Search
- Page Path
- HOME > Search
- Garre’s osteomyelitis of the mandible managed by nonsurgical re-endodontic treatment
- Heegyun Kim, Jiyoung Kwon, Hyun-Jung Kim, Soram Oh, Duck-Su Kim, Ji-Hyun Jang
- Restor Dent Endod 2024;49(2):e13. Published online March 18, 2024
- DOI: https://doi.org/10.5395/rde.2024.49.e13
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
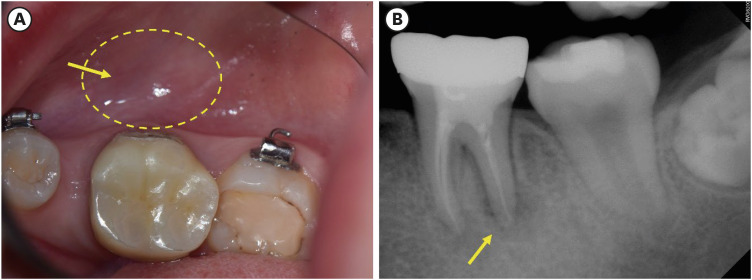
ePub Chronic osteomyelitis with proliferative periostitis, known as Garre’s osteomyelitis, is a type of osteomyelitis characterized by a distinctive gross thickening of the periosteum of bones. Peripheral reactive bone formation can be caused by mild irritation or infection. Garre’s osteomyelitis is usually diagnosed in children and young adults, and the mandible is more affected than the maxilla. The following is a case report of a 12-year-old female patient with Garre’s osteomyelitis of the mandible due to an infection of a root canal-treated tooth. Without surgical intervention, the patient’s symptoms were relieved through nonsurgical root canal re-treatment with long-term calcium hydroxide placement. A cone-beam computed tomography image obtained 6 months after treatment completion displayed complete healing of the periapical lesion and resolution of the peripheral reactive buccal bone. Due to the clinical features of Garre's osteomyelitis, which is characterized by thickening of the periosteum, it can be mistaken for other diseases such as fibrous dysplasia. It is important to correctly diagnose Garre's osteomyelitis based on its distinctive clinical features to avoid unnecessary surgical intervention, and it can lead to minimally invasive treatment options.
-
Citations
Citations to this article as recorded by- Focal osteomyelitis with proliferative periostitis
Zarah Yakoob
South African Dental Journal.2025; 79(09): 508. CrossRef - Garré’s osteomyelitis of the mandible in an adolescent: a case report
Wiem Feki, Imen Haddar, Marwa Bahloul, Zeineb Mnif, Thouraya Kammoun, Ines Maaloul
Journal of Medical Case Reports.2025;[Epub] CrossRef - Garré’s Chronic Sclerosing Osteomyelitis: An Overview of Clinical and Radiologic Features
Mohamed Fadil, Ayman Farouki, Rachida Saouab, Hassan En-nouali, Jamal El Fenni, Zakariya Toufga
Oxford Medical Case Reports.2025;[Epub] CrossRef
- Focal osteomyelitis with proliferative periostitis
- 7,218 View
- 183 Download
- 2 Web of Science
- 3 Crossref

- Mandibular bone necrosis after use of paraformaldehyde-containing paste
- Chi-hwan Lee, Yoorina Choi, Sujung Park
- Restor Dent Endod 2016;41(4):332-337. Published online November 8, 2016
- DOI: https://doi.org/10.5395/rde.2016.41.4.332
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Paraformaldehyde has been used in the past as a pulpotomy agent. However, it has a severe cytotoxic effect and may cause alveolar bone necrosis. Depulpin, a devitalizing agent containing 49% paraformaldehyde, is no longer used frequently due to its severe side effects. In the two cases described in the present study, Depulpin was used as a devitalizing agent during root canal treatment. It caused a gradual loss of sensibility in adjacent teeth, gingival necrosis, and osteomyelitis. This case report demonstrates the serious side effects of using a paraformaldehyde-containing paste as a devitalizing agent for pulp, particularly mandibular bone necrosis.
-
Citations
Citations to this article as recorded by- Numb chin syndrome caused by paraformaldehyde-containing devitalizing agent – Case report
Jyh-Kwei Chen, Yeung-Yi Hsu, Chun-Pin Chiang, Meng-Ling Chiang
Journal of Dental Sciences.2023; 18(2): 955. CrossRef - Non-radiation and non-drug–induced maxillary osteomyelitis: Study of underlying risk factors, presentation, management and treatment outcomes
Kumar Nilesh, Pankaj Patil, Digvijay Patil, Monica Patil
Medical Journal Armed Forces India.2022; 78: S145. CrossRef - Acute toxicity potential and impact on periodontal and periapical tissue of Pulp Out: A paste contained jatropha, sidaguri, and melittin
Maria Tanumihardja, A.M. Windha, N. Musfirah, G.K. Punggawa, Andi Fatima, A.H.M. Nur Fadhila, Esfandiary, Nurhayaty Natsir, Husni Cangara, Lukman Muslimin
Toxicology Reports.2022; 9: 1788. CrossRef - Comparative evaluation of the effect of two pulpal medicaments on pain and bleeding status of mandibular molars with irreversible pulpitis post-failure of inferior alveolar nerve block: a double-blind, randomized, clinical trial
Naomi Ranjan Singh, Lora Mishra, Ajinkya M. Pawar, Nike Kurniawati, Dian Agustin Wahjuningrum
PeerJ.2022; 10: e13397. CrossRef - Dental implant restoration of mandibular bone necrosis defects caused by use of paraformaldehyde-containing paste: A case report
Won-Pyo Lee, Ho-Keel Hwang, Hyoung-Hoon Jo
Oral Biology Research.2019; 43(1): 110. CrossRef - Is Panoramic Radiography an Accurate Imaging Technique for the Detection of Endodontically Treated Asymptomatic Apical Periodontitis?
Cosimo Nardi, Linda Calistri, Giulia Grazzini, Isacco Desideri, Chiara Lorini, Mariaelena Occhipinti, Francesco Mungai, Stefano Colagrande
Journal of Endodontics.2018; 44(10): 1500. CrossRef - A case of high density abnormality in x-ray findings of mandible caused by leakage of root canal filling paste
Haruko Kashiwamura, Kyoko Oka, Yoko Tuchihashi, Hanako Yoshioka, Mayumi Kato, Atsuko Baba, Toyohiro Kagawa, Kazuhiko Okamura, Masao Ozaki
Pediatric Dental Journal.2017; 27(3): 162. CrossRef
- Numb chin syndrome caused by paraformaldehyde-containing devitalizing agent – Case report
- 2,547 View
- 17 Download
- 7 Crossref


 KACD
KACD

 First
First Prev
Prev


