Search
- Page Path
- HOME > Search
- Dentin thickness of C-shaped root canal walls in mandibular premolars based on cone-beam computed tomography: a retrospective cross-sectional study
- Elif Aslan, Ali Canberk Ulusoy, Bilge Hakan Sen, B. Guniz Baksi, Erinc Onem, Ali Mert
- Restor Dent Endod 2025;50(2):e18. Published online May 15, 2025
- DOI: https://doi.org/10.5395/rde.2025.50.e18
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Objectives
This study aimed to measure the dentin thickness of C-shaped canals in mandibular first and second premolars at coronal, middle, and apical root levels using cone-beam computed tomography (CBCT).
Methods
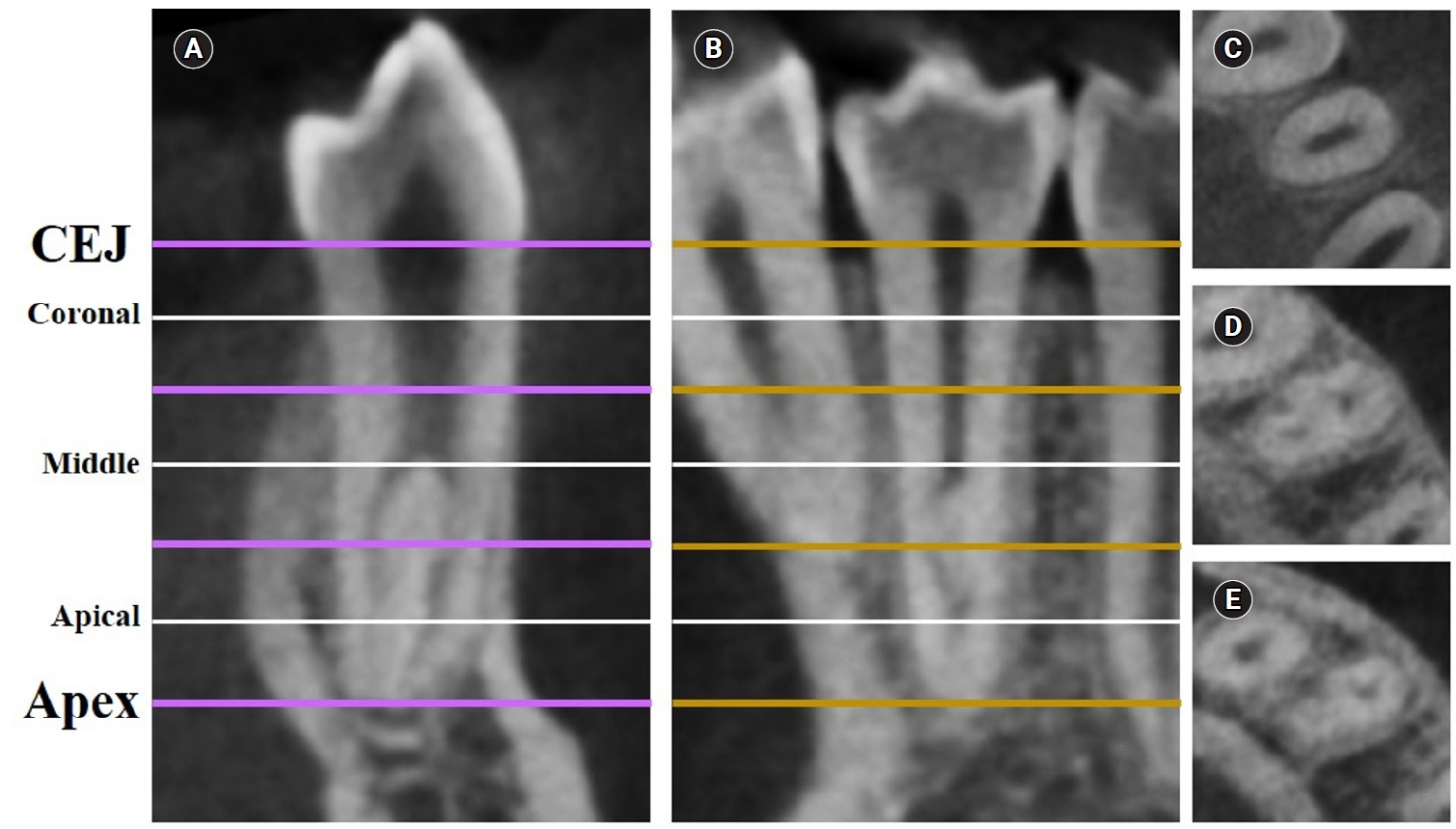
Dentin thicknesses of buccal, lingual, mesial, and distal root walls of 41 C-shaped premolars were measured at three different root levels on axial CBCT slices. The measurements were made at the midpoint of each third, along with 1 mm below and above the midpoint. C-shape configurations of the premolar root canals were also recorded. Analysis of variance, Kruskal-Wallis, and the independent samples t-tests were used for the comparisons (p = 0.05).
Results
The thickest walls for both premolars were buccal and lingual walls at all three root levels (p < 0.05). The thinnest walls for the first premolar teeth were mesial and distal walls of the lingual canal, while it was the mesial end of the buccal and lingual canals for the second premolars (p < 0.05). Dentin wall thicknesses at the mesial end of buccal and lingual canals of C1-shaped first premolars were thinner than C2-shaped first premolars at the apical level (p < 0.05).
Conclusions
Danger zones for C-shaped mandibular first and second premolars are predominantly mesial walls facing the radicular groove and distal wall of the lingual canal. CBCT imaging during endodontic treatment is recommended to avoid complications. -
Citations
Citations to this article as recorded by- Anatomical complexity in mandibular second molars: prevalence of C-shaped canals, radicular grooves, taurodontism, and radices molarum in Saudi population
Ahmed A. Madfa, Abdullah F. Alshammari, Eyad Almagadawyi, Ebtsam A. Aledaili, Afaf Al-Haddad
Scientific Reports.2025;[Epub] CrossRef
- Anatomical complexity in mandibular second molars: prevalence of C-shaped canals, radicular grooves, taurodontism, and radices molarum in Saudi population
- 3,556 View
- 135 Download
- 1 Web of Science
- 1 Crossref

- Predictor factors of 1-rooted mandibular second molars on complicated root and canal anatomies of other mandibular teeth
- Hakan Aydın, Hatice Harorlı
- Restor Dent Endod 2024;49(1):e2. Published online January 3, 2024
- DOI: https://doi.org/10.5395/rde.2024.49.e2
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives This study aimed to determine the effects of 1-rooted mandibular second molar (MnSM) teeth on root canal anatomy complexities of the mandibular central incisor (MnCI), mandibular lateral incisor (MnLI), mandibular canine (MnCn), mandibular first premolar (MnFP), mandibular second premolar (MnSP), and mandibular first molar (MnFM) teeth.
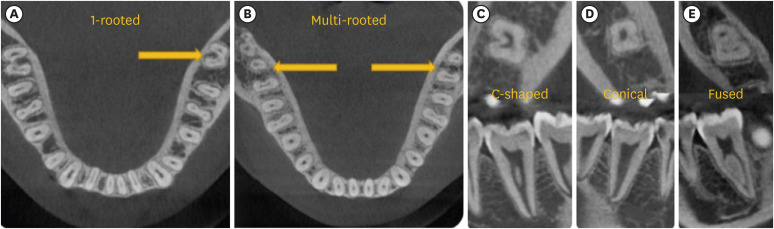
Materials and Methods Cone-beam computed tomography images of 600 patients with full lower dentition were examined. Individuals with 1-rooted MnSMs were determined, and the complexity of root canal anatomy of other teeth was compared with individuals without 1-rooted MnSMs (Group-1; subjects with at least one 1-rooted MnSM, Group-2; subjects with more than a single root in both MnSMs). A second canal in MnCIs, MnLIs, MnCns, MnFPs, and MnSPs indicated a complicated root canal. The presence of a third root in MnFMs was recorded as complicated.
Results The prevalence of 1-rooted MnSMs was 12.2%, with the C-shaped root type being the most prevalent (9%). There were fewer complicated root canals in MnCIs (
p = 0.02), MnLIs (p < 0.001), and MnFPs (p < 0.001) in Group 1. The other teeth showed no difference between the groups (p > 0.05). According to logistic regression analysis, 1-rooted right MnSMs had a negative effect on having complex canal systems of MnLIs and MnFPs. Left MnSMs were explanatory variables on left MnLIs and both MnFPs.Conclusions In individuals with single-rooted MnSMs, a less complicated root canal system was observed in all teeth except the MnFMs.
-
Citations
Citations to this article as recorded by- Repair of furcal perforations using different calcium silicate cements: An in vitro study
Ariana Esperanza Apolo Aguilar, Maria Soledad Peñaherrera Manosalvas, Henry Paul Valverde Haro
Journal of Conservative Dentistry and Endodontics.2025; 28(10): 1007. CrossRef
- Repair of furcal perforations using different calcium silicate cements: An in vitro study
- 1,927 View
- 62 Download
- 1 Crossref

- C-shaped root canals of mandibular second molars in a Korean population: a CBCT analysis
- Hee-Sun Kim, Daun Jung, Ho Lee, Yoon-Sic Han, Sohee Oh, Hye-Young Sim
- Restor Dent Endod 2018;43(4):e42. Published online November 1, 2018
- DOI: https://doi.org/10.5395/rde.2018.43.e42
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives The purpose of this study was to investigate the C-shaped root canal anatomy of mandibular second molars in a Korean population.
Materials and Methods A total of 542 teeth were evaluated using cone-beam computed tomography (CBCT). The canal shapes were classified according to a modified version of Melton's method at the level where the pulp chamber floor became discernible.
Results Of the 542 mandibular second molars, 215 (39.8%) had C-shaped canals, 330 (53%) had 3 canals, 17 (3.3%) had 2 canals, 12 (2.2%) had 4 canals, and 8 (1.7%) had 1 canal. The prevalence of C-shaped canals was 47.8% in females and 28.4% in males. Seventy-seven percent of the C-shaped canals showed a bilateral appearance. The prevalence of C-shaped canals showed no difference according to age or tooth position. Most teeth with a C-shaped canal system presented Melton's type II (45.6%) and type III (32.1%) configurations.
Conclusions There was a high prevalence of C-shaped canals in the mandibular second molars of the Korean population studied. CBCT is expected to be useful for endodontic diagnosis and treatment planning of mandibular second molars.
-
Citations
Citations to this article as recorded by- A cone-beam computed tomography-based morphometric comparison of mandibular molars between Han Chinese and Malays
Jacob John, Wei Cheong Ngeow, Ting-Chun Shen, Lih-Jyh Fuh, Phrabhakaran Nambiar, Yen-Wen Shen, Jui-Ting Hsu
Journal of Dental Sciences.2026; 21(1): 265. CrossRef - Prevalence of C‐Shaped Canals in Maxillary Molars in an Iranian Population: A Cone‐Beam Computed Tomography Analysis
Amin Salem Milani, Shahin Namvar Asl Amirkhizi, Tahmineh Razi, Ahmad Nouroloyouni, Pouya Sabanik, Nikhat Kaura
International Journal of Clinical Practice.2026;[Epub] CrossRef - Evaluation of mandibular and maxillary second molar root canal anatomy in a Turkish subpopulation using CBCT: comparison of Briseno-Marroquin and Vertucci classifications
Hüseyin Gürkan Güneç, İpek Öreroğlu, Kemal Çağlar, Kader Cesur Aydin
BMC Medical Imaging.2025;[Epub] CrossRef - Dentin thickness of C-shaped root canal walls in mandibular premolars based on cone-beam computed tomography: a retrospective cross-sectional study
Elif Aslan, Ali Canberk Ulusoy, Bilge Hakan Sen, B. Guniz Baksi, Erinc Onem, Ali Mert
Restorative Dentistry & Endodontics.2025; 50(2): e18. CrossRef - Prevalence of c-shaped canal morphology in premolar and molar teeth assessed by cone-beam computed tomography: systematic review and meta-analysis
Faezeh Yousefi, Younes Mohammadi, Elham Shokri
BMC Oral Health.2025;[Epub] CrossRef - Anatomical complexity in mandibular second molars: prevalence of C-shaped canals, radicular grooves, taurodontism, and radices molarum in Saudi population
Ahmed A. Madfa, Abdullah F. Alshammari, Eyad Almagadawyi, Ebtsam A. Aledaili, Afaf Al-Haddad
Scientific Reports.2025;[Epub] CrossRef - Imaging Findings of Clinical Significance in Endodontics During Cone Beam Computed Tomography Scanning of the Upper Airway—The Anterior, Bilateral, C-Shaped, Dual of Mandibular Root Canals: A Brief Case Report
Edgar García-Torres, Diana Laura Grissel Guerrero-Falcón, Hugo Alejandro Bojórquez-Armenta, Oscar Eduardo Almeda-Ojeda, Víctor Hiram Barajas-Pérez, Luis Javier Solís-Martínez
Diagnostics.2025; 15(24): 3157. CrossRef - Frequency of C-Shaped Root Canals in Permanent Mandibular Second Molars in a Sample of Pakistani Population using Cone Beam Computed Tomography
Syed Nabeel Ahmed, Muhammad Mansoor Majeed, Sakina Kazmi, Muhammad Omar Ansari
Pakistan Journal of Health Sciences.2024; : 109. CrossRef - ANÁLISE DAS VARIAÇÕES ANATÔMICAS DE CANAIS C-SHAPED NOS MOLARES INFERIORES: UMA REVISÃO INTEGRATIVA DA LITERATURA
Larissa Eulália Pereira, Thayana Karla Guerra Lira dos Santos
Revista Contemporânea.2024; 4(5): e4264. CrossRef - External Validation of the Effect of the Combined Use of Object Detection for the Classification of the C-Shaped Canal Configuration of the Mandibular Second Molar in Panoramic Radiographs: A Multicenter Study
Sujin Yang, Kee-Deog Kim, Yoshitaka Kise, Michihito Nozawa, Mizuho Mori, Natsuho Takata, Akitoshi Katsumata, Yoshiko Ariji, Wonse Park, Eiichiro Ariji
Journal of Endodontics.2024; 50(5): 627. CrossRef - A Cone‐Beam Computed Tomography Evaluation of C‐Shaped Canal Configuration in Maxillary Molars Among an Iranian Population
Nafiseh Nikkerdar, Mohammad Moslehi, Amin Golshah, Mario Dioguardi
International Journal of Dentistry.2024;[Epub] CrossRef - Root and canal morphology of mandibular second molars in an Egyptian subpopulation: a cone-beam computed tomography study
Shehabeldin Mohamed Saber, Mohammed abou El Seoud, Shaimaa Mohamed Abu el Sadat, Nawar Naguib Nawar
BMC Oral Health.2023;[Epub] CrossRef - Comprehensive evaluation of root and root canal morphology of mandibular second molars in a Saudi subpopulation evaluated by cone-beam computed tomography
Moazzy I. Almansour, Saad M. Al‑Zubaidi, Abdulmjeed S. Enizy, Ahmed A. Madfa
BMC Oral Health.2022;[Epub] CrossRef - Assessment of C-Shaped Canal Morphology in Mandibular and Maxillary Second Molars in an Iraqi Subpopulation Using Cone-Beam Computed Tomography
Kazhan Abdalrahman, Ranjdar Talabani, Sara Kazzaz, Dlsoz Babarasul, Berndt Koslowski
Scanning.2022; 2022: 1. CrossRef - Cone-beam computed tomography evaluation of C-shaped root canal system in mandibular second molars in kuwaiti sub-population
AbdullahJassim Alenezi, Saad Al-Nazhan, Nassr Al-Maflehi, MazenA Aldosimani
Saudi Endodontic Journal.2022; 12(3): 283. CrossRef - Prevalence and morphology of C‐shaped and non‐C‐shaped root canal systems in mandibular second molars
T Fenelon, P Parashos
Australian Dental Journal.2022;[Epub] CrossRef - Evaluation of C-shaped canals in mandibular second molars of a selected patient group using cone beam computed tomography: prevalence, configuration and radicular groove types
Sema Sönmez Kaplan, Tuna Kaplan, Güzide Pelin Sezgin
Odontology.2021; 109(4): 949. CrossRef - Prevalência estimada de canais “C- Shaped”: Uma revisão sistemática e meta-análise
Natália Pereira da Silva Falcão, Sandro Junio de Oliveira Tavares, Ludmila Silva Guimarães, Katherine Azevedo Batistela Rodrigues Thuller, Leonardo dos Santos Antunes, Estefano Borgo Sarmento, Fellipe Navarro Azevedo de Azevedo, Cinthya Cristina Gomes, Ca
Revista Científica Multidisciplinar Núcleo do Conhecimento.2020; : 91. CrossRef - Preferred Reporting Items for Epidemiologic Cross-sectional Studies on Root and Root Canal Anatomy Using Cone-beam Computed Tomographic Technology: A Systematized Assessment
Jorge N.R. Martins, Anil Kishen, Duarte Marques, Emmanuel João Nogueira Leal Silva, João Caramês, António Mata, Marco A. Versiani
Journal of Endodontics.2020; 46(7): 915. CrossRef - Clinical and radiological assessment of the anatomical and topographic structure of the root canals of teeth in patients of different age groups
N.B. Petrukhina, O.A. Zorina, O.A. Boriskina, I.S. Berkutova, V.A. Venediktova, R.R. Saltovets
Stomatologiya.2020; 99(5): 32. CrossRef
- A cone-beam computed tomography-based morphometric comparison of mandibular molars between Han Chinese and Malays
- 2,353 View
- 13 Download
- 20 Crossref

- Healing outcomes of root canal treatment for C-shaped mandibular second molars: a retrospective analysis
- Hye-Ra Ahn, Young-Mi Moon, Sung-Ok Hong, Min-Seock Seo
- Restor Dent Endod 2016;41(4):262-270. Published online August 29, 2016
- DOI: https://doi.org/10.5395/rde.2016.41.4.262
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives This study aimed to evaluate the healing rate of non-surgical endodontic treatment between C-shaped and non-C-shaped mandibular second molars.
Materials and Methods Clinical records and radiological images of patients who had undergone endodontic treatment on mandibular second molars between 2007 and 2014 were screened. The periapical index scoring system was applied to compare healing outcomes. Information about preoperative and postoperative factors as well as the demographic data of the patients was acquired and evaluated using chi-square and multinomial logistic regression tests.
Results The total healing rate was 68.4%. Healing rates for the mandibular second molar were 70.9% in C-shaped canals (
n = 79) and 66.6% in non-C-shaped ones (n = 117). The difference was not statistically significant.Conclusions The presence of a C-shaped canal in the mandibular second molar did not have a significantly negative effect on healing after treatment. Instead, proper pulpal diagnosis and final restoration were indicated as having significantly greater influence on the healing outcomes of C-shaped and non-C-shaped canals, respectively.
-
Citations
Citations to this article as recorded by- Predicting early endodontic treatment failure following primary root canal treatment
Young-Eun Jang, Yemi Kim, Sin-Young Kim, Bom Sahn Kim
BMC Oral Health.2024;[Epub] CrossRef - Factors Influencing Non-Surgical Root Canal Treatment Outcomes in Mandibular Second Molars: A Retrospective Cone-Beam Computed Tomography Analysis
Da-Min Park, Woo-Hyun Seok, Ji-Young Yoon
Journal of Clinical Medicine.2024; 13(10): 2931. CrossRef - Retrospective Assessment of Healing Outcome of Endodontic Treatment for Mandibular Molars with C-shaped Root Canal
Kishore Kumar Majety, Basanta Kumar Choudhury, Anika Bansal, Achla Sethi, Jaina Panjabi
The Journal of Contemporary Dental Practice.2017; 18(7): 591. CrossRef
- Predicting early endodontic treatment failure following primary root canal treatment
- 1,939 View
- 20 Download
- 3 Crossref

- Analysis of C-shaped root canal configuration in maxillary molars in a Korean population using cone-beam computed tomography
- Hyoung-Hoon Jo, Jeong-Bum Min, Ho-Keel Hwang
- Restor Dent Endod 2016;41(1):55-62. Published online January 29, 2016
- DOI: https://doi.org/10.5395/rde.2016.41.1.55
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives The purpose of this study was to investigate the incidence of root fusion and C-shaped root canals in maxillary molars, and to classify the types of C-shaped canal by analyzing cone-beam computed tomography (CBCT) in a Korean population.
Materials and Methods Digitized CBCT images from 911 subjects were obtained in Chosun University Dental Hospital between February 2010 and July 2012 for orthodontic treatment. Among them, a total of selected 3,553 data of maxillary molars were analyzed retrospectively. Tomography sections in the axial, coronal, and sagittal planes were displayed by PiViewstar and Rapidia MPR software (Infinitt Co.). The incidence and types of root fusion and C-shaped root canals were evaluated and the incidence between the first and the second molar was compared using Chi-square test.
Results Root fusion was present in 3.2% of the first molars and 19.5% of the second molars, and fusion of mesiobuccal and palatal root was dominant. C-shaped root canals were present in 0.8% of the first molars and 2.7% of the second molars. The frequency of root fusion and C-shaped canal was significantly higher in the second molar than the first molar (
p < 0.001).Conclusions In a Korean population, maxillary molars showed total 11.3% of root fusion and 1.8% of C-shaped root canals. Furthermore, root fusion and C-shaped root canals were seen more frequently in the maxillary second molars.
-
Citations
Citations to this article as recorded by- Prevalence of C‐Shaped Canals in Maxillary Molars in an Iranian Population: A Cone‐Beam Computed Tomography Analysis
Amin Salem Milani, Shahin Namvar Asl Amirkhizi, Tahmineh Razi, Ahmad Nouroloyouni, Pouya Sabanik, Nikhat Kaura
International Journal of Clinical Practice.2026;[Epub] CrossRef - Prevalence of c-shaped canal morphology in premolar and molar teeth assessed by cone-beam computed tomography: systematic review and meta-analysis
Faezeh Yousefi, Younes Mohammadi, Elham Shokri
BMC Oral Health.2025;[Epub] CrossRef - A Cone‐Beam Computed Tomography Evaluation of C‐Shaped Canal Configuration in Maxillary Molars Among an Iranian Population
Nafiseh Nikkerdar, Mohammad Moslehi, Amin Golshah, Mario Dioguardi
International Journal of Dentistry.2024;[Epub] CrossRef - Endodontic treatment of a C‐shaped mandibular second molar with narrow dentinal thickness: A case report
Mina Mehrjouei, Hamid Jafarzadeh, Pourya Esmaeelpour, Maryam Khorasanchi
Clinical Case Reports.2024;[Epub] CrossRef - Evaluation of 2- and 3-dimensional anatomic parameters of C-shaped root canals with cone beam computed tomography, microcomputed tomography, and nanocomputed tomography
Miguel Angel Ventura Molina, Giovane Oliveira Silva, Amanda Pelegrin Candemil, Rafael Verardino de Camargo, Ruben Pauwels, Reinhilde Jacobs, Manoel Damião Sousa-Neto, Jardel Francisco Mazzi-Chaves
Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology.2023; 136(6): 759. CrossRef - Cone-Beam Computed Tomography (CBCT) Analysis of an Unusual Configuration of the Upper First Molar With a C-shaped Canal With Apically Fused Roots: A Case Report
Kapil D Wahane, Anand V Bansod, Sudha mattigatti, Rushikesh Mahaparale, Yuvraj B Rote, Mayur B Wanjari
Cureus.2023;[Epub] CrossRef - Assessment of C-Shaped Canal Morphology in Mandibular and Maxillary Second Molars in an Iraqi Subpopulation Using Cone-Beam Computed Tomography
Kazhan Abdalrahman, Ranjdar Talabani, Sara Kazzaz, Dlsoz Babarasul, Berndt Koslowski
Scanning.2022; 2022: 1. CrossRef - Root and canal-specific features of maxillary first molars with fused roots
Katarina Beljic-Ivanovic, Branislav Karadzic
Vojnosanitetski pregled.2022; 79(11): 1092. CrossRef - Diagnosis and treatment of maxillary molar with abnormality
Kkot-Byeol Bae, Bin-Na Lee, Hoon-Sang Chang, In-Nam Hwang, Won-Mann Oh, Yun-Chan Hwang
Oral Biology Research.2022; 46(4): 195. CrossRef - Endodontic treatment of the maxillary first molar with palatal canal variations: A case report and review of literature
Kai Chen, Xing Ran, Yan Wang
World Journal of Clinical Cases.2022; 10(32): 12036. CrossRef - Evaluation of C-shaped canals in maxillary molars in a Chinese population using CBCT
Yuyan Qian, Yamei Li, Jukun Song, Ping Zhang, Zhu Chen
BMC Medical Imaging.2022;[Epub] CrossRef - Comprehensive evaluation of root and root canal morphology of mandibular second molars in a Saudi subpopulation evaluated by cone-beam computed tomography
Moazzy I. Almansour, Saad M. Al‑Zubaidi, Abdulmjeed S. Enizy, Ahmed A. Madfa
BMC Oral Health.2022;[Epub] CrossRef - Evaluation of C-shaped canal configuration in maxillary molars: A retrospective cone-beam computed tomography study
Emre KÖSE, Rüya AK
Clinical and Experimental Health Sciences.2021; 11(3): 444. CrossRef - Maxillary First Molars with Two Palatal Root Canals
Kun-Hwa Sung, Ho-Keel Hwang, Hyoung-Hoon Jo, Konstantinos Michalakis
Case Reports in Dentistry.2021;[Epub] CrossRef - Preferred Reporting Items for Epidemiologic Cross-sectional Studies on Root and Root Canal Anatomy Using Cone-beam Computed Tomographic Technology: A Systematized Assessment
Jorge N.R. Martins, Anil Kishen, Duarte Marques, Emmanuel João Nogueira Leal Silva, João Caramês, António Mata, Marco A. Versiani
Journal of Endodontics.2020; 46(7): 915. CrossRef - Evaluation of root and root canal morphology of elderly Korean patients maxillary molars using cone-beam computed tomography
Tae-Yong Lee, Mi-Yeon Kim, Sun-Ho Kim, Jeong-Hee Kim
The Journal of Korean Academy of Prosthodontics.2020; 58(2): 95. CrossRef - Second mesiobuccal root canal in maxillary molars—A systematic review and meta-analysis of prevalence studies using cone beam computed tomography
Jorge N.R. Martins, Duarte Marques, Emmanuel João Nogueira Leal Silva, João Caramês, António Mata, Marco A. Versiani
Archives of Oral Biology.2020; 113: 104589. CrossRef - Prevalência estimada de canais “C- Shaped”: Uma revisão sistemática e meta-análise
Natália Pereira da Silva Falcão, Sandro Junio de Oliveira Tavares, Ludmila Silva Guimarães, Katherine Azevedo Batistela Rodrigues Thuller, Leonardo dos Santos Antunes, Estefano Borgo Sarmento, Fellipe Navarro Azevedo de Azevedo, Cinthya Cristina Gomes, Ca
Revista Científica Multidisciplinar Núcleo do Conhecimento.2020; : 91. CrossRef - Evaluation of the internal anatomy of paramolar tubercles using cone-beam computed tomography
G. Colakoglu, I. Kaya Buyukbayram, M. A. Elcin, M. Kazak, H. Sezer
Surgical and Radiologic Anatomy.2020; 42(1): 15. CrossRef - Analysis of Prevalence of Pyramidal Molars in Adolescent
Woojin Kwon, Hyung-Jun Choi, Jaeho Lee, Je Seon Song
THE JOURNAL OF THE KOREAN ACADEMY OF PEDTATRIC DENTISTRY.2020; 47(4): 389. CrossRef - Prevalence Studies on Root Canal Anatomy Using Cone-beam Computed Tomographic Imaging: A Systematic Review
Jorge N.R. Martins, Duarte Marques, Emmanuel João Nogueira Leal Silva, João Caramês, Marco A. Versiani
Journal of Endodontics.2019; 45(4): 372. CrossRef - Fused roots of maxillary molars: characterization and prevalence in a Latin American sub-population: a cone beam computed tomography study
Maytté Marcano-Caldera, Jose Luis Mejia-Cardona, María del Pilar Blanco-Uribe, Elena Carolina Chaverra-Mesa, Didier Rodríguez-Lezama, Jose Hernán Parra-Sánchez
Restorative Dentistry & Endodontics.2019;[Epub] CrossRef - An original micro‐CT study and meta‐analysis of the internal and external anatomy of maxillary molars—implications for endodontic treatment
Iwona M. Tomaszewska, Anna Jarzębska, Bendik Skinningsrud, Przemysław A. Pękala, Sebastian Wroński, Joe Iwanaga
Clinical Anatomy.2018; 31(6): 838. CrossRef - A Cone-beam Computed Tomographic Study of Root and Canal Morphology of Maxillary First and Second Permanent Molars in a Thai Population
Roserin Ratanajirasut, Anchana Panichuttra, Soontra Panmekiate
Journal of Endodontics.2018; 44(1): 56. CrossRef - Retrospective Assessment of Healing Outcome of Endodontic Treatment for Mandibular Molars with C-shaped Root Canal
Kishore Kumar Majety, Basanta Kumar Choudhury, Anika Bansal, Achla Sethi, Jaina Panjabi
The Journal of Contemporary Dental Practice.2017; 18(7): 591. CrossRef - The morphology of maxillary first and second molars analyzed by cone-beam computed tomography in a polish population
Katarzyna Olczak, Halina Pawlicka
BMC Medical Imaging.2017;[Epub] CrossRef
- Prevalence of C‐Shaped Canals in Maxillary Molars in an Iranian Population: A Cone‐Beam Computed Tomography Analysis
- 1,916 View
- 14 Download
- 26 Crossref

- Endodontic treatment of a C-shaped mandibular second premolar with four root canals and three apical foramina: a case report
- Thikamphaa Bertrand, Sahng Gyoon Kim
- Restor Dent Endod 2016;41(1):68-73. Published online January 19, 2016
- DOI: https://doi.org/10.5395/rde.2016.41.1.68
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
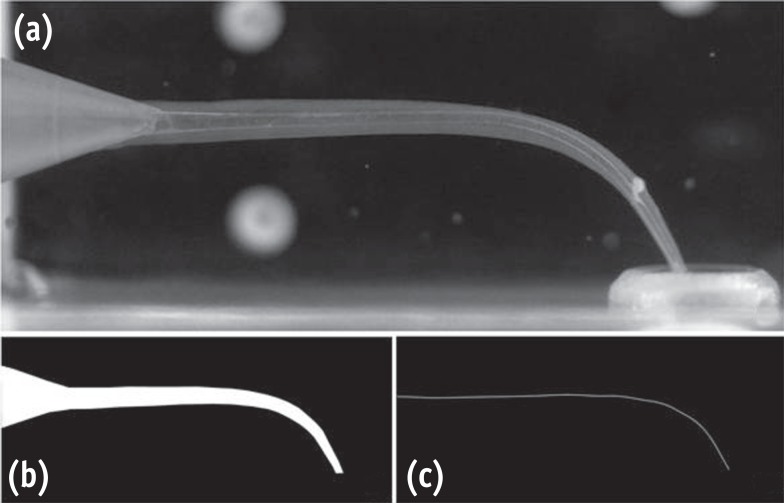
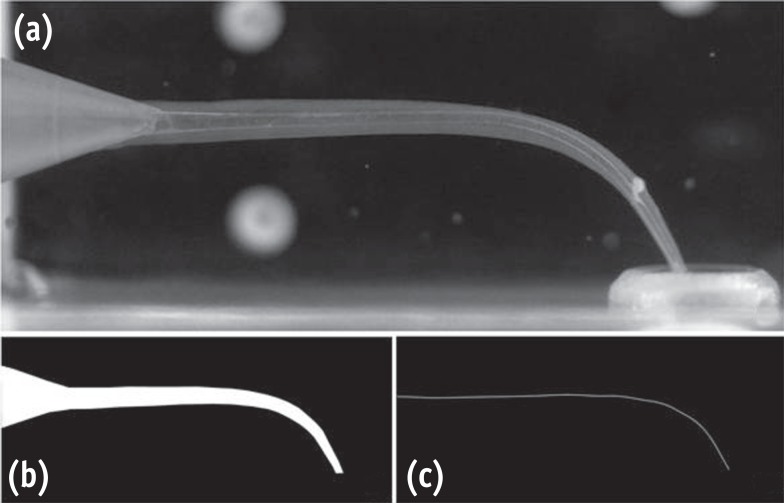
ePub This case report describes a unique C-shaped mandibular second premolar with four canals and three apical foramina and its endodontic management with the aid of cone-beam computer tomography (CBCT). C-shaped root canal morphology with four canals was identified under a dental operating microscope. A CBCT scan was taken to evaluate the aberrant root canal anatomy and devise a better instrumentation strategy based on the anatomy. All canals were instrumented to have a 0.05 taper using 1.0 mm step-back filing with appropriate apical sizes determined from the CBCT scan images and filled using a warm vertical compaction technique. A C-shaped mandibular second premolar with multiple canals is an anatomically rare case for clinicians, yet its endodontic treatment may require a careful instrumentation strategy due to the difficulty in disinfecting the canals in the thin root area without compromising the root structure.
-
Citations
Citations to this article as recorded by- Unique root anatomy of mandibular second premolars: clinical strategies for effective disinfection and preservation of dentine structure in root canal treatment—a case report
Ji Wook Jeong, Erika Silguero Gonzalez, Scott R. Makins, Timothy Kirkpatrick
Frontiers in Dental Medicine.2024;[Epub] CrossRef - PRICE 2020 guidelines for reporting case reports in Endodontics: explanation and elaboration
V. Nagendrababu, B. S. Chong, P. McCabe, P. K. Shah, E. Priya, J. Jayaraman, S. J. Pulikkotil, P. M. H. Dummer
International Endodontic Journal.2020; 53(7): 922. CrossRef - A cone-beam computed tomography study of C-shaped root canal systems in mandibular second premolars in a Taiwan Chinese subpopulation
Yi-Chin Chen, Chia-Lun Tsai, Yi-Chen Chen, Gin Chen, Shue-Fen Yang
Journal of the Formosan Medical Association.2018; 117(12): 1086. CrossRef - Anatomic Comparison of Contralateral Premolars
Gaute Floer Johnsen, Sazan Dara, Sameenah Asjad, Pia Titterud Sunde, Håvard Jostein Haugen
Journal of Endodontics.2017; 43(6): 956. CrossRef - Endodontic Management of Dilacerated Maxillary Central Incisor fused to a Supernumerary Tooth using Cone Beam Computed Tomography: An Unusual Clinical Presentation
Thilla S Vinothkumar, Deivanayagam Kandaswamy, Ganesh Arathi, Sathishkumar Ramkumar, Gnanasekaran Felsypremila
The Journal of Contemporary Dental Practice.2017; 18(6): 522. CrossRef
- Unique root anatomy of mandibular second premolars: clinical strategies for effective disinfection and preservation of dentine structure in root canal treatment—a case report
- 2,752 View
- 15 Download
- 5 Crossref

- Use of cone-beam computed tomography and three-dimensional modeling for assessment of anomalous pulp canal configuration: a case report
- Alper Sinanoglu, Dilek Helvacioglu-Yigit, Ibrahim Mutlu
- Restor Dent Endod 2015;40(2):161-165. Published online December 4, 2014
- DOI: https://doi.org/10.5395/rde.2015.40.2.161
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Three-dimensional (3D) reconstruction of cone-beam computed tomography (CBCT) scans appears to be a valuable method for assessing pulp canal configuration. The aim of this report is to describe endodontic treatment of a mandibular second premolar with aberrant pulp canal morphology detected by CBCT and confirmed by 3D modeling. An accessory canal was suspected during endodontic treatment of the mandibular left second premolar in a 21 year old woman with a chief complaint of pulsating pain. Axial cross-sectional CBCT scans revealed that the pulp canal divided into mesiobuccal, lingual, and buccal canals in the middle third and ended as four separate foramina. 3D modeling confirmed the anomalous configuration of the fused root with a deep lingual groove. Endodontic treatment of the tooth was completed in two appointments. The root canals were obturated using lateral compaction of gutta-percha and root canal sealer. The tooth remained asymptomatic and did not develop periapical pathology until 12 months postoperatively. CBCT and 3D modeling enable preoperative evaluation of aberrant root canal systems and facilitate endodontic treatment.
-
Citations
Citations to this article as recorded by- Exploring Technological Progress in Three-Dimensional Imaging for Root Canal Treatments: A Systematic Review
Kanwalpreet Kaur, Ravinder S. Saini, Sunil Kumar Vaddamanu, Shashit Shetty Bavabeedu, Vishwanath Gurumurthy, Shan Sainudeen, Vinod Babu Mathew, Shafait Ullah Khateeb, Aida Mokhlesi, Seyed Ali Mosaddad, Artak Heboyan
International Dental Journal.2025; 75(2): 1097. CrossRef - Root Canal Treatment of Oehlers Type III Dens Invaginatus in Maxillary Lateral Incisor and Remote Sinus Tract Using Dental Surgical Microscope and Cone-Beam Computed Tomography
Rie Fujii, Tomohiro Asai, Masashi Yamada, Ryo Sako, Yoshiki Tamiya, Masahiro Furusawa
The Bulletin of Tokyo Dental College.2023; 64(2): 67. CrossRef - CBCT and Micro-CT analysis of the mandibular first premolars with C-shaped canal system in a Chinese population author
Yimeng Zhang, Xunben Weng, Yu Fu, Xuekai Qi, Yihuai Pan, Yu Zhao
BMC Oral Health.2023;[Epub] CrossRef
- Exploring Technological Progress in Three-Dimensional Imaging for Root Canal Treatments: A Systematic Review
- 1,428 View
- 9 Download
- 3 Crossref

- Endodontic management of a C-shaped maxillary first molar with three independent buccal root canals by using cone-beam computed tomography
- Lorena Karanxha, Hee-Jin Kim, Sung-Ok Hong, Wan Lee, Pyung-Sik Kim, Kyung-San Min
- Restor Dent Endod 2012;37(3):175-179. Published online August 29, 2012
- DOI: https://doi.org/10.5395/rde.2012.37.3.175
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub The aim of this study was to present a method for endodontic management of a maxillary first molar with unusual C-shaped morphology of the buccal root verified by cone-beam computed tomography (CBCT) images. This rare anatomical variation was confirmed using CBCT, and nonsurgical endodontic treatment was performed by meticulous evaluation of the pulpal floor. Posttreatment image revealed 3 independent canals in the buccal root obturated efficiently to the accepted lengths in all 3 canals. Our study describes a unique C-shaped variation of the root canal system in a maxillary first molar, involving the 3 buccal canals. In addition, our study highlights the usefulness of CBCT imaging for accurate diagnosis and management of this unusual canal morphology.
-
Citations
Citations to this article as recorded by- Nonsurgical endodontic retreatment of C-shaped maxillary molars: case reports and review of literature
Ming Liu, Yanling Huang, Yixuan Wu, Yi Zhang, Zhisheng Zhang, Qianju Wu
BMC Oral Health.2024;[Epub] CrossRef - Analysis of Fused Rooted Maxillary First and Second Molars with Merged and C-shaped Canal Configurations: Prevalence, Characteristics, and Correlations in a Saudi Arabian Population
Mohammed Mashyakhy, Hemant Ramesh Chourasia, Ahmad Jabali, Abdulmajeed Almutairi, Gianluca Gambarini
Journal of Endodontics.2019; 45(10): 1209. CrossRef - C-shaped root canals of mandibular second molars in a Korean population: a CBCT analysis
Hee-Sun Kim, Daun Jung, Ho Lee, Yoon-Sic Han, Sohee Oh, Hye-Young Sim
Restorative Dentistry & Endodontics.2018;[Epub] CrossRef - Prevalence and Characteristics of the Maxillary C-shaped Molar
Jorge N.R. Martins, António Mata, Duarte Marques, Craig Anderson, João Caramês
Journal of Endodontics.2016; 42(3): 383. CrossRef - Use of cone-beam computed tomography and three-dimensional modeling for assessment of anomalous pulp canal configuration: a case report
Alper Sinanoglu, Dilek Helvacioglu-Yigit, Ibrahim Mutlu
Restorative Dentistry & Endodontics.2015; 40(2): 161. CrossRef - Endodontic management of a mandibular second molar with radix entomolaris: a case report
Rosaline Hannah, Deivanayagam Kandaswamy, Nachimuthu Jayaprakash
Restorative Dentistry & Endodontics.2014; 39(2): 132. CrossRef
- Nonsurgical endodontic retreatment of C-shaped maxillary molars: case reports and review of literature
- 1,416 View
- 4 Download
- 6 Crossref

- A retrospective study of the intentionally replanted mandibular second molars with C-shaped root canal configurations
- Won-Jun Shon, Kee-Yeon Kum, Seung-Ho Baek, Woo-Cheol Lee
- J Korean Acad Conserv Dent 2011;36(1):19-25. Published online January 31, 2011
- DOI: https://doi.org/10.5395/JKACD.2011.36.1.19
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives The purpose of this retrospective study was to evaluate the success rate of intentionally replanted mandibular second molar with C-shaped canal configurations and to access the impact of preoperative periapical lesion on the success of intentional replantation procedure.
Materials and Methods This retrospective chart review study evaluated 52 intentionally replanted mandibular second molar teeth treated at Seoul National University Dental Hospital Department of Conservative Dentistry from January 2005 to December 2007. Seventeen teeth were lost for the follow-up, and another 6 teeth did not meet inclusion criteria of C-shaped root canal configurations. Healing outcome such as success, uncertain healing, and failure after follow-up was evaluated by clinical criteria and radiographs.
Results The overall success rate was 72.4% for the 29 intentionally replanted C-shaped mandibular second molars. The success rate of replanted teeth with preoperative periapical lesions was similar to that of replanted teeth which have no periapical lesions.
Conclusions Therefore, root canal treatment failure on C-shaped mandibular second molar can be predictably treated by intentional replantation regardless of the presence of periapical lesion.
- 1,228 View
- 6 Download

- A retrospective study on incidence of C-shaped canals in mandibular second molars
- Hee-Sun Kim
- J Korean Acad Conserv Dent 2009;34(4):346-349. Published online July 31, 2009
- DOI: https://doi.org/10.5395/JKACD.2009.34.4.346
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Mandibular second molars have many variations in canal configuration. Technical modifications in cleaning, shaping and obturation are required. The purpose of this study was to investigate the root canal anatomy of mandibular second molars. 86 teeth of 85 patients were accessed and evaluated with taking radiographs for working length determination. 27 teeth(31.4%) had C-shaped canals, 43 teeth(50%) had 3 canals, 11 teeth(12.7%) had 4 canals, 5 teeth(5.8%) had 2 canals. Incidence of C-shaped canal was 31.7% in male and 31.1% in female. 30.9% of left mandibular second molar and 31.8% of right mandibular second molar showed C-shaped canals.
- 791 View
- 1 Download

- A study on the C-shaped root canal system of mandibular second molar
- Dong-Gyun Lee, Jun-Mo Park, Ho-Keel Hwang
- J Korean Acad Conserv Dent 2007;32(4):335-342. Published online July 31, 2007
- DOI: https://doi.org/10.5395/JKACD.2007.32.4.335
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
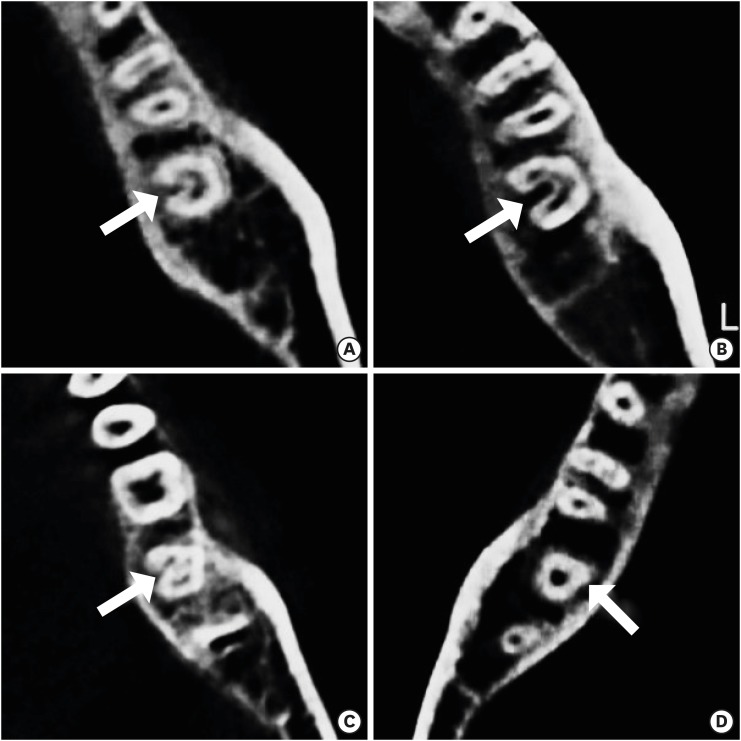
ePub C-shaped canals are known to present a complex canal anatomy with numerous fins connecting individual canals, thus requiring supplementary effort to accomplish a successful root canal treatment. This study examined the frequency of the C-shaped mandibular second molars and interrelation between the clinical records and radiographs to recognize them treated in the Department of Conservative Dentistry of the Chosun University Dental Hospital during a six-year period (1998 - 2004). This study reviewed the clinical records of 227 patients who underwent root canal treatment of the mandibular second molars. After opening the chamber, those cases with C-shaped orifices in the pulpal floor were selected, and the C-shaped root canal types were classified according to Melton's criteria. Three experienced dentists evaluated the radiographs of the C-shaped mandibular second molar on a viewer using a magnifying glass in order to determine if the root apex was fused or separated, the distal root canal was either centered or mesial shifted in the distal root, and if there was bilateral symmetry in a panorama. In conclusion, there is a high frequency of C-shaped mandibular second molars in Koreans. Simultaneous interpretation of the root shape and distal root canal using the preoperative, working length and post-treatment radiographs is important for diagnosing a C-shaped mandibular second molar.
-
Citations
Citations to this article as recorded by- An evaluation of canal curvature at the apical one third in type II mesial canals of mandibular molars
Hye-Rim Yun, Dong-Kyun Lee, Ho-Keel Hwang
Restorative Dentistry & Endodontics.2012; 37(2): 104. CrossRef - A retrospective study on incidence of C-shaped canals in mandibular second molars
Hee-Sun Kim
Journal of Korean Academy of Conservative Dentistry.2009; 34(4): 346. CrossRef
- An evaluation of canal curvature at the apical one third in type II mesial canals of mandibular molars
- 1,992 View
- 12 Download
- 2 Crossref

- Cross-sectional morphology and minimum canal wall widths in C-shaped root of mandibular molars
- Byung-Chul Song, Yong-Bum Cho
- J Korean Acad Conserv Dent 2007;32(1):37-46. Published online January 31, 2007
- DOI: https://doi.org/10.5395/JKACD.2007.32.1.037
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub The C-shaped canal system is an anatomical variation mostly seen in mandibular second molars, although it can also occur in maxillary and other mandibular molars. The main anatomical feature of C-shaped canals is the presence of fins or web connecting the individual root canals. The complexity of C-shaped canals prevents these canals from being cleaned, shaped, and obturated effectively during root canal therapy, and sometimes it leads to an iatrogenic perforation from the extravagant preparation.
The purpose of this study was to provide further knowledge of the anatomical configuration and the minimal thickness of dentinal wall according to the level of the root.
Thirty extracted mandibular second molars with fused roots and longitudinal grooves on lingual or buccal surface of the root were collected from a native Korean population. The photo images and radiographs from buccal, lingual, apical direction were taken. After access cavity was prepared, teeth were placed in 5.25% sodium hypochlorite solution for 2 hours to dissolve the organic tissue of the root surface and from the root canal system. After bench dried and all the teeth were embedded in a self-curing resin. Each block was sectioned using a microtome (Accutom-50, Struers, Denmark) at interval of 1 mm. The sectioned surface photograph was taken using a digital camera (Coolpix 995, Nikon, Japan) connected to the microscope. 197 images were evaluated for canal configurations and the minimal thickness of dentinal wall between canal and external wall using' Root Thickness Gauge Program' designed with Visual Basic.
The results were as follows:
1. At the orifice level of all teeth, the most frequent observed configuration was Melton's Type C I (73%), however the patterns were changed to type C II and C III when the sections were observed at the apical third. On the other hand, the type C III was observed at the orifice level of only 2 teeth but this type could be seen at apical region of the rest of the teeth.
2. The C-shaped canal showed continuous and semi-colon shape at the orifice level, but at the apical portion of the canal there was high possibility of having 2 or 3 canals.
3. Lingual wall was thinner than buccal wall at coronal, middle, apical thirds of root but there was no statistical differences.
- 936 View
- 1 Download


 KACD
KACD

 First
First Prev
Prev


