Search
- Page Path
- HOME > Search
- Microleakage and characteristics of resin-tooth tissues interface of a self-etch and an etch-and-rinse adhesive systems
- Xuan Vinh Tran, Khanh Quang Tran
- Restor Dent Endod 2021;46(2):e30. Published online May 18, 2021
- DOI: https://doi.org/10.5395/rde.2021.46.e30
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives This study was conducted to compare the microleakage and characteristics of the resin-tooth tissue interface between self-etch and etch-and-rinse adhesive systems after 48 hours and 3 months.
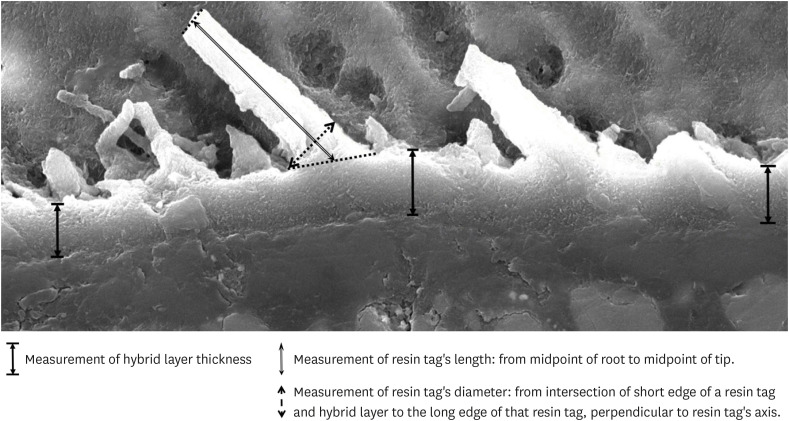
Materials and Methods 40 extracted premolar teeth were randomly divided into 2 groups: 1-step self-etch adhesive system – Optibond™ All-In-One, and 2-step etch-and-rinse adhesive system - Adper™ Single Bond 2. Both groups were subjected to 500 thermocycles (5°C–55°C) before scanning electron microscope (SEM) analysis or microleakage trial at 48-hour and 3-month time periods.
Results SEM images showed the hybrid layer thickness, diameter, and length of resin tags of the self-etch adhesive (0.42 ± 0.14 µm; 1.49 ± 0.45 µm; 16.35 ± 14.26 µm) were smaller than those of the etch-and-rinse adhesive (4.39 ± 1.52 µm; 3.49 ± 1 µm; 52.81 ± 35.81 µm). In dentin, the microleakage scores of the 2 adhesives were not different in both time periods (48 hours/3 months). However, the microleakage score of etch-and-rinse adhesive increased significantly after 3 months (0.8 ± 0.63 and 1.9 ± 0.88,
p < 0.05).Conclusions The self-etch adhesive exhibited better long-term sealing ability in dentin when compared to that of the etch-and-rinse adhesive. The greater hybrid layer thickness and dimensions of resin tags did not guarantee reliable, long-lasting sealing in the bonding area.
-
Citations
Citations to this article as recorded by- A systematic review of shear bond strength of sixth- and fourth-generation adhesives in primary teeth
Maryam Hajiahmadi, Najmeh Akhlaghi, Hamid Mosleh, Ehsan Samani, Sheida Bagheri, Zohreh Salehi
Dental Research Journal.2026;[Epub] CrossRef - Efficacy of different adhesive systems in bonding direct resin composite restorations: a systematic review and meta-analysis
Ravinder S. Saini, Rajesh Vyas, Sunil Kumar Vaddamanu, Syed Altafuddin Quadri, Seyed Ali Mosaddad, Artak Heboyan
Evidence-Based Dentistry.2025; 26(2): 115. CrossRef - Characterisation of universal adhesive bonded resin-dentin interface after focused ultrasound smear layer conditioning
Cheryl Fu, Peta L. Clode, Amr S. Fawzy
International Journal of Adhesion and Adhesives.2025; 142: 104115. CrossRef - Effect of Dentin Pretreatment With Dimethyl Sulfoxide Solution on Interfacial Fracture Toughness of Composite Resin to Wet and Dry Dentin
Fatemeh Molaei, Mehrsima Ghavami-Lahiji, Seyedeh Maryam Tavangar, Hannah Wesley
International Journal of Dentistry.2025;[Epub] CrossRef - Resin tags formation by modified Renewal MI formulations in a carious dentine model
Nabih Alkhouri, Wendy Xia, Paul Ashley, Anne Young
Frontiers in Oral Health.2024;[Epub] CrossRef - Effect of propolis added to single‐bottle adhesives on water permeation through the hybrid layer
Lucineide Silva da Rocha, Daniela Ferreira de Oliveira, Cinthya Luna Veloso de Lima, Ticiano Gomes do Nascimento, Johnnatan Duarte de Freitas, Jeniffer Mclaine Duarte de Freitas, Isabel Cristina Celerino de Moraes Porto
European Journal of Oral Sciences.2024;[Epub] CrossRef - Exploration and preliminary clinical investigation of an adhesive approach for primary tooth restoration
Xiangqin Xu, Jiansheng Zhu, May Lei Mei, Huaying Wu, Kaipeng Xie, Shoulin Wang, Yaming Chen
The Journal of Biomedical Research.2023; 37(2): 138. CrossRef - Adhesion to enamel and dentine: an update
Rana Alkattan
Primary Dental Journal.2023; 12(3): 33. CrossRef - Effects of carbodiimide combined with ethanol–wet bonding pretreatment on dentin bonding properties: an in vitro study
Xiaoxiao You, Long Chen, Jie Xu, Sihui Li, Zhenghao Zhang, Ling Guo
PeerJ.2022; 10: e14238. CrossRef - The effects of amalgam contamination and different surface modifications on microleakage of dentin bonded to bulk fill composite when using different adhesive protocols
Nojoud Alshehri, Abdullah Aljamhan, Mohammed Bin-Shuwaish
BMC Oral Health.2022;[Epub] CrossRef - Development of low-shrinkage dental adhesives via blending with spiroorthocarbonate expanding monomer and unsaturated epoxy resin monomer
Zonghua Wang, Xiaoran Zhang, Shuo Yao, Jiaxin Zhao, Chuanjian Zhou, Junling Wu
Journal of the Mechanical Behavior of Biomedical Materials.2022; 133: 105308. CrossRef - Influence of silver nanoparticles on the resin-dentin bond strength and antibacterial activity of a self-etch adhesive system
Jia Wang, Wei Jiang, Jingping Liang, Shujun Ran
The Journal of Prosthetic Dentistry.2022; 128(6): 1363.e1. CrossRef
- A systematic review of shear bond strength of sixth- and fourth-generation adhesives in primary teeth
- 2,641 View
- 41 Download
- 10 Web of Science
- 12 Crossref

- Bonding efficacy of cured or uncured dentin adhesives in indirect resin
- Ji-Hyun Jang, Bin-Na Lee, Hoon-Sang Chang, Yun-Chan Hwang, Won-Mann Oh, In-Nam Hwang
- J Korean Acad Conserv Dent 2011;36(6):490-497. Published online November 30, 2011
- DOI: https://doi.org/10.5395/JKACD.2011.36.6.490
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives This study examined the effect of the uncured dentin adhesives on the bond interface between the resin inlay and dentin.
Materials and Methods Dentin surface was exposed in 24 extracted human molars and the teeth were assigned to indirect and direct resin restoration group. For indirect resin groups, exposed dentin surfaces were temporized with provisional resin. The provisional restoration was removed after 1 wk and the teeth were divided further into 4 groups which used dentin adhesives (OptiBond FL, Kerr; One-Step, Bisco) with or without light-curing, respectively (Group OB-C, OB-NC, OS-C and OS-NC). Pre-fabricated resin blocks were cemented on the entire surfaces with resin cement. For the direct resin restoration groups, the dentin surfaces were treated with dentin adhesives (Group OB-D and OS-D), followed by restoring composite resin. After 24 hr, the teeth were assigned to microtensile bond strength (µTBS) and confocal laser scanning microscopy (CLSM), respectively.
Results The indirect resin restoration groups showed a lower µTBS than the direct resin restoration groups. The µTBS values of the light cured dentin adhesive groups were higher than those of the uncured dentin adhesive groups (
p < 0.05). CLSM analysis of the light cured dentin adhesive groups revealed definite and homogenous hybrid layers. However, the uncured dentin adhesive groups showed uncertain or even no hybrid layer.Conclusions Light-curing of the dentin adhesive prior to the application of the cementing material in luting a resin inlay to dentin resulted in definite, homogenous hybrid layer formation, which may improve the bond strength.
- 1,600 View
- 10 Download

- Effect of Er:YAG lasing on the dentin bonding strength of two-step adhesives
- Byeong-Choon Song, Young-Gon Cho, Myung-Seon Lee
- J Korean Acad Conserv Dent 2011;36(5):409-418. Published online September 30, 2011
- DOI: https://doi.org/10.5395/JKACD.2011.36.5.409
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives The purpose of this study was to compare the microshear bond strength (µSBS) and bonding interfaces of two-step total-etching and self-etching adhesive systems to three etch types of dentin either the acid etched, laser etched or laser and acid etched.
Materials and Methods The occlusal dentinal surfaces of thirty human molars were used. They were divided into six groups: group 1, 37% H3PO4 + Single Bond 2 (3M ESPE); group 2, Er:YAG laser (KEY Laser 3, KaVo) + Single Bond 2; group 3, Er:YAG laser + 37% H3PO4 + Single Bond 2; group 4, Clearfil SE Primer + Bond (Kuraray); group 5, Er:YAG laser + Clearfil SE Bond; group 6, Er:YAG laser + Clearfil SE Primer + Bond. The samples were subjected to µSBS testing 24 hr after bonding. Also scanning microscopic evaluations were made on the resin-dentin interfaces of six specimens.
Results The µSBS of group 2 was significantly lower than that of groups 1 and 3 in Single Bond 2 (
p < 0.05). There were significant differences among the uSBS of groups 4, 5, and 6 in Clearfil SE Bond (p < 0.05). Very short and slender resin tags were observed in groups 2 and 5. Long and slender resin tags and lateral branches of tags were observed in groups 3 and 6.Conclusions Treatment of dentin surface using phosphoric acid or self-etching primer improved the adhesion of Er:YAG lased dentin.
-
Citations
Citations to this article as recorded by- Effect of Acid or Laser Treatment on Degradation of Dentin Matrix
Aslihan Usumez, Tugrul Sari, Roda Seseogullari Dirihan, Mehmet Esad Guven, Serra Oguz Ahmet, Norbert Gutknecht, Arzu Tezvergil Mutluay
Lasers in Dental Science.2022; 6(2): 99. CrossRef - Ablation of carious dental tissue using an ultrashort pulsed laser (USPL) system
Christoph Engelbach, Claudia Dehn, Christoph Bourauel, Jörg Meister, Matthias Frentzen
Lasers in Medical Science.2015; 30(5): 1427. CrossRef
- Effect of Acid or Laser Treatment on Degradation of Dentin Matrix
- 961 View
- 1 Download
- 2 Crossref

- Cuspal deflection in class V cavities restored with composite resins
- Jun-Gyu Park, Bum-Soon Lim, In-Bog Lee
- J Korean Acad Conserv Dent 2008;33(2):83-89. Published online March 31, 2008
- DOI: https://doi.org/10.5395/JKACD.2008.33.2.083
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub The purpose of this study was to evaluate the effect of the polymerization shrinkage and modulus of elasticity of composites on the cusp deflection of class V restoration in premolars. The sixteen extracted upper premolars were divided into 2 groups with similar size. The amounts of cuspal deflection were measured in Class V cavities restored with a flowable composite (Filtek flow) or a universal hybrid composite (Z-250). The bonded interfaces of the sectioned specimens were observed using a scanning electron microscopy (SEM). The polymerization shrinkage and modulus of elasticity of the composites were measured to find out the effect of physical properties of composite resins on the cuspal deflection. The results were as follows.
The amounts of cuspal deflection restored with Filtek flow or Z-250 were 2.18 ± 0.92 µm and 2.95 ± 1.13 µm, respectively. Filtek flow showed less cuspal deflection but there was no statistically significant difference (p > 0.05).
The two specimens in each group showed gap at the inner portion of the cavity.
The polymerization shrinkages of Filtek flow and Z-250 were 4.41% and 2.23% respectively, and the flexural modulus of elasticity of cured Filtek flow (7.77 GPa) was much lower than that of Z-250 (17.43 GPa).
The cuspal deflection depends not only on the polymerization shrinkage but also on the modulus of elasticity of composites.
-
Citations
Citations to this article as recorded by- Comparison of marginal microleakage between low and high flowable resins in class V cavity
Sang-Bae Bae, Young-Gon Cho, Myeong-Seon Lee
Journal of Korean Academy of Conservative Dentistry.2009; 34(6): 477. CrossRef - A survey on the use of composite resin in Class II restoration in Korea
Dong-Ho Shin, Se-Eun Park, In-Seok Yang, Juhea Chang, In-Bog Lee, Byeong-Hoon Cho, Ho-Hyun Son
Journal of Korean Academy of Conservative Dentistry.2009; 34(2): 87. CrossRef - Effect of instrument compliance on the polymerization shrinkage stress measurements of dental resin composites
Deog-Gyu Seo, Sun-Hong Min, In-Bog Lee
Journal of Korean Academy of Conservative Dentistry.2009; 34(2): 145. CrossRef - The change of the initial dynamic visco-elastic modulus of composite resins during light polymerization
Min-Ho Kim, In-Bog Lee
Journal of Korean Academy of Conservative Dentistry.2009; 34(5): 450. CrossRef
- Comparison of marginal microleakage between low and high flowable resins in class V cavity
- 1,326 View
- 7 Download
- 4 Crossref

- A study on fractural behavior of dentin-resin interface
- Gil-Joo Ryu, Gi-Woon Choi, Sang-Jin Park, Kyung-Kyu Choi
- J Korean Acad Conserv Dent 2007;32(3):208-221. Published online May 31, 2007
- DOI: https://doi.org/10.5395/JKACD.2007.32.3.208
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub The fracture toughness test is believed as a clinically relevant method for assessing the fracture resistance of the dentinal restoratives. The objectives of this study were to measure the fracture toughness (K1C) and microtensile bond strength of dentin-resin composite interface and compare their relationship for their use in evaluation of the integrity of the dentin-resin bond.
A minimum of six short-rod specimens for fracture toughness test and fifteen specimens for microtensile bond strength test was fabricated for each group of materials used. After all specimens storing for 24 hours in distilled water at 37℃, they were tensile-loaded with an EZ tester universal testing machin. Statistical analysis was performed using ANOVA and Tukey's test at the 95% confidence level, Pearson's coefficient was used to verify the correlation between the mean of fracture toughness and microtensile bond strength. FE-SEM was employed on fractured surface to describe the crack propagation.
Fracture toughness value of Clearfil SE Bond (SE) was the highest, followed by Adper Single Bond 2 (SB), OptiBond Solo (OB), ONE-STEP PLUS (OS), ScotchBond Multi-purpose (SM) and there was significant difference between SE and other 4 groups (p < 0.05). There were, however, no significant difference among SB, OB, OS, SM (p > 0.05). Microtensile bond strength of SE was the highest, followed by SB, OB, SM, OS and OS only showed significant lower value (p < 0.05). There was no correlation between fracture toughness and microtensile bond strength values. FE-SEM examination revealed that dentin bonding agent showed different film thickness and different failure pattern according to the film thickness.
From the limited results of this study, it was noted that there was statistically no correlation between K1C and µTBS. We can conclude that for obtaining the reliability of bond strength test of dentin bonding agent, we must pay more attention to the test procedure and its profound scrutiny.
-
Citations
Citations to this article as recorded by- The study of fractural behavior of repaired composite
Sang-Soon Park, Wook Nam, Ah-Hyang Eom, Duck-Su Kim, Gi-Woon Choi, Kyoung-Kyu Choi
Journal of Korean Academy of Conservative Dentistry.2010; 35(6): 461. CrossRef
- The study of fractural behavior of repaired composite
- 1,182 View
- 4 Download
- 1 Crossref

- Microtensile bond strength of single step adhesives to dentin
- Young-Gon Cho, Young-Jae Kee
- J Korean Acad Conserv Dent 2005;30(4):312-318. Published online July 30, 2005
- DOI: https://doi.org/10.5395/JKACD.2005.30.4.312
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub This study compared the microtensile bond strength (µTBS) of three single step adhesives to dentin.
Occlusal superficial dentin was exposed in fifteen human molars. They were assigned to three groups by used adhesives: Xeno group (Xeno III), Prompt group (Adper Prompt L-Pop), AQ group (AQ Bond).
Each adhesive was applied to dentin surface, and composite of same manufacturer was constructed. The bonded specimens were sectioned into sticks with an interface area approximately 1 mm2, and subjected to µTBS testing with a crosshead speed of 1 mm/minute. The results of this study were as follows;
The µTBS to dentin was 48.78 ± 9.83 MPa for Xeno III, 30.22 ± 4.52 MPa for Adper Prompt L-Pop, and 26.31 ± 7.07 MPa for AQ Bond.
The mean µTBS of Xeno group was significantly higher than that of Prompt group and AQ group (p < 0.05).
There was no significant difference between the µTBS of Prompt group and AQ group.
- 995 View
- 5 Download

- Study on the interface between light-cured glass ionomer base and indirect composite resin inlay and dentin
- Song-Hee Lee, Dong-Jun Kim, Yun-Chan Hwang, Won-Mann Oh, In-Nam Hwang
- J Korean Acad Conserv Dent 2005;30(3):158-169. Published online May 31, 2005
- DOI: https://doi.org/10.5395/JKACD.2005.30.3.158
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub This study was done to evaluate the shear bond strength between light-cured glass ionomer cement (GIC) base and resin cement for luting indirect resin inlay and to observe bonding aspects which is produced at the interface between them by SEM.
Two types of light cured GIC (Fuji II LC Improved, GC Co. Tokyo, Japan and Vitrebond™, 3M, Paul, Minnesota, U.S.A) were used in this study. For shear bond test, GIC specimens were made and immersed in 37℃ distilled water for 1 hour, 24 hours, 1 week and 2 weeks. Eighty resin inlays were prepared with Artglass® (Heraeus Kultzer, Germany) and luted with Variolink® II (Ivoclar Vivadent, Liechtenstein).
Shear bond strength of each specimen was measured and fractured surface were examined. Statistical analysis was done with one-way ANOVA.
Twenty four extracted human third molars were selected and Class II cavities were prepared and GIC based at axiopulpal lineangle. The specimens were immersed in 37℃ distilled water for 1 hour, 24 hours, 1 week and 2 weeks. And then the resin inlays were luted to prepared teeth. The specimens were sectioned vertically with low speed saw. The bonding aspect of the specimens were observed by SEM (JSM-5400®, Jeol, Tokyo, Japan). There was no significant difference between the shear bond strength according to storage periods of light cured GIC base. And cohesive failure was mostly appeared in GIC. On scanning electron micrograph, about 30 - 120 µm of the gaps were observed on the interface between GIC base and dentin. No gaps were observed on the interface between GIC and resin inlay.
-
Citations
Citations to this article as recorded by- Comparative analysis of strain according to two wavelengths of light source and constant temperature bath deposition in ultraviolet-curing resin for dental three-dimensional printing
Dong-Yeon Kim, Gwang-Young Lee, Hoo-Won Kang, Cheon-Seung Yang
Journal of Korean Acedemy of Dental Technology.2020; 42(3): 208. CrossRef
- Comparative analysis of strain according to two wavelengths of light source and constant temperature bath deposition in ultraviolet-curing resin for dental three-dimensional printing
- 1,123 View
- 0 Download
- 1 Crossref


 KACD
KACD

 First
First Prev
Prev


