Search
- Page Path
- HOME > Search
- Shape and anatomical relationship of the mental foramen to the mandibular premolars in an Indian sub-population: a retrospective CBCT analysis
- Komal Sheth, Kulvinder Singh Banga, Ajinkya M. Pawar, James L. Gutmann, Hyeon-Cheol Kim
- Restor Dent Endod 2022;47(1):e1. Published online December 13, 2021
- DOI: https://doi.org/10.5395/rde.2022.47.e1
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives This study assessed the shape and anatomical relationship of the mental foramen (MF) to mandibular posterior teeth in an Indian sub-population.
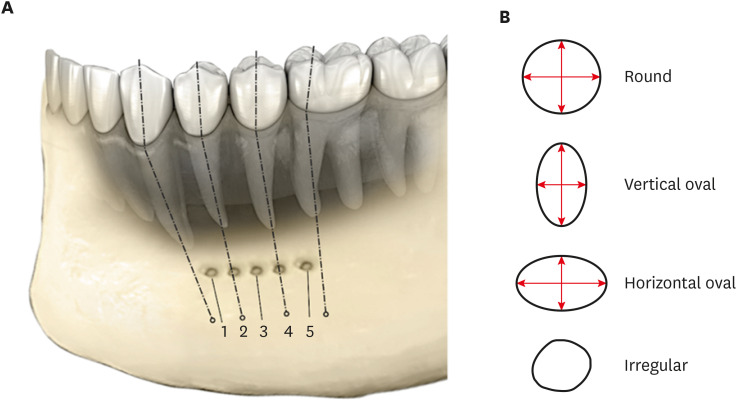
Materials and Methods In total, 475 existing cone-beam computed tomography records exhibiting 950 MFs and including the bilateral presence of mandibular premolars and first molars were assessed. Images were evaluated 3-dimensionally to ascertain the position, shape, and anatomical proximity of MFs to mandibular teeth. The position and shape of MFs were measured and calculated. The Pythagorean theorem was used to calculate the distance between the root apex of the mandibular teeth and the MF.
Results MFs exhibited a predominantly round shape (left: 67% and right: 65%) followed by oval (left: 30% and right: 31%) in both males and females and in different age groups. The root apices of mandibular second premolars (left: 71% and right: 62%) were closest to the MF, followed by distal to the first premolars and mesial to the second premolars. The mean vertical distance between the MF and the nearest tooth apex calculated on sagittal sections was 2.20 mm on the right side and 2.32 mm on the left side; no significant difference was found according to sex or age. The distance between the apices of the teeth and the MF was ≥ 4 mm (left; 4.09 ± 1.27 mm and right; 4.01 ± 1.15 mm).
Conclusions These findings highlight the need for clinicians to be aware of the location of the MF in treatment planning and while performing non-surgical and surgical endodontic procedures.
-
Citations
Citations to this article as recorded by- Optimising Treatment Strategies: Labial versus Labio-inferior Plating Using Three-dimensional Miniplates for Mandibular Symphysis and Parasymphysis Fractures
Akash P Muralidharan, Kalyani Bhate, K Mithun Nilgiri, Sumithra S Nair, Lakshmi Shetty, Rose Johnson
Advances in Human Biology.2025; 15(2): 242. CrossRef - Morphometric analysis of mental foramen in retained cadaveric specimens of mandibles of Sri Lankan population
Dadallage Tharanga De Silva, Usliyanage Clifford Priyantha Perera
Anatomical Science International.2025;[Epub] CrossRef - A Cross-Sectional CBCT Study of Anterior Loop, Accessory Mental Foramen, and Lingual Foramina in Patients’ Mandibles: Implications for Safer Implant Planning
Abbas Shokri, Mohammad Mahdi Maleki, Leili Tapak
Journal of Maxillofacial and Oral Surgery.2025;[Epub] CrossRef - Radiographic Recognition of Mental Nerve for Secured Dental Implant Placement by Cone-Beam Computed Tomography in Mosul City Population
Asmaa B. Al-Saffar, Mekdad H. Alrigbo, Rawaa Y. Al-Rawee
Journal of Craniofacial Surgery.2024; 35(7): 2049. CrossRef - Accuracy of Implant Size Prediction Based on Edentulous Ridge Dimension on Cone-beam Computed Tomography - A Retrospective Study
Hunter R. Jolicoeur, Gerard A. Camargo, Tamara G. Stephenson, Wenjian Zhang
Annals of Maxillofacial Surgery.2024; 14(2): 187. CrossRef - Mental Foramenin Panoramik Radyografi ve Konik Işınlı Bilgisayarlı Tomografi Görüntüleri Üzerinde Morfolojik Analizi
Ezgi UZUN, Burak Kerem APAYDIN, Ayşen TİL
Selcuk Dental Journal.2023; 10(3): 540. CrossRef - Evaluation of the Possible Relationship between the Curvature and
Horizontal Course of the Inferior Alveolar Canal
Cansu G. Koca, M. Fatih Çiçek, Sanaz Sadry, Ozan Yenidünya, Fatma Akkoca Kaplan, Aras Erdil
Current Medical Imaging Formerly Current Medical Imaging Reviews.2023;[Epub] CrossRef
- Optimising Treatment Strategies: Labial versus Labio-inferior Plating Using Three-dimensional Miniplates for Mandibular Symphysis and Parasymphysis Fractures
- 2,771 View
- 46 Download
- 8 Web of Science
- 7 Crossref

- Mental nerve paresthesia secondary to initiation of endodontic therapy: a case report
- Syed Mukhtar-Un-Nisar Andrabi, Sharique Alam, Afaf Zia, Masood Hasan Khan, Ashok Kumar
- Restor Dent Endod 2014;39(3):215-219. Published online May 8, 2014
- DOI: https://doi.org/10.5395/rde.2014.39.3.215
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Whenever endodontic therapy is performed on mandibular posterior teeth, damage to the inferior alveolar nerve or any of its branches is possible. Acute periapical infection in mandibular posterior teeth may also sometimes disturb the normal functioning of the inferior alveolar nerve. The most common clinical manifestation of these insults is the paresthesia of the inferior alveolar nerve or mental nerve paresthesia. Paresthesia usually manifests as burning, prickling, tingling, numbness, itching or any deviation from normal sensation. Altered sensation and pain in the involved areas may interfere with speaking, eating, drinking, shaving, tooth brushing and other events of social interaction which will have a disturbing impact on the patient. Paresthesia can be short term, long term or even permanent. The duration of the paresthesia depends upon the extent of the nerve damage or persistence of the etiology. Permanent paresthesia is the result of nerve trunk laceration or actual total nerve damage. Paresthesia must be treated as soon as diagnosed to have better treatment outcomes. The present paper describes a case of mental nerve paresthesia arising after the start of the endodontic therapy in left mandibular first molar which was managed successfully by conservative treatment.
-
Citations
Citations to this article as recorded by- Evolving Paradigms in the Management of Trigeminal Nerve Injuries Post Oral Surgery: A Comprehensive Narrative Review
Saanvi Tank, Amit Patil, Tejal Patil, Minal M Kshirsagar, Aarti S Bedia, Sanpreet S Sachdev, Vyshnavi Mundada
Cureus.2025;[Epub] CrossRef - Separated Surgical Instrument During the Extraction of a Third Molar: A Case Report
Abdulaziz A Mahdi, Abdullah I Alkharji, Safa A Alburayh, Bader A Fatani, Osama A Alharbi
Cureus.2025;[Epub] CrossRef - Treatment of paresthesia induced by periapical lesions: a case report
Hyo Jin Jo, Jung-Hong Ha
Journal of Dental Rehabilitation and Applied Science.2024; 40(4): 305. CrossRef - İMPLANT CERRAHİSİ SONRASI HİPOESTEZİ-6 AYLIK TAKİP: VAKA SERİSİ
Sefa AYDINDOĞAN, Emine Elif MUTAFCİLAR VELİOĞLU, Yunus Emre BALABAN
Selcuk Dental Journal.2023; 10(4): 350. CrossRef - Mental Nerve Paraesthesia: A Report of Two Cases Associated with Endodontic Etiology
Neeta Patel, Akshayraj Langaliya, Shikha Kanodia, Aravind Kumbhar, Aastha Buch, Aarshvi Shah, Himani Bhatt, Drashti Panchal, Sharan Shah, Jinali Shah, Darko Macan
Case Reports in Dentistry.2021;[Epub] CrossRef - Anatomic Danger Zones of the Head and Neck
Guy Talmor, Andy Trang, Omeed Ahadiat, Boris Paskhover, Ashley Wysong
Dermatologic Surgery.2020; 46(12): 1549. CrossRef - The anatomical relationship between the roots of erupted permanent teeth and the mandibular canal: a systematic review
Michał Puciło, Mariusz Lipski, Magdalena Sroczyk-Jaszczyńska, Aleksandra Puciło, Alicja Nowicka
Surgical and Radiologic Anatomy.2020; 42(5): 529. CrossRef - Endodontic-related inferior alveolar nerve injuries: A review and a therapeutic flow chart
R. Castro, M. Guivarc'h, J.M. Foletti, J.H. Catherine, C. Chossegros, L. Guyot
Journal of Stomatology, Oral and Maxillofacial Surgery.2018; 119(5): 412. CrossRef - Neuropathy of Trigeminal Nerve Branches After Oral and Maxillofacial Treatment
Jimoh Olubanwo Agbaje, Elke Van de Casteele, Marjolein Hiel, Ciska Verbaanderd, Ivo Lambrichts, Constantinus Politis
Journal of Maxillofacial and Oral Surgery.2016; 15(3): 321. CrossRef - Facial nerve paralysis following endodontic treatment of lower first molar
Umut Demetoglu, Gokhan Ozkan, Hasan Onur Simsek
Journal of Oral and Maxillofacial Surgery, Medicine, and Pathology.2016; 28(3): 267. CrossRef - Broken Endodontic Instrument Caused Inferior Alveolar Nerve Paraesthesia: A Case Report.
M. Ozbek Selcuk, Kaman Süleyman, Ozgur Demiralp Kemal
Journal of Dentistry And Oral Implants.2016; 1(1): 21. CrossRef
- Evolving Paradigms in the Management of Trigeminal Nerve Injuries Post Oral Surgery: A Comprehensive Narrative Review
- 2,797 View
- 12 Download
- 11 Crossref


 KACD
KACD

 First
First Prev
Prev


