Search
- Page Path
- HOME > Search
- The application of “bone window technique” using piezoelectric saws and a CAD/CAM-guided surgical stent in endodontic microsurgery on a mandibular molar case
- Ukseong Kim, Sunil Kim, Euiseong Kim
- Restor Dent Endod 2020;45(3):e27. Published online May 21, 2020
- DOI: https://doi.org/10.5395/rde.2020.45.e27
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
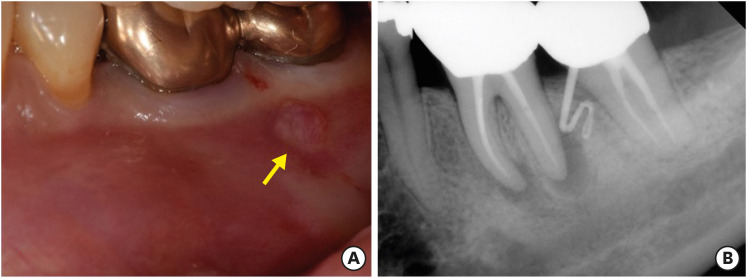
ePub Apical surgery for a mandibular molar is still challenging for many reasons. This report describes the applications of computer-guided cortical ‘bone-window technique’ using piezoelectric saws that prevented any nerve damage in performing endodontic microsurgery of a mandibular molar. A 49-year-old woman presented with gumboil on tooth #36 (previously endodontically treated tooth) and was diagnosed with chronic apical abscess. Periapical lesions were confirmed using cone-beam computed tomography (CBCT). Endodontic microsurgery for the mesial and distal roots of tooth #36 was planned. Following the transfer of data of the CBCT images and the scanned cast to an implant surgical planning program, data from both devices were merged. A surgical stent was designed, on the superimposed three-dimensional model, to guide the preparation of a cortical window on the buccal side of tooth #36. Endodontic microsurgery was performed with a printed surgical template. Minimal osteotomy was required and preservation of the buccal cortical plate rendered this endodontic surgery less traumatic. No postoperative complications such as mental nerve damage were reported. Window technique guided by a computer-aided design/computer-aided manufacture based surgical template can be considerably useful in endodontic microsurgery in complicated cases.
-
Citations
Citations to this article as recorded by- Optimising Outcomes in Endodontic Microsurgery: Evidence, Uncertainties and Future Directions
Ukseong Kim, Euiseong Kim
International Endodontic Journal.2026;[Epub] CrossRef - Accuracy of Guided Dual Technique in Esthetic Crown Lengthening: A Prospective Case‐Series Study
Meritxell Enfedaque‐Prat, Albert González‐Barnadas, Adrià Jorba‐García, Javi Vilarrasa, Jorge Toledano‐Serrabona, Rui Figueiredo, Eduard Valmaseda‐Castellón, Octavi Camps‐Font
Journal of Esthetic and Restorative Dentistry.2025; 37(6): 1284. CrossRef - Guided endodontics in the application of personalized mini-invasive treatment in clinical cases: a literature review
Shuangshuang Ren, Wanping Wang, Mingyue Cheng, Wenyue Tang, Yue Zhao, Leiying Miao
The Saudi Dental Journal.2025;[Epub] CrossRef - Accurately Defining the Location and Dimension of the Bony Lid Under the Guidance of Dynamic Navigation: Report on Three Cases
Kailiang Tang, Xiaole Zhang, Qibao Wang, Xinyu Zhao, Xijiao Yu, Yi Du
Australian Endodontic Journal.2025; 51(3): 785. CrossRef - Minimally Invasive Vertical Incision Subperiosteal Tunnelling Technique for Targeted Endodontic Surgery: Technical Overview and a Case Report
Francesc Abella Sans, Jaime Barragán Montes, Tomasz Zbozen, Nandini Suresh, Lalli Dharmarajan, Paul M. H. Dummer, Venkateshbabu Nagendrababu
International Endodontic Journal.2025; 58(11): 1799. CrossRef - Endodontic Microsurgery of Mandibular Molars with an Autonomous Robotic System
Haiying Zhang, Zi Yang, Mangnan Liu, Yaoxin Wang, Mei Fu, Benxiang Hou, Chen Zhang
Journal of Endodontics.2025; 51(12): 1830. CrossRef - Endodontic Microsurgery of a Mandibular Molar Using a Dynamic Navigation System (DNS) and Cortical Window Technique: A Case Report
Gustavo Castillo, Silvia Restrepo-Méndez, Oscar Zuluaga, Paola Escobar-Villegas
Journal of Endodontic Microsurgery.2024; 3: 1. CrossRef - The bone lid technique in endodontic microsurgery
Min Zhang, He Liu, Ya Shen
Asian Journal of Surgery.2024; 47(7): 3126. CrossRef - Guided Periradicular Surgery with Er,Cr:YSGG Laser Osteotomy: A Case Report
Julian Torres Celeita, Johanna Hernández la Rotta, Amdie Chirinos Salazar, Jorge Fandiño Rodríguez, Laura López Rincón, Mauren Orduz Solorzano, Diana Parra Galvis, Oscar Jiménez Peña
Journal of Endodontic Microsurgery.2024;[Epub] CrossRef - Piezoelectric Endodontic Microsurgery with Modified Cortical Window Technique: A Case Report
Rafael Fernández-Grisales, Wilder Rojas, Carolina Berruecos-Orozco
Journal of Endodontic Microsurgery.2023; 2: 34. CrossRef - The Impact of the Preferred Reporting Items for Case Reports in Endodontics (PRICE) 2020 Guidelines on the Reporting of Endodontic Case Reports
Sofian Youssef, Phillip Tomson, Amir Reza Akbari, Natalie Archer, Fayjel Shah, Jasmeet Heran, Sunmeet Kandhari, Sandeep Pai, Shivakar Mehrotra, Joanna M Batt
Cureus.2023;[Epub] CrossRef - Clinical and radiological outcomes of dynamic navigation in endodontic microsurgery: a prospective study
Chen Chen, Rui Zhang, Wei Zhang, Fangzhe Li, Zan Wang, Li Qin, Yun Chen, Zhuan Bian, Liuyan Meng
Clinical Oral Investigations.2023; 27(9): 5317. CrossRef - New-designed 3D printed surgical guide promotes the accuracy of endodontic microsurgery: a study of 14 upper anterior teeth
Dan Zhao, Weige Xie, Tianguo Li, Anqi Wang, Li Wu, Wen Kang, Lu Wang, Shiliang Guo, Xuna Tang, Sijing Xie
Scientific Reports.2023;[Epub] CrossRef - Failure case analysis during each stage of endodontic microsurgery: A retrospective study based on clinical databases
Changwoo Ryu, Sooil Shin, Yong-Bum Cho, Euiseong Kim, Minju Song
Saudi Endodontic Journal.2023; 13(2): 160. CrossRef - Piezoelectric Device and Dynamic Navigation System Integration for Bone Window-Guided Surgery
Frederico C. Martinho, Ina L. Griffin, Patricia A. Tordik
Journal of Endodontics.2023; 49(12): 1698. CrossRef - Bone Window Technique in Endodontic Microsurgery – Report of Two Cases
Spyros Floratos, Vasileios Molonis, Apostolos Tsolakis, Stylianos Kykalos, Konstantinos Kontzoglou
Journal of Endodontic Microsurgery.2022; 2: 24. CrossRef - An Update on Endodontic Microsurgery of Mandibular Molars: A Focused Review
Sun Mi Jang, Euiseong Kim, Kyung-San Min
Medicina.2021; 57(3): 270. CrossRef
- Optimising Outcomes in Endodontic Microsurgery: Evidence, Uncertainties and Future Directions
- 1,959 View
- 37 Download
- 17 Crossref

- Apicoectomy of maxillary anterior teeth through a piezoelectric bony-window osteotomy: two case reports introducing a new technique to preserve cortical bone
- Viola Hirsch, Meetu R. Kohli, Syngcuk Kim
- Restor Dent Endod 2016;41(4):310-315. Published online July 5, 2016
- DOI: https://doi.org/10.5395/rde.2016.41.4.310
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Two case reports describing a new technique of creating a repositionable piezoelectric bony window osteotomy during apicoectomy in order to preserve bone and act as an autologous graft for the surgical site are described. Endodontic microsurgery of anterior teeth with an intact cortical plate and large periapical lesion generally involves removal of a significant amount of healthy bone in order to enucleate the diseased tissue and manage root ends. In the reported cases, apicoectomy was performed on the lateral incisors of two patients. A piezoelectric device was used to create and elevate a bony window at the surgical site, instead of drilling and destroying bone while making an osteotomy with conventional burs. Routine microsurgical procedures - lesion enucleation, root-end resection, and filling - were carried out through this window preparation. The bony window was repositioned to the original site and the soft tissue sutured. The cases were re-evaluated clinically and radiographically after a period of 12 - 24 months. At follow-up, radiographic healing was observed. No additional grafting material was needed despite the extent of the lesions. The indication for this procedure is when teeth present with an intact or near-intact buccal cortical plate and a large apical lesion to preserve the bone and use it as an autologous graft.
-
Citations
Citations to this article as recorded by- Virtual surgical planning with dual-stage guide using internal irrigation for cortical plate access and apicectomy
Hadeel M. Abdelhamid, Andrew B. Cameron, Roy George
Saudi Endodontic Journal.2026; 16(1): 121. CrossRef - Accuracy of 3‐dimensional surgical guide for endodontic microsurgery with a new design concept: A cadaver study
Se‐Won Ha, Stephanie M. Choi, Sunil Kim, Minju Song, Kyung‐Seok Hu, Euiseong Kim
International Endodontic Journal.2025; 58(2): 295. CrossRef - Expert consensus on apical microsurgery
Hanguo Wang, Xin Xu, Zhuan Bian, Jingping Liang, Zhi Chen, Benxiang Hou, Lihong Qiu, Wenxia Chen, Xi Wei, Kaijin Hu, Qintao Wang, Zuhua Wang, Jiyao Li, Dingming Huang, Xiaoyan Wang, Zhengwei Huang, Liuyan Meng, Chen Zhang, Fangfang Xie, Di Yang, Jinhua Yu
International Journal of Oral Science.2025;[Epub] CrossRef - Apicoectomy: A review of clinical concepts and techniques
Vivek Thakur, Rahul Kaul
Journal of Oral Research and Review.2025; 17(1): 77. CrossRef - Management of Periapical Lesion and Discoloration with Periapical Microsurgery Followed up by Internal-External Bleaching and Direct Composite Restoration: One-Year Clinical Evaluation
Opik Hidayat, Suhardjo Sitam, Irmaleny Irmaleny, Setyo Harnowo, Wawan Suridwan
Clinical, Cosmetic and Investigational Dentistry.2025; Volume 17: 217. CrossRef - Guided endodontics in the application of personalized mini-invasive treatment in clinical cases: a literature review
Shuangshuang Ren, Wanping Wang, Mingyue Cheng, Wenyue Tang, Yue Zhao, Leiying Miao
The Saudi Dental Journal.2025;[Epub] CrossRef - A novel three-dimensional printed guide for handling three strategic steps of surgical endodontics
Ankit Arora, Kavina Desai, Sonali Kapoor, Seema Gajera, Vatsal Joshi
Saudi Endodontic Journal.2025; 15(3): 297. CrossRef - Periapical microsurgical endodontic treatment of the maxillary second premolar: a clinical case
K. A. Ordashiev, S. M. Kurbanova, P. A. Gamzatova, A. K. Dalgatova, K. Z. Agaragimov, S. M. Kadyrbekova, D. R. Kazavatov, R. S. Adzhamatov, K. M. Kaziev, F. M. Murtazalieva
Endodontics Today.2025; 23(4): 692. CrossRef - Dynamically guided transantral piezoelectric endodontic microsurgery: A case report with technical considerations
Paula Andrea Villa‐Machado, Felipe Augusto Restrepo‐Restrepo, Sergio Iván Tobón‐Arroyave
International Endodontic Journal.2024; 57(4): 490. CrossRef - Piezoelectric Endodontic Microsurgery with Modified Cortical Window Technique: A Case Report
Rafael Fernández-Grisales, Wilder Rojas, Carolina Berruecos-Orozco
Journal of Endodontic Microsurgery.2023; 2: 34. CrossRef - The bone lid technique in lateral sinus lift: a systematic review and meta-analysis
Lucia Schiavon, Alessandro Perini, Giulia Brunello, Giada Ferrante, Massimo Del Fabbro, Daniele Botticelli, Fouad Khoury, Stefano Sivolella
International Journal of Implant Dentistry.2022;[Epub] CrossRef - Present status and future directions: Surgical endodontics
Frank C. Setzer, Samuel I. Kratchman
International Endodontic Journal.2022; 55(S4): 1020. CrossRef - Is apicectomy with retrograde filling still relevant in contemporary dental practice? A 25‐year retrospective review
Charles Ezechukwu Anyanechi
Oral Surgery.2022; 15(4): 537. CrossRef - Targeted Endodontic Microsurgery
Smitha Reddy, Sravya Gadhiraju, Akram Quraishi, Shekhar Kamishetty
Contemporary Clinical Dentistry.2022; 13(3): 280. CrossRef - Endodontic Microsurgery of Mandibular Second Molars Using the Bony Lid Approach: A Case Series
Cheng Bi, Mengting Zhou, Yu Zhang, Pei Zheng
Journal of Endodontics.2022; 48(12): 1533. CrossRef - Bone Window Technique in Endodontic Microsurgery – Report of Two Cases
Spyros Floratos, Vasileios Molonis, Apostolos Tsolakis, Stylianos Kykalos, Konstantinos Kontzoglou
Journal of Endodontic Microsurgery.2022; 2: 24. CrossRef - Effect of the Piezoelectric Device on Intraoperative Hemorrhage Control and Quality of Life after Endodontic Microsurgery: A Randomized Clinical Study
Jaya Bharathi, Shweta Mittal, Sanjay Tewari, Shikha Tewari, Jigyasa Duhan, Pankaj Sangwan, Vinay Kumar
Journal of Endodontics.2021; 47(7): 1052. CrossRef - Three-dimensional printing: A revealing pathway to an unpredictable maze
MeetkumarS Dedania, NimishaC Shah, Ankit Arora, Nidhi Pisal
Journal of Conservative Dentistry.2020; 23(5): 533. CrossRef - The Application of “Bone Window” Technique in Endodontic Microsurgery
Su-Min Lee, Ya-Hsin Yu, Yu Wang, Euiseong Kim, Syngcuk Kim
Journal of Endodontics.2020; 46(6): 872. CrossRef - Evaluation of surface integrity of root end cavities prepared using conventional and piezoelectric devices: A scanning electron microscopy study
MithraN Hegde, ManjiriNagesh Honap, Sreenath Narayanan
Indian Journal of Dental Research.2019; 30(5): 772. CrossRef - Targeted Endodontic Microsurgery: Computed Tomography–based Guided Stent Approach with Platelet-rich Fibrin Graft: A Report of 2 Cases
Witold Popowicz, Aleksandra Palatyńska-Ulatowska, Meetu Ralli Kohli
Journal of Endodontics.2019; 45(12): 1535. CrossRef - The bone lid technique in oral surgery: a case series study
S. Sivolella, G. Brunello, F. Fistarol, E. Stellini, C. Bacci
International Journal of Oral and Maxillofacial Surgery.2017; 46(11): 1490. CrossRef
- Virtual surgical planning with dual-stage guide using internal irrigation for cortical plate access and apicectomy
- 2,429 View
- 37 Download
- 22 Crossref


 KACD
KACD

 First
First Prev
Prev


