns for Implants: An In Vitro Study
Suchada Kongkiatkamon, Chaimongkon Peampring
Journal of Functional Biomaterials.2022; 13(4): 281. CrossRef - Cytotoxicity and Bonding Property of Bioinspired Nacre-like Ceramic-Polymer Composites
Hui Sun, Kefeng Gao, Zhe Yi, Chengwei Han, Zengqian Liu, Qiang Wang, Qing Zhou, Zhefeng Zhang
Frontiers in Bioengineering and Biotechnology.2022;[Epub] CrossRef - Characterisation of Selected Materials in Medical Applications
Kacper Kroczek, Paweł Turek, Damian Mazur, Jacek Szczygielski, Damian Filip, Robert Brodowski, Krzysztof Balawender, Łukasz Przeszłowski, Bogumił Lewandowski, Stanisław Orkisz, Artur Mazur, Grzegorz Budzik, Józef Cebulski, Mariusz Oleksy
Polymers.2022; 14(8): 1526. CrossRef - Adhesive bond integrity of Y‐TZP post with calcium fluoride infiltrated resin dentin adhesive: An SEM, EDX, FTIR and micro‐Raman study
Eman M. AlHamdan, Samar Al‐Saleh, Mohammad H. AlRefeai, Imran Farooq, Eisha Abrar, Fahim Vohra, Tariq Abduljabbar
Surface and Interface Analysis.2021; 53(11): 956. CrossRef - Additive Manufacturing (3D PRINTING) Methods and Applications in Dentistry
Elif DEMİRALP, Gülsüm DOĞRU, Handan YILMAZ
Clinical and Experimental Health Sciences.2021; 11(1): 182. CrossRef - Interleukin-1β activity in gingival crevicular fluid of abutment teeth with temporary fixed restorations versus final fixed restorations: Prospective observational study
Amal Abdallah A. Abo-Elmagd, Dina Sabry, Ebtehal Mohammed
The Saudi Dental Journal.2021; 33(6): 322. CrossRef - Change in the Microhardness of Composite Ceramics at the CaO–ZrO2/CaO–ZrO2 + Al2O3 Interface
A. A. Dmitrievskiy, D. G. Zhigacheva, G. V. Grigoriev, P. N. Ovchinnikov
Journal of Surface Investigation: X-ray, Synchrotron and Neutron Techniques.2021; 15(S1): S137. CrossRef - Cytotoxicity of two self-adhesive flowable composites on bovine dental pulp-derived cells
Firdevs KAHVECİOĞLU, Türkay KÖLÜŞ, Fatma SAĞ GÜNGÖR, Hayriye Esra ÜLKER
Journal of Health Sciences and Medicine.2021; 4(2): 209. CrossRef - Cytotoxicity and biocompatibility of high mol% yttria containing zirconia
Gulsan Ara Sathi Kazi, Ryo Yamagiwa
Restorative Dentistry & Endodontics.2020;[Epub] CrossRef - Cytotoxic effects of different self-adhesive resin cements: Cell viability and induction of apoptosis
Soner Şişmanoğlu, Mustafa Demirci, Helmut Schweikl, Gunes Ozen-Eroglu, Esin Cetin-Aktas, Serap Kuruca, Safa Tuncer, Neslihan Tekce
The Journal of Advanced Prosthodontics.2020; 12(2): 89. CrossRef - Effects of nano-zirconia fillers conditioned with phosphate ester monomers on the conversion and mechanical properties of Bis-GMA- and UDMA-based resin composites
Jiaxue Yang, Jiadi Shen, Xinyi Wu, Feng He, Haifeng Xie, Chen Chen
Journal of Dentistry.2020; 94: 103306. CrossRef - Effect of APTES- or MPTS-Conditioned Nanozirconia Fillers on Mechanical Properties of Bis-GMA-Based Resin Composites
Jiaxue Yang, Mengyuan Liao, Gaoying Hong, Shiqi Dai, Jiadi Shen, Haifeng Xie, Chen Chen
ACS Omega.2020; 5(50): 32540. CrossRef - In Vitro Cytotoxicity of Self-Adhesive Dual-Cured Resin Cement Polymerized Beneath Three Different Cusp Inclinations of Zirconia
Chang-Yuan Zhang, Yi-Ling Cheng, Xin-Wen Tong, Hao Yu, Hui Cheng
BioMed Research International.2019; 2019: 1. CrossRef - Investigations on the corrosion behaviour and biocompatibility of magnesium alloy surface composites AZ91D-ZrO2 fabricated by friction stir processing
R. Vaira Vignesh, R. Padmanaban, M. Govindaraju, G. Suganya Priyadharshini
Transactions of the IMF.2019; 97(5): 261. CrossRef - Microwave assisted synthesis and antimicrobial activity of Fe3O4-doped ZrO2 nanoparticles
M. Imran, Saira Riaz, Ifra Sanaullah, Usman Khan, Anjum N. Sabri, Shahzad Naseem
Ceramics International.2019; 45(8): 10106. CrossRef - Additive manufacturing of ceramics for dental applications: A review
Raquel Galante, Celio G. Figueiredo-Pina, Ana Paula Serro
Dental Materials.2019; 35(6): 825. CrossRef - Reinforcement of dental resin composite via zirconium hydroxide coating and phosphate ester monomer conditioning of nano-zirconia fillers
Xinyi Wu, Shiqi Dai, Ying Chen, Feng He, Haifeng Xie, Chen Chen
Journal of the Mechanical Behavior of Biomedical Materials.2019; 94: 32. CrossRef - Effects of TiO2 on microstructural, mechanical properties and in-vitro bioactivity of plasma sprayed yttria stabilised zirconia coatings for dental application
A. Jemat, M.J. Ghazali, M. Razali, Y. Otsuka, A. Rajabi
Ceramics International.2018; 44(4): 4271. CrossRef - In vitro evaluation of cytotoxicity of different self-adhesive resin cements
Necla Demir, Firdevs Kahvecioğlu, Muhammet Karcı, Hayriye Esra Ülker, Nuray Günaydın
Acta Odontologica Turcica.2017;[Epub] CrossRef
- Digital light processing 3D printing of yttria stabilized zirconia ceramics: microstructures, characterizations, and cytocompatibility
- 2,300 View
- 17 Download
- 30 Crossref

- Orthodontic bracket bonding to glazed full-contour zirconia
- Ji-Young Kwak, Hyo-Kyung Jung, Il-Kyung Choi, Tae-Yub Kwon
- Restor Dent Endod 2016;41(2):106-113. Published online April 14, 2016
- DOI: https://doi.org/10.5395/rde.2016.41.2.106
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives This study evaluated the effects of different surface conditioning methods on the bond strength of orthodontic brackets to glazed full-zirconia surfaces.
Materials and Methods Glazed zirconia (except for the control, Zirkonzahn Prettau) disc surfaces were pre-treated: PO (control), polishing; BR, bur roughening; PP, cleaning with a prophy cup and pumice; HF, hydrofluoric acid etching; AA, air abrasion with aluminum oxide; CJ, CoJet-Sand. The surfaces were examined using profilometry, scanning electron microscopy, and electron dispersive spectroscopy. A zirconia primer (Z-Prime Plus, Z) or a silane primer (Monobond-S, S) was then applied to the surfaces, yielding 7 groups (PO-Z, BR-Z, PP-S, HF-S, AA-S, AA-Z, and CJ-S). Metal bracket-bonded specimens were stored in water for 24 hr at 37℃, and thermocycled for 1,000 cycles. Their bond strengths were measured using the wire loop method (
n = 10).Results Except for BR, the surface pre-treatments failed to expose the zirconia substructure. A significant difference in bond strengths was found between AA-Z (4.60 ± 1.08 MPa) and all other groups (13.38 ± 2.57 - 15.78 ± 2.39 MPa,
p < 0.05). For AA-Z, most of the adhesive remained on the bracket.Conclusions For bracket bonding to glazed zirconia, a simple application of silane to the cleaned surface is recommended. A zirconia primer should be used only when the zirconia substructure is definitely exposed.
-
Citations
Citations to this article as recorded by- Evaluation of Different Surface Roughening Techniques on Clear Aligner Attachments Bonded to Monolithic Zirconia: In Vitro Study
Nehal F Albelasy, Ahmad M Hafez, Abdullah S Alhunayni
The Journal of Contemporary Dental Practice.2025; 25(12): 1104. CrossRef - An Innovative Method of Permanent Retention on Veneered Crowns
Yugandhar Garlapati, Sampath Krishna Veni, Jashva Vamsi Kogila, Polisetty Siva Krishna, K. N. Anand Kumar
Journal of Indian Orthodontic Society.2025; 59(3): 279. CrossRef - Effect of Different Primers on the Shear Bond Strength of Orthodontic Brackets Bonded to Reinforced Polyetheretherketone (PEEK) Substrate
Ahmed Akram EL-Awady, Khaled Samy ElHabbak, Hussein Ramadan Mohamed, Ahmed Elsayed Elwan, Karim Sherif Adly, Moamen Ahmed Abdalla, Ehab Mohamed Kamal, Ahmed Leithy Alameldin
Dentistry Journal.2024; 12(6): 188. CrossRef - The Effect of Various Lasers on the Bond Strength Between Orthodontic Brackets and Dental Ceramics: A Systematic Review and Meta-Analysis
Seyed Ali Mosaddad, Jaafar Abduo, Mehrnaz Zakizade, Hamid Tebyaniyan, Ahmed Hussain
Photobiomodulation, Photomedicine, and Laser Surgery.2024; 42(1): 20. CrossRef - Shear Bond Strength of Clear Aligner Attachment Using 4-META/MMA-TBB Resin Cement on Glazed Monolithic Zirconia
Kasidit Nitasnoraset, Apiwat Riddhabhaya, Chidchanok Sessirisombat, Hitoshi Hotokezaka, Noriaki Yoshida, Irin Sirisoontorn
Polymers.2024; 16(14): 1988. CrossRef - Orthodontic bonding in special circumstances
Angus Burns, Annie Hughes, Michael O’Sullivan
British Dental Journal.2024; 237(5): 400. CrossRef - Bonding Effectiveness of Saliva-Contaminated Monolithic Zirconia Ceramics Using Different Decontamination Protocols
Necla Demir, Ozge Genc, Ipek Balevi Akkese, Meral Arslan Malkoc, Mutlu Ozcan, Konstantinos Michalakis
BioMed Research International.2024; 2024: 1. CrossRef - Comparison of shear bond strength of metallic orthodontic brackets bonded to zirconia models underwent different surface conditioning methods and different primer systems
Amena Raafat Khaled, Enas Talb Al-Jwary
APOS Trends in Orthodontics.2024; 15: 251. CrossRef - Shear bond strength and ARI scores of metal brackets to glazed glass ceramics and zirconia: an in vitro study investigating surface treatment protocols
Claire Pédemay, Philippe François, Vincent Fouquet, Sarah Abdel-Gawad, Jean-Pierre Attal, Claire-Adeline Dantagnan
BMC Oral Health.2024;[Epub] CrossRef - Enhanced Bracket Retention on Reinforced Polyetheretherketone: Role of Specialized Primers in Shear Bond Strength
Mehmet Yılmaz, Ayşe Demir
International Journal of Dental Research and Allied Sciences.2024; 4(2): 64. CrossRef - Mechanical and chemical surface treatment enhances bond strength between zirconia and orthodontic brackets: an in vitro study
Nareudee Limpuangthip, Atikom Surintanasarn, Ploylada Vitavaspan
BDJ Open.2023;[Epub] CrossRef - Shear bond strength of orthodontic brackets bonded to a new version of zirconium all ceramic restoration: An in vitro comparative study
Assem Abd EL-wahab, Marwa Shamaa, Ahmed Hafez, Noha El-Wassefy, Shaza Hammad
Heliyon.2023; 9(5): e16249. CrossRef - Evaluation of the effects of different composite materials and surface roughening techniques in bonding attachments of clear aligner on monolithic zirconia
Semiha Arslan, Hamiyet Kilinc
Orthodontics & Craniofacial Research.2023; 26(4): 546. CrossRef - Effect of Different Types of Adhesive Agents on Orthodontic Bracket Shear Bond Strength: A Cyclic Loading Study
Irfan Eser, Orhan Cicek, Nurhat Ozkalayci, Mehmet Yetmez, Hande Erener
Materials.2023; 16(2): 724. CrossRef - Bracket Bonding to All-Ceramic Materials with Universal Adhesives
Cecilia Goracci, Giuseppe Di Bello, Lorenzo Franchi, Chris Louca, Jelena Juloski, Jovana Juloski, Alessandro Vichi
Materials.2022; 15(3): 1245. CrossRef - Effects of Three Novel Bracket Luting Agents Containing Zirconia Primer on Shear Bond Strength of Metal Orthodontic Brackets Attached to Monolithic Zirconia Crowns: A Preliminary In Vitro Study
Milad Shamohammadi Heidari, Mehrnaz Moradinejad, Hamed Tabatabaei, Vahid Rakhshan, Dinesh Rokaya
International Journal of Dentistry.2022;[Epub] CrossRef - Does Surface Treatment With Different Primers Increase The Shear Bond Strength Between Metallic Bracket and Monolithic Zirconia?
Emine Begüm BÜYÜKERKMEN, Ayşe Selenge AKBULUT, Murat KEÇECİ
Selcuk Dental Journal.2022; 9(2): 451. CrossRef - Effect of different primer agents on shear bond strength of ceramic orthodontic brackets bonded to zirconia ceramics
Ebru Kucukkaraca, Canan Akay
Journal of the Australian Ceramic Society.2022; 58(2): 645. CrossRef - Shear Bond Strength of Polypropylene Fiber in Orthodontic Adhesive on Glazed Monolithic Zirconia
Dhanabhol Riowruangsanggoon, Apiwat Riddhabhaya, Nattisa Niyomtham, Irin Sirisoontorn
Polymers.2022; 14(21): 4627. CrossRef - Bond Integrity and Surface Topography of Orthodontic Metal Brackets to Ceramic and Polymer-Based Restorations. An In-Vitro Study Design
Ali Alqerban
Science of Advanced Materials.2021; 13(4): 650. CrossRef - The effect of surface treatment and thermocycling on the shear bond strength of orthodontic brackets to the Y-TZP zirconia ceramics: A systematic review
Tamzid AHMED, Nashid FAREEN, Mohammad Khursheed ALAM
Dental Press Journal of Orthodontics.2021;[Epub] CrossRef - Orthodontic Bonding: Review of the Literature
Ali H. Alzainal, Ahmed Shehab Majud, Abdulfatah M. Al-Ani, Adil O. Mageet
International Journal of Dentistry.2020; 2020: 1. CrossRef - Shear bond strength between orthodontic metal brackets and Y-TZP according to the various ceramic surface treatments before and after thermocycling
Ji-Bong Choi, Seon-Mi Byeon
Korean Journal of Dental Materials.2020; 47(2): 83. CrossRef - Bond Strength and Failure Pattern of Orthodontic Tubes Adhered to a Zirconia Surface Submitted to Different Modes of Application of a Ceramic Primer
Francisco da Silva Araújo Milagres, Dauro Douglas Oliveira, Giordani Santos Silveira, Emanuelle de Fátima Ferreira Oliveira, Alberto Nogueira da Gama Antunes
Materials.2019; 12(23): 3922. CrossRef - Shear bond strength of orthodontic brackets bonded to a new all-ceramic crown composed of lithium silicate infused with zirconia: An in vitro comparative study
Ryan Gardiner, Richard Ballard, Qingzhao Yu, Edwin Kee, Xiaoming Xu, Paul Armbruster
International Orthodontics.2019; 17(4): 726. CrossRef - Comparison of bond strengths of ceramic brackets bonded to zirconia surfaces using different zirconia primers and a universal adhesive
Ji-Yeon Lee, Jaechan Ahn, Sang In An, Jeong-won Park
Restorative Dentistry & Endodontics.2018;[Epub] CrossRef
- Evaluation of Different Surface Roughening Techniques on Clear Aligner Attachments Bonded to Monolithic Zirconia: In Vitro Study
- 2,034 View
- 12 Download
- 26 Crossref

- Finite element analysis of maxillary central incisors restored with various post-and-core applications
- MinSeock Seo, WonJun Shon, WooCheol Lee, Hyun-Mi Yoo, Byeong-Hoon Cho, Seung-Ho Baek
- J Korean Acad Conserv Dent 2009;34(4):324-332. Published online July 31, 2009
- DOI: https://doi.org/10.5395/JKACD.2009.34.4.324
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub The purpose of this study was to investigate the effect of rigidity of post core systems on stress distribution by the theoretical technique, finite element stress-analysis method. Three-dimensional finite element models simulating an endodontically treated maxillary central incisor restored with a zirconia ceramic crown were prepared and 1.5 mm ferrule height was provided. Each model contained cortical bone, trabecular bone, periodontal ligament, 4 mm apical root canal filling, and post-and-core. Six combinations of three parallel type post (zirconia ceramic, glass fiber, and stainless steel) and two core (Paracore and Tetric ceram) materials were evaluated, respectively. A 50 N static occlusal load was applied to the palatal surface of the crown with a 60° angle to the long axis of the tooth. The differences in stress transfer characteristics of the models were analyzed. von Mises stresses were chosen for presentation of results and maximum displacement and hydrostatic pressure were also calculated. An increase of the elastic modulus of the post material increased the stress, but shifted the maximum stress location from the dentin surface to the post material. Buccal side of cervical region (junction of core and crown) of the glass fiber post restored tooth was subjected to the highest stress concentration. Maximum von Mises stress in the remaining radicular tooth structure for low elastic modulus resin core (29.21 MPa) was slightly higher than that for high elastic modulus resin core (29.14 MPa) in case of glass fiber post. Maximum displacement of glass fiber post restored tooth was higher than that of zirconia ceramic or stainless steel post restored tooth.
-
Citations
Citations to this article as recorded by- Evaluation of stress distribution on an endodontically treated maxillary central tooth with lesion restored with different crown materials: A finite element analysis
Ömer Kirmali, Gülsah Icen, H. Kursat Celik, Allan E.W. Rennie
Heliyon.2024; 10(3): e25829. CrossRef - The mechanical and physical properties of microcrystalline cellulose (MCC)/sisal/PMMA hybrid composites for dental applications
Harini Sosiati, Arif Muhammad Rizky, Aldi Lukman Maulana Latief, Rahmad Kuncoro Adi, Sinin Hamdan
Materials Research Express.2023; 10(3): 035301. CrossRef - Influence of post types and sizes on fracture resistance in the immature tooth model
Jong-Hyun Kim, Sung-Ho Park, Jeong-Won Park, Il-Young Jung
Journal of Korean Academy of Conservative Dentistry.2010; 35(4): 257. CrossRef
- Evaluation of stress distribution on an endodontically treated maxillary central tooth with lesion restored with different crown materials: A finite element analysis
- 1,447 View
- 6 Download
- 3 Crossref


 KACD
KACD

 First
First Prev
Prev


