Search
- Page Path
- HOME > Search
- Anesthetic efficacy in vital asymptomatic teeth using different local anesthetics: a systematic review with network meta-analysis
- Amy Kia Cheen Liew, Yi-Chun Yeh, Dalia Abdullah, Yu-Kang Tu
- Restor Dent Endod 2021;46(3):e41. Published online July 21, 2021
- DOI: https://doi.org/10.5395/rde.2021.46.e41
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub Objectives This study aimed to evaluate the efficacy of various local anesthesia (LA) in vital asymptomatic teeth.
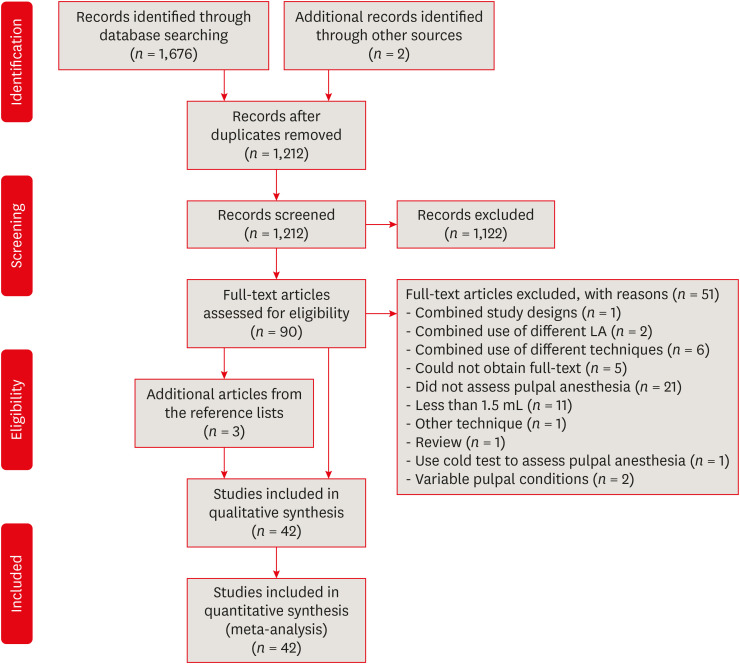
Materials and Methods Randomized controlled trials comparing pulpal anesthesia of various LA on vital asymptomatic teeth were included in this review. Searches were conducted in the Cochrane CENTRAL, MEDLINE (via PubMed), EMBASE, ClinicalTrials.gov, Google Scholar and 3 field-specific journals from inception to May 3, 2019. Study selection, data extraction, and risk of bias assessment using Cochrane Risk of Bias Tool were done by 2 independent reviewers in duplicate. Network meta-analysis (NMA) was performed within the frequentist setting using STATA 15.0. The LA was ranked, and the surface under the cumulative ranking (SUCRA) line was plotted. The confidence of the NMA estimates was assessed using the CINeMA web application.
Results The literature search yielded 1,678 potentially eligible reports, but only 42 were included in this review. For maxillary buccal infiltration, articaine 4% with epinephrine 1:100,000 was more efficacious than lidocaine 2% with epinephrine 1:100,000 (odds ratio, 2.11; 95% confidence interval, 1.14–3.89). For mandibular buccal infiltration, articaine 4% with epinephrine 1:100,000 was more efficacious than various lidocaine solutions. The SUCRA ranking was highest for articaine 4% with epinephrine when used as maxillary and mandibular buccal infiltrations, and lidocaine 2% with epinephrine 1:80,000 when used as inferior alveolar nerve block. Inconsistency and imprecision were detected in some of the NMA estimates.
Conclusions Articaine 4% with epinephrine is superior when maxillary or mandibular infiltration is required in vital asymptomatic teeth.
-
Citations
Citations to this article as recorded by- Anatomical Basis of the Palatal Injection Technique for Pulpal Anesthesia of Maxillary Teeth
Sergey Kabak, Joe Iwanaga, Yuliya Melnichenko, Ruslan Mekhtiev, Nina Savrasova
Clinical Anatomy.2025;[Epub] CrossRef - Adrenaline in pulp capping treatment of reversible pulpitis
Si-Yun Yang, Jin-Zhu Wang, Hao Fan, Min Chen
World Journal of Clinical Cases.2024; 12(22): 5024. CrossRef - Effect of 810 nm Diode Laser Irradiation on the Time of Initiation and Depth of Anesthesia for Endodontic Treatment of Mandibular First Molars with Symptomatic Irreversible Pulpitis: A Clinical Trial
Elham Khoshbin, Leila Ghasemi, Rooholah Behroozi, Zahra Khosravi, Afsaneh Rahmati, Loghman Rezaeisoufi, Hamed Karkehabadi
Photobiomodulation, Photomedicine, and Laser Surgery.2023; 41(9): 475. CrossRef - The potential of articaine as new generation of local anesthesia in dental clinics: A review
Wen Luo, Kaiyue Zheng, Huifang Kuang, Zhixin Li, Jinrong Wang, Jie Mei
Medicine.2022; 101(48): e32089. CrossRef
- Anatomical Basis of the Palatal Injection Technique for Pulpal Anesthesia of Maxillary Teeth
- 3,919 View
- 37 Download
- 3 Web of Science
- 4 Crossref

- Efficacy of buccal piroxicam infiltration and inferior alveolar nerve block in patients with irreversible pulpitis: a prospective, double-blind, randomized clinical trial
- Saurav Paul, Sridevi Nandamuri, Aakrati Raina, Mukta Bansal
- Restor Dent Endod 2021;46(1):e9. Published online January 26, 2021
- DOI: https://doi.org/10.5395/rde.2021.46.e9
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives This randomized clinical trial aimed to assess the effectiveness of buccal infiltration with piroxicam on the anesthetic efficacy of inferior alveolar nerve block (IANB) with buccal infiltration in irreversible pulpitis, with pain assessed using the Heft-Parker visual analogue scale (HP-VAS).
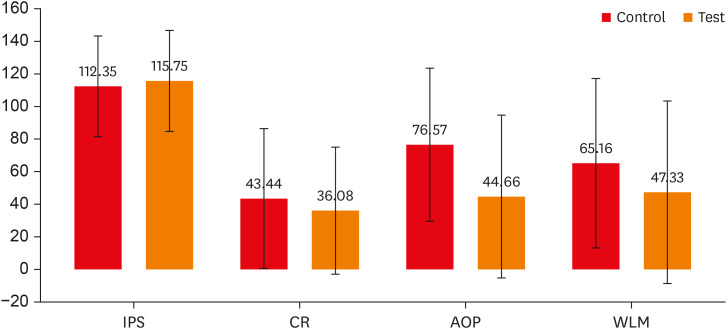
Materials and Methods This study included 56 patients with irreversible pulpitis in mandibular molars, randomly distributed between 2 groups (
n = 28). After evaluating the initial pain score with the HP-VAS, each patient received IANB followed by buccal infiltration of 2% lignocaine with adrenaline (1:80,000). Five minutes later, the patients in groups 1 and 2 were given buccal infiltration with 40 mg/2 mL of piroxicam or normal saline, respectively. An access opening procedure (AOP) was performed 15 minutes post-IANB once the individual showed signs of lip numbness as well as 2 negative responses to electric pulp testing. The HP-VAS was used to grade the patient's pain during caries removal (CR), AOP, and working length measurement (WLM). Successful anesthesia was identified either by the absence of pain or slight pain through CR, AOP, and WLM, with no requirement of a further anesthetic dose. A statistical analysis was done using the Shapiro-Wilk and Mann-WhitneyU tests.Results The piroxicam group presented a significantly lower (
p < 0.05) mean pain score than the saline group during AOP.Conclusions Buccal infiltration with piroxicam enhanced the efficacy of anesthesia with IANB and buccal infiltration with lignocaine in patients with irreversible pulpitis.
-
Citations
Citations to this article as recorded by- Inferior alveolar nerve block success of 2% mepivacaine versus 4% articaine in patients with symptomatic irreversible pulpitis in mandibular molars: A randomized double‐blind single‐centre clinical trial
Mohammed Fawzy Omar Mohammed Habib, Sovana Tarek, Sara Mohamed Elsayed Teama, Khaled Ezzat, Randa Mohamed El Boghdadi, Abeer Marzouk, Manar Yehia Fouda, Shaimaa Ismail Gawdat, Marwa Mahmoud Bedier, Suzan Abdul Wanees Amin
International Endodontic Journal.2022; 55(11): 1177. CrossRef - Present status and future directions—Mechanisms and management of local anaesthetic failures
Masoud Parirokh, Paul V. Abbott
International Endodontic Journal.2022; 55(S4): 951. CrossRef
- Inferior alveolar nerve block success of 2% mepivacaine versus 4% articaine in patients with symptomatic irreversible pulpitis in mandibular molars: A randomized double‐blind single‐centre clinical trial
- 2,049 View
- 23 Download
- 2 Web of Science
- 2 Crossref

- Accidental injury of the inferior alveolar nerve due to the extrusion of calcium hydroxide in endodontic treatment: a case report
- Yooseok Shin, Byoung-Duck Roh, Yemi Kim, Taehyeon Kim, Hyungjun Kim
- Restor Dent Endod 2016;41(1):63-67. Published online January 6, 2016
- DOI: https://doi.org/10.5395/rde.2016.41.1.63
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
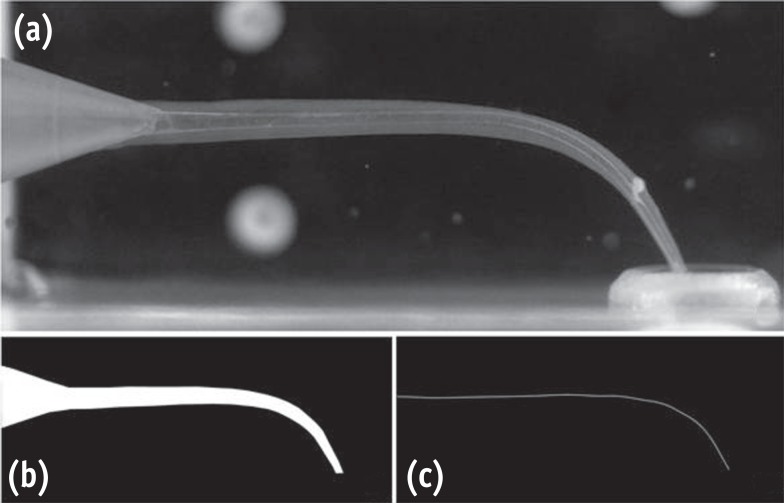
ePub During clinical endodontic treatment, we often find radiopaque filling material beyond the root apex. Accidental extrusion of calcium hydroxide could cause the injury of inferior alveolar nerve, such as paresthesia or continuous inflammatory response. This case report presents the extrusion of calcium hydroxide and treatment procedures including surgical intervention. A 48 yr old female patient experienced Calcipex II extrusion in to the inferior alveolar canal on left mandibular area during endodontic treatment. After completion of endodontic treatment on left mandibular first molar, surgical intervention was planned under general anesthesia. After cortical bone osteotomy and debridement, neuroma resection and neurorrhaphy was performed, and prognosis was observed. But no improvement in sensory nerve was seen following surgical intervention after 20 mon. A clinician should be aware of extrusion of intracanal medicaments and the possibility of damage on inferior alveolar canal. Injectable type of calcium hydroxide should be applied with care for preventing nerve injury. The alternative delivery method such as lentulo spiral was suggested on the posterior mandibular molar.
-
Citations
Citations to this article as recorded by- Nicolau syndrome in endodontics: A narrative review on calcium hydroxide extrusion and its therapeutic risks
Manisha Chaudhary, Akash Kumar Giri, Ashok Ayer
Saudi Endodontic Journal.2026; 16(1): 12. CrossRef - Invasion of Calcium Hydroxide Preparations Leading to Severe Chemical Nerve Injury Treated Through Nerve Repair Using Artificial Nerve Conduit: A Case Report
Akihiro Nishiyama, Andreas Neff, Takahiro Nakada, Takaharu Ariizumi, Akira Iwasaki, Keisuke Sugahara, Akira Katakura, Hannah Wesley
Case Reports in Dentistry.2025;[Epub] CrossRef - Automatic localization of inferior alveolar nerve canal in panoramic dental images
Uma Maheswari Pandyan, Banumathi Arumugam, Ulaganathan Gurunathan, Shahul Hameed Kopuli Ashkar Ali
Signal, Image and Video Processing.2022; 16(5): 1389. CrossRef - Inferior alveolar nerve injury due to the extrusion of calcium hydroxide during endodontic treatment: A case report
Metin Berk Kasapoğlu, Gülce Ecem Doğancalı
Australian Endodontic Journal.2022; 48(2): 342. CrossRef - Inferior alveolar nerve canal segmentation by local features based neural network model
P. Uma Maheswari, A. Banumathi, G. Ulaganathan, R. Yoganandha
IET Image Processing.2022; 16(3): 703. CrossRef - Microsurgical Repair of Inferior Alveolar Nerve Injuries Associated With Endodontic Treatment: Results on Sensory Function and Relief of Pain
Keith A. Sonneveld, Kristopher L. Hasstedt, Roger A. Meyer, Shahrokh C. Bagheri
Journal of Oral and Maxillofacial Surgery.2021; 79(7): 1434. CrossRef - The significance of diagnosis and treatment planning in periapical lesion overfilled with calcium hydroxide paste
Kyoung-Hwa Jung, Eun-Young Kwon, Youn-Kyung Choi, So-Yeun Kim, Hye-Mi Jeon, Jeong-Kil Park
Journal of Dental Rehabilitation and Applied Science.2021; 37(2): 95. CrossRef - The anatomical relationship between the roots of erupted permanent teeth and the mandibular canal: a systematic review
Michał Puciło, Mariusz Lipski, Magdalena Sroczyk-Jaszczyńska, Aleksandra Puciło, Alicja Nowicka
Surgical and Radiologic Anatomy.2020; 42(5): 529. CrossRef - Massive extrusion of calcium hydroxide paste containing barium sulphate during endodontic treatment
Jéssica Montenegro Fonsêca, Natália Rangel Palmier, Gleyson Kleber Amaral‐Silva, Lady Paola Aristizabal Arboleda, José Flávio Affonso Almeida, Mario Fernando de Goes, Pablo Agustin Vargas, Marcio Ajudarte Lopes, Alan Roger Santos‐Silva
Australian Endodontic Journal.2020; 46(2): 257. CrossRef - The double-edged sword of calcium hydroxide in endodontics
Alan H. Gluskin, Gordon Lai, Christine I. Peters, Ove A. Peters
The Journal of the American Dental Association.2020; 151(5): 317. CrossRef - Endodontic-related inferior alveolar nerve injuries: A review and a therapeutic flow chart
R. Castro, M. Guivarc'h, J.M. Foletti, J.H. Catherine, C. Chossegros, L. Guyot
Journal of Stomatology, Oral and Maxillofacial Surgery.2018; 119(5): 412. CrossRef - Relationship between Root Apices and the Mandibular Canal: A Cone-beam Computed Tomographic Comparison of 3 Populations
Alex Lvovsky, Shir Bachrach, Hyeon-Cheol Kim, Ajinkya Pawar, Oleg Levinzon, Joe Ben Itzhak, Michael Solomonov
Journal of Endodontics.2018; 44(4): 555. CrossRef - A case of high density abnormality in x-ray findings of mandible caused by leakage of root canal filling paste
Haruko Kashiwamura, Kyoko Oka, Yoko Tuchihashi, Hanako Yoshioka, Mayumi Kato, Atsuko Baba, Toyohiro Kagawa, Kazuhiko Okamura, Masao Ozaki
Pediatric Dental Journal.2017; 27(3): 162. CrossRef - Oral dysesthesia
Christopher J. Spencer, Gary D. Klasser
The Journal of the American Dental Association.2017; 148(12): 941. CrossRef - Microsurgical Decompression of Inferior Alveolar Nerve After Endodontic Treatment Complications
Bernardo Bianchi, Andrea Ferri, Andrea Varazzani, Michela Bergonzani, Enrico Sesenna
Journal of Craniofacial Surgery.2017; 28(5): 1365. CrossRef
- Nicolau syndrome in endodontics: A narrative review on calcium hydroxide extrusion and its therapeutic risks
- 3,211 View
- 36 Download
- 15 Crossref

- The success rate of bupivacaine and lidocaine as anesthetic agents in inferior alveolar nerve block in teeth with irreversible pulpitis without spontaneous pain
- Masoud Parirokh, Mohammad Hosein Yosefi, Nouzar Nakhaee, Paul V. Abbott, Hamed Manochehrifar
- Restor Dent Endod 2015;40(2):155-160. Published online March 16, 2015
- DOI: https://doi.org/10.5395/rde.2015.40.2.155
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives Achieving adequate anesthesia with inferior alveolar nerve blocks (IANB) is of great importance during dental procedures. The aim of the present study was to assess the success rate of two anesthetic agents (bupivacaine and lidocaine) for IANB when treating teeth with irreversible pulpitis.
Materials and Methods Sixty volunteer male and female patients who required root canal treatment of a mandibular molar due to caries participated in the present study. The inclusion criteria included prolonged pain to thermal stimulus but no spontaneous pain. The patients were randomly allocated to receive either 2% lidocaine with 1:80,000 epinephrine or 0.5% bupivacaine with 1:200,000 epinephrine as an IANB injection. The sensitivity of the teeth to a cold test as well as the amount of pain during access cavity preparation and root canal instrumentation were recorded. Results were statistically analyzed with the Chi-Square and Fischer's exact tests.
Results At the final step, fifty-nine patients were included in the study. The success rate for bupivacaine and lidocaine groups were 20.0% and 24.1%, respectively. There was no significant difference between the two groups at any stage of the treatment procedure.
Conclusions There was no difference in success rates of anesthesia when bupivacaine and lidocaine were used for IANB injections to treat mandibular molar teeth with irreversible pulpitis. Neither agent was able to completely anesthetize the teeth effectively. Therefore, practitioners should be prepared to administer supplemental anesthesia to overcome pain during root canal treatment.
-
Citations
Citations to this article as recorded by- A Morphometric Study of the Mandibular Foramen, Lingula, and the Incidence of Accessory Mandibular Foramina in Dry Mandibles
Yashaswi Singh, Pratibha Shakya, Noor Us Saba, Heena Singh, Navneet Kumar
Cureus.2025;[Epub] CrossRef - A Comparative Evaluation of the Effect of Photobiomodulation on the Depth of Anaesthesia During Endodontic Treatment of Teeth with Symptomatic Irreversible Pulpitis—A Prospective Clinical Trial
Akshita Balivada, R Vinay Chandra, D Krithika, B Arvind, Mrinalini Jaichander, Priyanka Girish
Journal of Pharmacy and Bioallied Sciences.2025; 17(Suppl 2): S1359. CrossRef - Is there a direct relationship between the cost and effectiveness of local anesthetics in lower molars with irreversible pulpitis? Systematic review, meta-analysis and cost-effectiveness evaluation
Luísa Figueredo de Carvalho, Adriana Poli Castilho Dugaich, Alexandra Maria de Melo Schiefler, Letícia Cristine Ramos Ribeiro, Andressa da Silva Barboza, Sheila Cristina Stolf, Rafael Guerra Lund, Juliana Silva Ribeiro de Andrade
Journal of Dentistry.2025; 163: 106175. CrossRef - Effect of topical application of amitriptyline and nortriptyline on irreversible pulpitis pain in teeth with failed pulpal anesthesia after a successful inferior alveolar nerve block: A randomized clinical trial
Armita Vali Sichani, Hossein Baharian, Navid Yaraghi, Zahra Khosravani, Asana Vali Sichani
Dental Research Journal.2024;[Epub] CrossRef - The Effect of the Anatomic Variables on the Success Rate of Anesthesia in Maxillary Molars with Irreversible Pulpitis
Masoud Parirokh, Sina Kakooei, Nouzar Nakhaee, Hamed Manochehrifar, Paul Abbott
Journal of Endodontics.2022; 48(6): 707. CrossRef - Present status and future directions—Mechanisms and management of local anaesthetic failures
Masoud Parirokh, Paul V. Abbott
International Endodontic Journal.2022; 55(S4): 951. CrossRef - Local anesthesia in oral and maxillofacial surgery: A review of current opinion
Yu-Hao Wang, Dian-Ri Wang, Ji-Yuan Liu, Jian Pan
Journal of Dental Sciences.2021; 16(4): 1055. CrossRef - ANATOMICAL STUDY OF MANDIBULAR FORAMEN IN DRY ADULT HUMAN MANDIBLES IN BIHAR STATE REGION
Vijay Kumar Singh, Md. Zahid Hussain, Subodh Kumar
GLOBAL JOURNAL FOR RESEARCH ANALYSIS.2021; : 34. CrossRef - Efficacy of buccal piroxicam infiltration and inferior alveolar nerve block in patients with irreversible pulpitis: a prospective, double-blind, randomized clinical trial
Saurav Paul, Sridevi Nandamuri, Aakrati Raina, Mukta Bansal
Restorative Dentistry & Endodontics.2021;[Epub] CrossRef - Different anesthetics on the efficacy of inferior alveolar nerve block in patients with irreversible pulpitis
Juliana Larocca de Geus, Jane Kenya Nogueira da Costa, Letícia Maíra Wambier, Bianca Medeiros Maran, Alessandro Dourado Loguercio, Alessandra Reis
The Journal of the American Dental Association.2020; 151(2): 87. CrossRef - Efficacy of local anaesthetic solutions on the success of inferior alveolar nerve block in patients with irreversible pulpitis: a systematic review and network meta‐analysis of randomized clinical trials
V. Nagendrababu, S. J. Pulikkotil, A. Suresh, S. K. Veettil, S. Bhatia, F. C. Setzer
International Endodontic Journal.2019; 52(6): 779. CrossRef - The Effect of Sphenopalatine Block on the Postoperative Pain of Endoscopic Sinus Surgery: A Meta‐analysis
Do Hyun Kim, Haram Kang, Se Hwan Hwang
Otolaryngology–Head and Neck Surgery.2019; 160(2): 223. CrossRef - Effect of four local anesthetics (tetracaine, proparacaine, lidocaine, and bupivacaine) on intraocular pressure in dogs
Ali Asghar Sarchahi, Mehdi Eskandari
International Ophthalmology.2019; 39(7): 1467. CrossRef - Strategies for managing pain during endodontic treatment
Paul V. Abbott, Masoud Parirokh
Australian Endodontic Journal.2018; 44(2): 99. CrossRef - Is mepivacaine as effective as lidocaine during inferior alveolar nerve blocks in patients with symptomatic irreversible pulpitis? A systematic review and meta‐analysis
W. A. Vieira, L. R. Paranhos, G. O. Cericato, A. Franco, M. A. G. Ribeiro
International Endodontic Journal.2018; 51(10): 1104. CrossRef - Injectable local anaesthetic agents for dental anaesthesia
Geoffrey St George, Alyn Morgan, John Meechan, David R Moles, Ian Needleman, Yuan-Ling Ng, Aviva Petrie
Cochrane Database of Systematic Reviews.2018;[Epub] CrossRef - Successful pulpal anesthesia for symptomatic irreversible pulpitis
Melissa Drum, Al Reader, John Nusstein, Sara Fowler
The Journal of the American Dental Association.2017; 148(4): 267. CrossRef - The Effect of Photobiomodulation on the Depth of Anesthesia During Endodontic Treatment of Teeth With Symptomatic Irreversible Pulpitis (Double Blind Randomized Clinical Trial)
Sholeh Ghabraei, Nasim Chiniforush, Behnam Bolhari, Mohsen Aminsobhani, Abbas Khosarvi
Journal of Lasers in Medical Sciences.2017; 9(1): 11. CrossRef - Morphometric study on mandibular foramen and incidence of accessory mandibular foramen in mandibles of south Indian population and its clinical implications in inferior alveolar nerve block
R. Shalini, C. RaviVarman, R. Manoranjitham, M. Veeramuthu
Anatomy & Cell Biology.2016; 49(4): 241. CrossRef - The Effect of Maxillary First Molar Root Length on the Success Rate of Buccal Infiltration Anesthesia
Ehsan Moradi Askari, Masoud Parirokh, Nouzar Nakhaee, Hamid Reza Hosseini, Paul V. Abbott
Journal of Endodontics.2016; 42(10): 1462. CrossRef - Efficacy of Ketorolac Buccal Infiltrations and Inferior Alveolar Nerve Blocks in Patients with Irreversible Pulpitis: A Prospective, Double-blind, Randomized Clinical Trial
Nahid Mohammadzadeh Akhlaghi, Behnoush Hormozi, Paul V. Abbott, Zohreh Khalilak
Journal of Endodontics.2016; 42(5): 691. CrossRef
- A Morphometric Study of the Mandibular Foramen, Lingula, and the Incidence of Accessory Mandibular Foramina in Dry Mandibles
- 2,738 View
- 8 Download
- 21 Crossref

- Hypoesthesia after IAN block anesthesia with lidocaine: management of mild to moderate nerve injury
- Sungjoo Moon, Seung-Jong Lee, Euiseong Kim, Chan-Young Lee
- Restor Dent Endod 2012;37(4):232-235. Published online November 21, 2012
- DOI: https://doi.org/10.5395/rde.2012.37.4.232
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Hypoesthesia after an inferior alveolar nerve (IAN) block does not commonly occur, but some cases are reported. The causes of hypoesthesia include a needle injury or toxicity of local anesthetic agents, and the incidence itself can cause stress to both dentists and patients. This case presents a hypoesthesia on mental nerve area followed by IAN block anesthesia with 2% lidocaine. Prescription of steroids for a week was performed and periodic follow up was done. After 1 wk, the symptoms got much better and after 4 mon, hypoesthesia completely disappeared. During this healing period, only early steroid medication was prescribed. In most cases, hypoesthesia is resolved within 6 mon, but being aware of etiology and the treatment options of hypoesthesia is important. Because the hypoesthesia caused by IAN block anesthesia is a mild to moderate nerve injury, early detection of symptom and prescription of steroids could be helpful for improvement of the hypoesthesia.
-
Citations
Citations to this article as recorded by- Botulinum Toxin-A, Generating a Hypothesis for Orofacial Pain Therapy
Yair Sharav, Rafael Benoliel, Yaron Haviv
Toxins.2025; 17(8): 389. CrossRef - Intranasal CRMP2-Ubc9 inhibitor regulates NaV1.7 to alleviate trigeminal neuropathic pain
Santiago I. Loya-Lopez, Heather N. Allen, Paz Duran, Aida Calderon-Rivera, Kimberly Gomez, Upasana Kumar, Rory Shields, Rui Zeng, Akshat Dwivedi, Saumya Saurabh, Olga A. Korczeniewska, Rajesh Khanna
Pain.2024; 165(3): 573. CrossRef - İMPLANT CERRAHİSİ SONRASI HİPOESTEZİ-6 AYLIK TAKİP: VAKA SERİSİ
Sefa AYDINDOĞAN, Emine Elif MUTAFCİLAR VELİOĞLU, Yunus Emre BALABAN
Selcuk Dental Journal.2023; 10(4): 350. CrossRef - Pathophysiology of Post-Traumatic Trigeminal Neuropathic Pain
Olga A. Korczeniewska, Divya Kohli, Rafael Benoliel, Sita Mahalakshmi Baddireddy, Eli Eliav
Biomolecules.2022; 12(12): 1753. CrossRef - Shape and anatomical relationship of the mental foramen to the mandibular premolars in an Indian sub-population: a retrospective CBCT analysis
Komal Sheth, Kulvinder Singh Banga, Ajinkya M. Pawar, James L. Gutmann, Hyeon-Cheol Kim
Restorative Dentistry & Endodontics.2022;[Epub] CrossRef - Trigeminal neuralgia and persistent idiopathic facial pain (atypical facial pain)
Gary W. Jay, Robert L. Barkin
Disease-a-Month.2022; 68(6): 101302. CrossRef - Differential roles of NMDAR subunits 2A and 2B in mediating peripheral and central sensitization contributing to orofacial neuropathic pain
Yan-Yan Zhang, Fei Liu, Zhong-Han Fang, Yue-Ling Li, Hong-Lin Liao, Qin-Xuan Song, Cheng Zhou, Jie-Fei Shen
Brain, Behavior, and Immunity.2022; 106: 129. CrossRef - Visualization of Inferior Alveolar and Lingual Nerve Pathology by 3D Double-Echo Steady-State MRI: Two Case Reports with Literature Review
Adib Al-Haj Husain, Daphne Schönegg, Silvio Valdec, Bernd Stadlinger, Thomas Gander, Harald Essig, Marco Piccirelli, Sebastian Winklhofer
Journal of Imaging.2022; 8(3): 75. CrossRef - Molecular mechanisms of painful traumatic trigeminal neuropathy—Evidence from animal research and clinical correlates
Olga A. Korczeniewska, Junad Khan, Eli Eliav, Rafael Benoliel
Journal of Oral Pathology & Medicine.2020; 49(6): 580. CrossRef - Behavioral changes in calves 11 days after cautery disbudding: Effect of local anesthesia
Sarah J.J. Adcock, Danielle M. Cruz, Cassandra B. Tucker
Journal of Dairy Science.2020; 103(9): 8518. CrossRef - Frequency of Lower Lip Paresthesia in Patients Receiving Implant-Supported Mandibular Dentures in Tabriz, Iran in 2017-2018
Farrokh Farhadi, Reza Khorshidi-Khiavi, Fereshteh Taheri, Milad Ghanizadeh
Avicenna Journal of Dental Research.2019; 11(1): 26. CrossRef - Persistent idiopathic facial pain
Rafael Benoliel, Charly Gaul
Cephalalgia.2017; 37(7): 680. CrossRef - Painful Traumatic Trigeminal Neuropathy
Rafael Benoliel, Sorin Teich, Eli Eliav
Oral and Maxillofacial Surgery Clinics of North America.2016; 28(3): 371. CrossRef - Neuropathy of Trigeminal Nerve Branches After Oral and Maxillofacial Treatment
Jimoh Olubanwo Agbaje, Elke Van de Casteele, Marjolein Hiel, Ciska Verbaanderd, Ivo Lambrichts, Constantinus Politis
Journal of Maxillofacial and Oral Surgery.2016; 15(3): 321. CrossRef - The Enigma of the Mental Foramen as It Relates to Plastic Surgery
Raphael Alves Chu, Fabio Xerfan Nahas, Marcello Di Martino, Fernanda Abibi Soares, Neil Ferreira Novo, Ricardo Luiz Smith, Lydia Masako Ferreira
Journal of Craniofacial Surgery.2014; 25(1): 238. CrossRef - Mental nerve paresthesia secondary to initiation of endodontic therapy: a case report
Syed Mukhtar-Un-Nisar Andrabi, Sharique Alam, Afaf Zia, Masood Hasan Khan, Ashok Kumar
Restorative Dentistry & Endodontics.2014; 39(3): 215. CrossRef - Pain Sensation and Postsurgical Complications in Posterior Mandibular Implant Placement Using Ridge Mapping, Panoramic Radiography, and Infiltration Anesthesia
Ali Saad Thafeed AlGhamdi
ISRN Dentistry.2013; 2013: 1. CrossRef
- Botulinum Toxin-A, Generating a Hypothesis for Orofacial Pain Therapy
- 2,031 View
- 7 Download
- 17 Crossref


 KACD
KACD

 First
First Prev
Prev


