Abstract
This study describes the clinical steps taken in the treatment of a patient who had an avulsed right upper central incisor that presented with incomplete root development and chronic apical periodontitis. A 7-year-old boy was referred from a private dentist to a dental office specializing in endodontics. The tooth had remained in a dry environment for 20 minutes, and tooth replantation was performed at an emergency appointment. After clinical and radiographic examinations, root canal decontamination was performed, followed by several changes in intracanal calcium hydroxide medication. Blood clot formation was attempted, but bleeding within the root canal was insufficient; therefore, we opted for an intracanal medication change to stimulate mineralized tissue formation in the apical region. Root obturation was performed 45 days after the last change of intracanal medication, and clinical, radiographic, and tomographic follow-up examinations were performed at 3, 6, 18, and 40 months after the endodontic intervention. The increase in thickness and length of the root structure and the absence of root resorption were verified through follow-up examinations. Therefore, it was concluded that the procedures used were successful for tooth replantation.
-
Keywords: Tooth avulsion; Tooth replanted; Root canal treatment; Odontogenesis
INTRODUCTION
The incidence of dental trauma is relatively high [
1], and tooth avulsion is a common condition, affecting between 0.7% and 29.2% of the population [
1,
2]. Ideally, after tooth avulsion, the tooth should be replanted into the alveolus immediately [
1,
3], since limiting the extraoral dry time is crucial for maintaining the viability of the cells present inside the root canal and on the surface of the dental root [
4]. Moreover, the storage medium used during the extra-alveolar time and the process of tooth manipulation influence the prognosis of the involved tooth [
5,
6]. Under unfavorable conditions, undesirable consequences such as pulp necrosis, periodontal ligament degeneration, ankylosis, and root resorption may occur [
1,
3,
4,
5,
6].
The most appropriate treatment choice for a tooth also depends on whether it has a mature or an immature root and on the cellular condition of the periodontal ligament [
1,
3]. The cells of the periodontal ligament are classified after tooth avulsion based on the following 3 conditions: 1) they may be viable, if the tooth is replanted soon after the dental trauma (immediate replantation); 2) they may be partially damaged in situations when the tooth is stored in solutions such as saline or milk for a specific time; and 3) they may be infeasible, if the extra-alveolar time exceeds 30 minutes or if there are inadequate means to preserve the tooth. This type of replantation is called late replantation [
3].
In teeth with a mature root apex, endodontic treatment should be performed 7–10 days after tooth replantation, or even earlier in cases of late replantation [
3], when the avulsed tooth has incomplete rhizogenesis, the pulp tissue might undergo revascularization in cases of immediate replantation [
1,
3]. If revascularization does not occur, or in cases of late replantation, endodontic treatment should be performed [
3]. Apexification is traditionally the treatment of choice for the non-vital pulp of teeth with incomplete rhizogenesis in cases of replantation. This treatment consists of successive changes of intracanal calcium hydroxide-based medications, which promote apical closure without adding root length or dentinal thickness [
7]. However, teeth subjected to this treatment may be susceptible to root fracture, after which they may be lost [
7]. Due to these unfavorable results and recent advances in biotechnology, pulp revascularization has recently been developed as a therapeutic approach that is capable of inducing new tissue formation [
8].
In order to perform pulp revascularization, the root canal is decontaminated using an irrigation solution, followed by the application of intracanal medication, which may be calcium hydroxide paste or triple antibiotic paste [
8,
9]. In a subsequent session, the region is periapically stimulated, which should promote a blood clot that eventually fills the entire root canal. The clot provides a matrix rich in growth factors such as platelet and vascular endothelial derivatives, promoting the differentiation of stem cells and providing an environment conducive to cell growth, adhesion, and migration [
8,
9]. These undifferentiated cells, stimulated by the presence of a biomaterial, contribute to root development, including an increase in length and root thickness and apical closure in immature necrotic teeth. This process promotes tissue regeneration of the periodontal ligament, cementum, bone, and dentin to restore the functional properties of the tooth [
10,
11].
For successful revascularization in immature or permanent teeth with pulp necrosis, 3 challenges must be overcome: 1) disinfection of the root canal; 2) preparation of adequate tissue inside the root canal; and 3) satisfactory coronary sealing [
12]. To determine clinical success, the patient should be monitored for a period of up to 4 years [
8,
12]. The goals of the treatment are absence of clinical symptoms and radicular complementation with an increase in length and thickness [
8].
This study aimed to describe the clinical management of a pediatric patient with an avulsed right upper central incisor that presented with an immature root apex and chronic apical periodontitis.
CASE REPORT
A 7-year-old boy accompanied by his parents was referred to the department of endodontics at our institution by a private dentist, who had initially cared for the patient. As reported, the patient's right upper central incisor was avulsed while playing with his sister in a hammock. After communicating with the patient's father, who was at work near the family's residence, the boy was taken to the private dental office within 20 minutes. The avulsed tooth was kept dry. The dentist performed immediate replantation with the following protocol: 1) local anesthesia (Mepiadre 2%, DFL, Taquara, RJ, Brazil); 2) irrigation of the socket and avulsed tooth with saline; 3) tooth replantation; 4) semi-rigid orthodontic retention with photopolymerizable composite resin; 5) antibiotic prescription (amoxicillin; 250 mg, 5 mL every 8 hours for 7 days); 6) an analgesic (Alivium [ibuprofen]; 20 drops every 8 hours); 7) a tetanus vaccination assessment; and 8) resting orientation. The total extra-alveolar time between tooth avulsion and replantation was less than 30 minutes. The dentist responsible for the care referred the patient to an endodontic specialist.
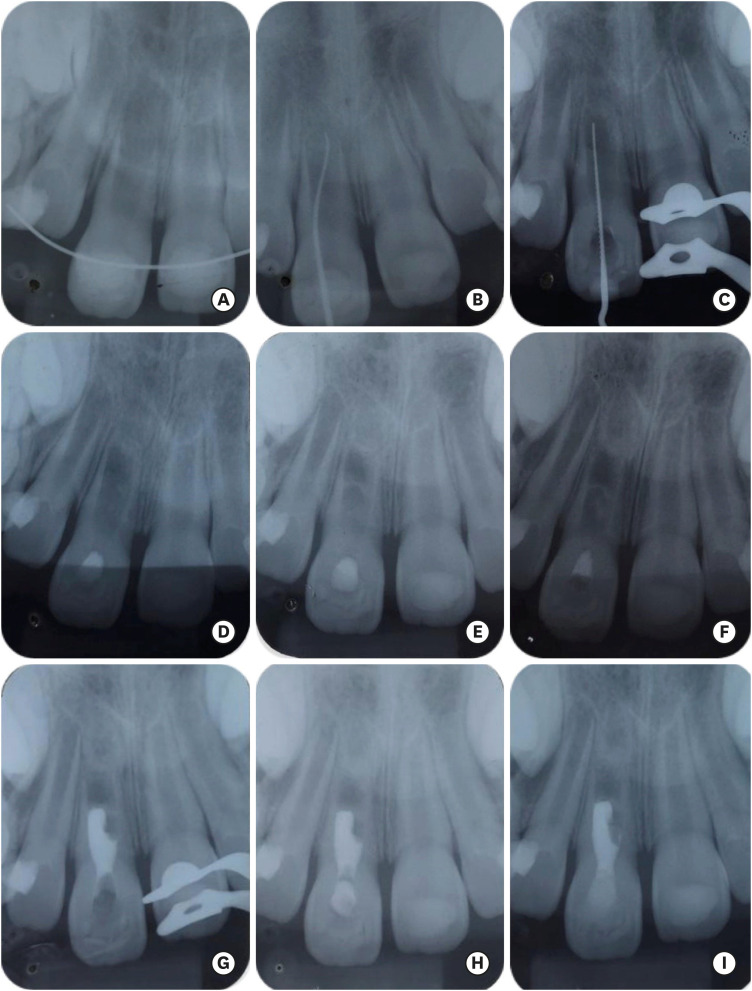
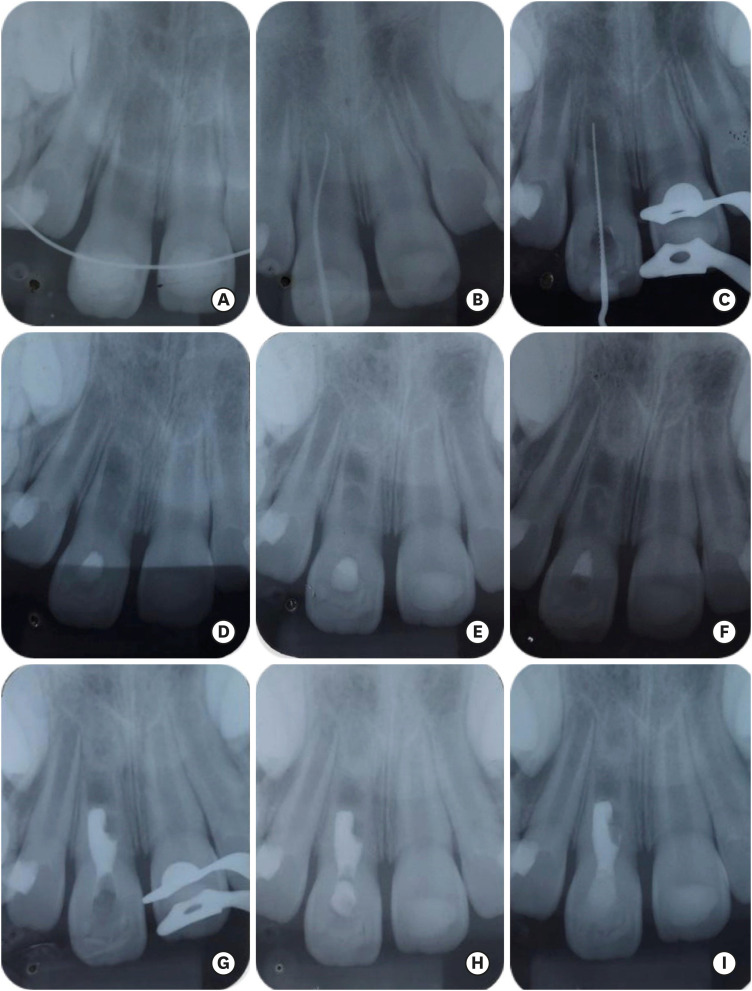
After 3 days, the endodontist noted that the tooth was positioned with the incisal edge level inconsistent with the adjacent teeth; endodontic tests and radiographic examinations were performed, and a positive response to the cold test and incomplete rhizogenesis in tooth 11 were verified (
Figure 1A). After initial analysis and verification that there were no other complications such as pain, pulp necrosis, and root fracture, it was decided to remove the semi-rigid splint after 15 days and to continue clinical and radiographic follow-up.
Figure 1 Radiographic images of endodontic treatment. (A) Initial radiograph of the case; (B) sinus tract tracking; (C) odontometry; (D) radiographic check-up examination to evaluate apical barrier formation; (E) formation of mineralized tissue between the cervical and middle thirds of the root canal; (F) increased deposition of mineralized tissue between the cervical and middle thirds of the root canal; (G) radiograph supporting root obturation; (H) final radiograph of root obturation; (I) radiographic follow-up examination 3 months after the endodontic intervention.
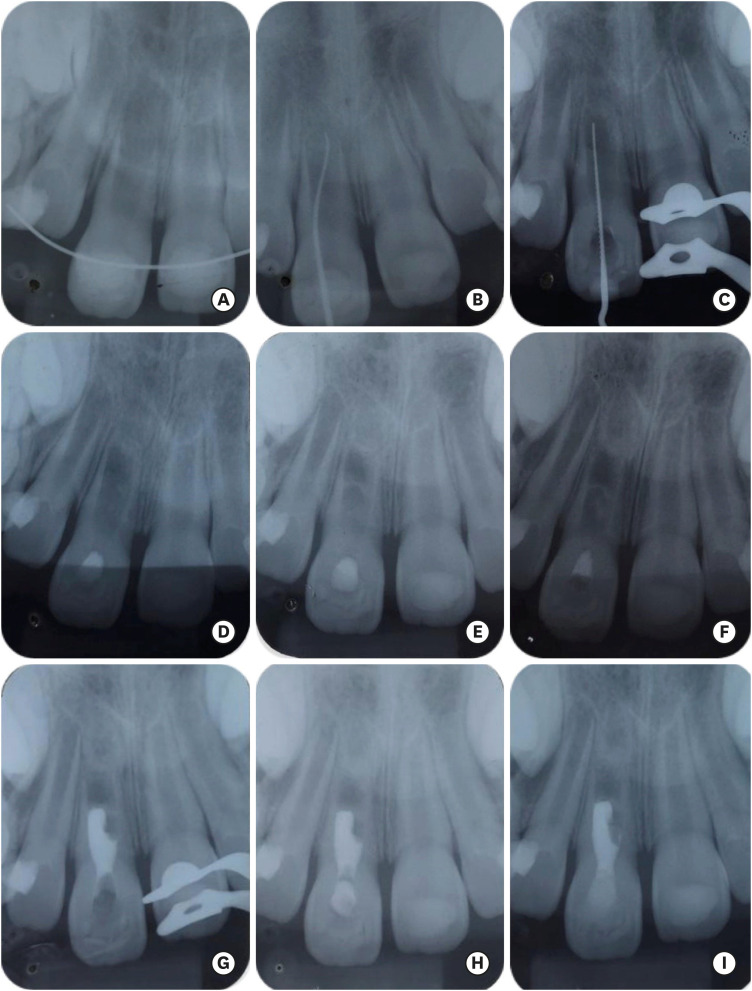
During the second session, a sinus tract originating in the root apex of tooth 11 was found (
Figure 1B); therefore, we opted for pulp revascularization. The following sequence of clinical steps was performed: 1) removal of the semi-rigid containment; 2) local anesthesia; 3) absolute isolation; 4) coronal opening; 5) disinfection of the conduit with 2.5% sodium hypochlorite (Asfer Indústria Química LTDA, São Caetano do Sul, SP, Brazil); 6) irrigation with 17% ethylenediaminetetraacetic acid solution (Biodynamics, Lobato, PR, Brazil) for 3 minutes, 7) root canal filling with calcium hydroxide (Biodynamics), and 8) double sealing with glass ionomer cement (Maxxion R, FGM, Joinville, SC, Brazil). A return visit was scheduled for 21 days later.
At the follow-up session, the patient's father reported that the cavity seal had been accidentally removed; therefore, a new root decontamination session and application of intracanal medication were carried out as described above. After 2 weeks, blood clot formation was planned, but the patient still had a fistula. Therefore, we decided to perform further decontamination and to determine the actual tooth length (
Figure 1C). After 14 days, when the patient returned without the fistula and with adequate coronal sealing, it was decided to attempt blood clot formation. The procedure included local anesthesia (Mepisv 3%, DFL) and promotion of bleeding inside the root canal by vigorous stimulation with 2-mm-caliber instruments longer than the actual tooth length (24 mm). Mild bleeding was detected inside the root canal; hence, the pulp chamber was cleaned, followed by root decontamination. Then, the root canal was filled with calcium hydroxide paste and a double seal was applied. Tactile detection of apical barrier formation was performed during this procedure.
Thirty days later, at the return visit, periapical radiography was performed to verify the presence of mineralized tissue in the root (
Figure 1D). Formation of an apical mineralized barrier was observed. Therefore, we chose to apply stimulation to the root canal using mechanical instrumentation again. Subsequently, we apply calcium hydroxide to the root canal to stimulate the deposition of mineralized tissue (apexification). After 2 monthly changes, a radiographic examination verified the beginning of mineralized tissue formation between the cervical and middle third of the root canal (
Figure 1E). In addition, minor intracanal bleeding was found during removal of the intracanal medication. Thus, we decided to renew the intracanal medication and perform clinical and radiographic analysis at a later session. At the follow-up session, an increase in the thickness of the apical barrier and between the cervical and middle third of the root canal (
Figure 1F) was detected. After this discovery, we opted to obturate of the portion of the root that was accessible via the canal.
Root obturation was performed 45 days after the last session by introducing Endosequence BC bioceramic cement (Brasseler, Savannah, GA, USA) without gutta-percha cones. On confirmatory radiography (
Figure 1G), an absence of material in the mesial region was noted, and even after successive attempts, it was impossible to fill (
Figure 1H). At subsequent consultations, restoration was performed with light-cured composite resin (Z250, 3M, Maple Wood, MN, USA), and further follow-up was scheduled.
To summarize, the treatment protocol used in this case was revascularization of the pulp of the replanted tooth. The technique was modified to include successive changes of intracanal medication before the use of biomaterial to control root infection, and the cervical third of the root was filled with a bioceramic material; in sequence, coronal restoration and clinical follow-up were performed.
At the 3-month follow-up after obturation, deposition of mineralized tissue beyond the initially formed apical barrier was noted (
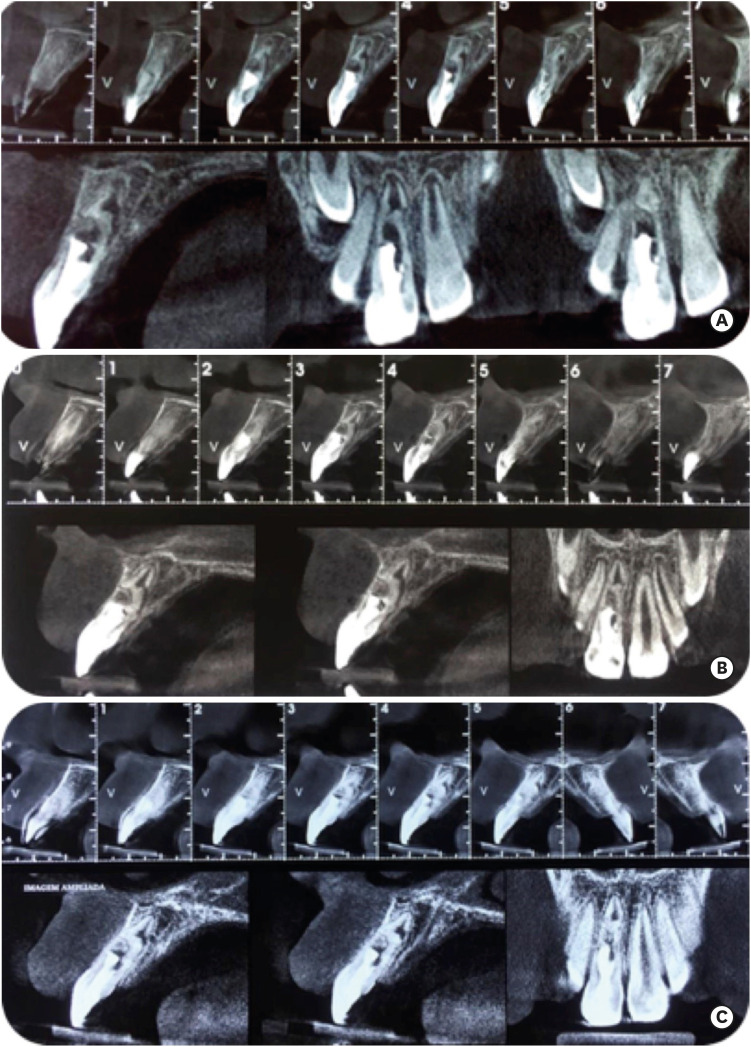
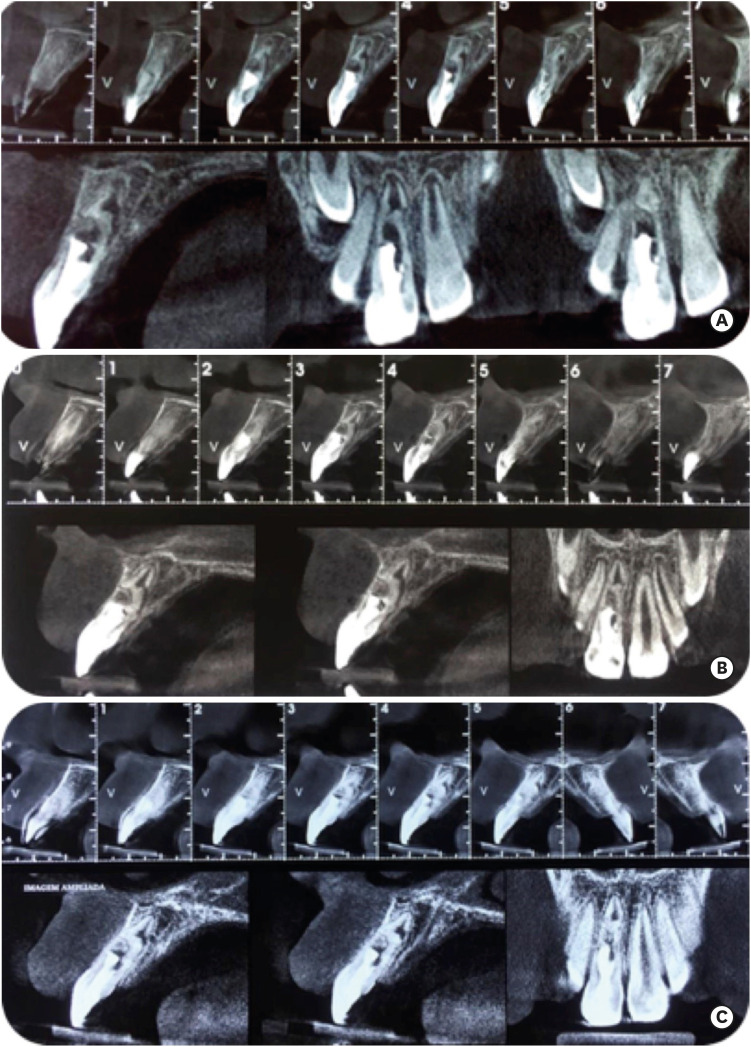
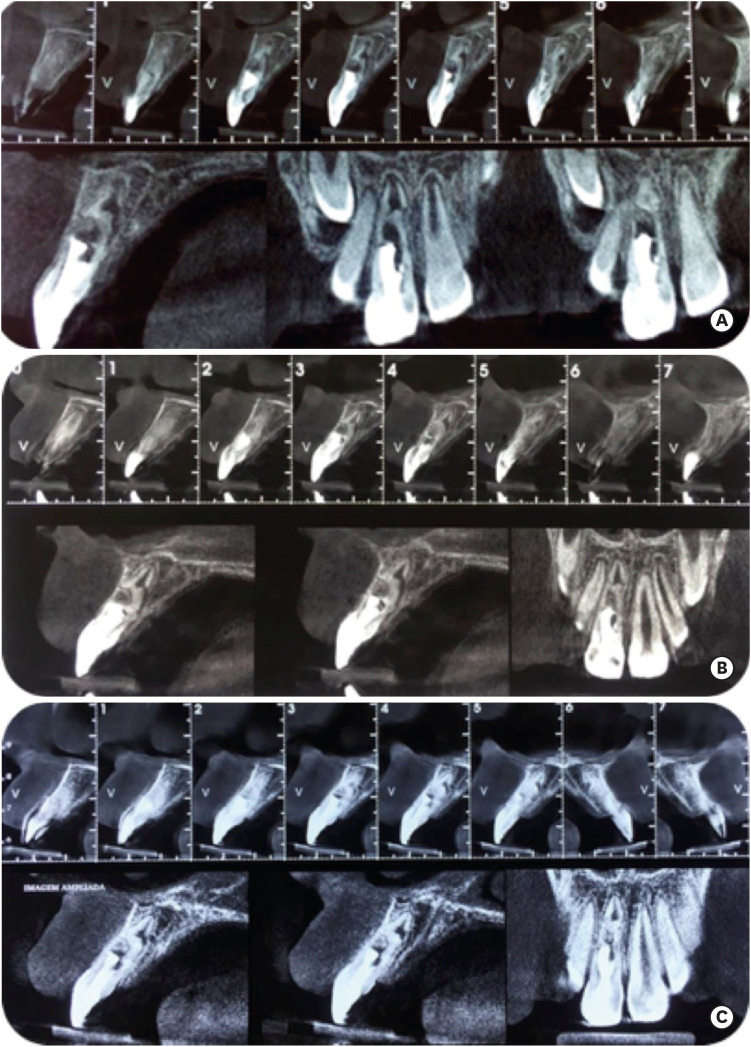
Figure 1I). Therefore, we chose to perform cone-beam computed tomography scans for a more detailed analysis of the root portion. Tomographic examinations over subsequent years showed root formation with an increase in thickness and length and absence of root resorption (
Figure 2). These data, combined with the absence of clinical symptoms and adequate coronal rehabilitation, demonstrated the success of the treatment.
Figure 2 Tomographic examinations to determine the absence of root resorption and occurrence of root development performed 6 (A), 18 (B) and 40 (C) months after the endodontic intervention was completed.
DISCUSSION
Studies have shown that dental trauma most commonly affects children between 7 and 12 years of age, leading to the loss of dental structures [
1,
3,
13]. This occurs because of the resilience of the periodontium and incomplete root development. The present clinical case report documents an avulsed tooth in a 7-year-old patient who presented with incomplete root development, confirming the data reported in the literature.
The avulsed tooth was replanted within 30 minutes. After a clinical examination, pulp sensitivity to cold was detected, possibly indicating pulp viability and consequent pulp tissue revascularization. Following the recommendations of the International Association for Dental Traumatology, follow-up of the case was proposed [
3].
During follow-up, a fistula was detected in the buccal gingiva of the tooth #11, with consequent pulp necrosis. Based on these findings, a change in the clinical treatment plan was devised. We chose to apply a pulp revascularization technique that would potentially culminate in root development and preservation of the tooth in the oral cavity [
8,
9,
10,
11,
14,
15].
During application of the technique described above, root canal disinfection should be performed to control pulp infection [
8,
9,
10,
15]. Sodium hypochlorite, which has tissue dissolution properties and exerts antimicrobial effects [
16,
17,
18], is the irrigation solution of choice in most cases. Different concentrations of sodium hypochlorite may be used [
19]; according to local availability, 2.5% sodium hypochlorite was used in this case. This concentration is typically used in endodontic treatment of teeth with pulp necrosis [
20].
An antibiotic paste consisting of a mixture of 3 antibiotics in equal doses and sterile saline may be used as an intracanal medication. However, regarding the survival of undifferentiated cells present in the apical region, this paste may be cytotoxic when used at concentrations of 1 mg/mL or greater. In addition, it can cause discoloration of the dentin, thereby promoting tooth staining [
21]. The clinical efficacy of calcium hydroxide as an intracanal medication for pulp revascularization has been proven [
22]. Calcium hydroxide has antimicrobial properties and is a bioactive material that can decontaminate the root canal and promote the stimulation of growth factors, with consequent formation of mineralized tissue [
23]. Thus, the use of calcium hydroxide as an intracanal medication was justified in this case.
At the patient's next visit, it was noted that the fistula had not regressed as it should have, and we developed 2 hypotheses to explain this result: 1) the 2.5% sodium hypochlorite concentration may not have been sufficient for tissue dissolution and disorganization of the microbial biofilm present in the root canal; or 2) resistant microbiota may have been present in the root canal and apical region, making treatment difficult [
24,
25]. Thus, new decontamination sessions were planned, since decontamination is of paramount importance for successful revascularization [
25].
The successive changes of calcium hydroxide paste for pulp decontamination may have prompted reduced bleeding during blood clot formation, since calcium hydroxide paste is alkaline and promotes self-limiting necrosis when in contact with the tissue [
26]. In addition, successive calcium hydroxide changes stimulated the formation of mineralized tissue in the apical region and the cervical and middle third of the root [
23], as portrayed in
Figure 1.
The biomaterial of choice for use in revascularization is the well-known mineral trioxide aggregate (MTA) [
25]. MTA improves root development in pulp revascularization because it stimulates cells from the blood clot, which contribute to the formation of mineralized tissue that enables root development with gains in thickness and length [
25]. The primary disadvantage of MTA is gradual discoloration of the tooth [
27], which was a particularly relevant problem in this case, as it involved the aesthetic area in a young patient. Therefore, in the present case, when treating the accessible third of the root, we decided to use the EndoSequence BC bioceramic cement. This material has adequate biocompatibility and excellent bioinductive capacity [
28]. This biomaterial improves mineralized tissue formation [
23,
28], similarly to MTA. In addition, EndoSequence BC does not induce changes in the color of the dental crown [
29], and it is easy to handle [
30]
. These properties justified the choice of EndoSequence BC as the biomaterial to be used in this case.
In fact, the bioinductive materials [
23,
27,
28] used in this clinical case probably contributed to the increase in root thickness shown in
Figure 2. The form of the root was unconventional, and a discontinuity in the root can be seen; this discontinuity most likely occurred during root development after pulp revascularization, which is a possible consequence of this endodontic treatment strategy [
8,
9] In addition, the antimicrobial properties associated with these materials [
23,
31] resulted in successful decontamination, limiting the inflammatory resorption process [
1]. In addition, the absence of clinical symptoms and the functional and aesthetic rehabilitation of the patient were verified, confirming that the described procedures were adequate for successful dental replantation.
Conclusion
The clinical management described herein of a pediatric patient with an avulsed right upper central incisor presenting with incomplete root development and chronic apical periodontitis was adequate and culminated in clinical success.
-
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
-
Author Contributions:
Conceptualization: Mori GG.
Data curation: Mori GG.
Formal analysis: Mori GG.
Investigation: Mori GG, Andrade BS, Araujo MB.
Methodology: Mori GG.
Project administration: Mori GG.
Resources: Mori GG, Andrade BS, Araujo MB.
Software: Andrade BS, Araujo MB.
Supervision: Mori GG.
Validation: Mori GG.
Visualization: Mori GG, Andrade BS, Araujo MB.
Writing - original draft: Andrade BS, Araujo MB.
Writing - review & editing: Mori GG.
REFERENCES
- 1. Andreasen JO, Andreasen FM, Andersson L. Textbook and color atlas of traumatic injuries to the teeth. 4th ed. Nova Jersey: Wiley-Blackwell; 2018.
- 2. Rodrigues Campos Soares T, de Andrade Risso P, Cople Maia L. Traumatic dental injury in permanent teeth of young patients attended at the federal University of Rio de Janeiro, Brazil. Dent Traumatol 2014;30:312-316.PubMed
- 3. Andersson L, Andreasen JO, Day P, Heithersay G, Trope M, DiAngelis AJ, Kenny DJ, Sigurdsson A, Bourguignon C, Flores MT, Hicks ML, Lenzi AR, Malmgren B, Moule AJ, Tsukiboshi M. Guidelines for the management of traumatic dental injuries: 2. Avulsion of permanent teeth. Pediatr Dent 2016;38:369-376.PubMed
- 4. Andersson L, Bodin I. Avulsed human teeth replanted within 15 minutes--a long-term clinical follow-up study. Endod Dent Traumatol 1990;6:37-42.PubMed
- 5. Mori GG, Nunes DC, Castilho LR, de Moraes IG, Poi WR. Propolis as storage media for avulsed teeth: microscopic and morphometric analysis in rats. Dent Traumatol 2010;26:80-85.ArticlePubMed
- 6. Mori GG, Poi WR, Castilho LR. Evaluation of the anti-resorptive ability of an experimental acetazolamide paste for the treatment of late replanted teeth: a study in rats. Dent Traumatol 2013;29:34-40.ArticlePubMed
- 7. Huang GT. Apexification: the beginning of its end. Int Endod J 2009;42:855-866.ArticlePubMed
- 8. Diogenes A, Henry MA, Teixeira FB, Hargreaves KM. An update on clinical regenerative endodontics. Endod Topics 2013;28:2-23.Article
- 9. Namour M, Theys S. Pulp revascularization of immature permanent teeth: a review of the literature and a proposal of a new clinical protocol. Sci World J 2014;2014:737503.ArticlePubMedPMCPDF
- 10. Moodley T, Patel N. Management of necrotic pulp of immature permanent incisor tooth: a regenerative endodontic treatment protocol: case report. SADJ 2017;72:122-125.
- 11. Thomson A, Kahler B. Regenerative endodontics--biologically-based treatment for immature permanent teeth: a case report and review of the literature. Aust Dent J 2010;55:446-452.ArticlePubMed
- 12. Nagata JY, Rocha-Lima TF, Gomes BP, Ferraz CC, Zaia AA, Souza-Filho FJ, De Jesus-Soares A. Pulp revascularization for immature replanted teeth: a case report. Aust Dent J 2015;60:416-420.ArticlePubMed
- 13. Mori GG, Turcio KH, Borro VP, Mariusso AM. Evaluation of the knowledge of tooth avulsion of school professionals from Adamantina, São Paulo, Brazil. Dent Traumatol 2007;23:2-5.ArticlePubMed
- 14. Silujjai J, Linsuwanont P. Treatment outcomes of apexification or revascularization in nonvital immature permanent teeth: a retrospective study. J Endod 2017;43:238-245.ArticlePubMed
- 15. Hargreaves KM, Diogenes A, Teixeira FB. Paradigm lost: a perspective on the design and interpretation of regenerative endodontic research. J Endod 2014;40(4 Supplement):S65-S69.ArticlePubMed
- 16. Zehnder M. Root canal irrigants. J Endod 2006;32:389-398.ArticlePubMed
- 17. Abuhaimed TS, Abou Neel EA. Sodium hypochlorite irrigation and its effect on bond strength to dentin. BioMed Res Int 2017;2017:1930360.ArticlePubMedPMCPDF
- 18. Gonçalves LS, Rodrigues RC, Andrade Junior CV, Soares RG, Vettore MV. The effect of sodium hypochlorite and chlorhexidine as irrigant solutions for root canal disinfection: a systematic review of clinical trials. J Endod 2016;42:527-532.ArticlePubMed
- 19. Murray PE, Garcia-Godoy F, Hargreaves KM. Regenerative endodontics: a review of current status and a call for action. J Endod 2007;33:377-390.ArticlePubMed
- 20. Rôças IN, Provenzano JC, Neves MA, Siqueira JF Jr. Disinfecting effects of rotary instrumentation with either 2.5% sodium hypochlorite or 2% chlorhexidine as the main irrigant: a randomized clinical study. J Endod 2016;42:943-947.ArticlePubMed
- 21. Kahler B, Chugal N, Lin LM. Alkaline materials and regenerative endodontics: a review. Materials (Basel) 2017;10:E1389.ArticlePubMedPMC
- 22. Iwaya S, Ikawa M, Kubota M. Revascularization of an immature permanent tooth with periradicular abscess after luxation. Dent Traumatol 2011;27:55-58.ArticlePubMed
- 23. Graham L, Cooper PR, Cassidy N, Nor JE, Sloan AJ, Smith AJ. The effect of calcium hydroxide on solubilisation of bio-active dentine matrix components. Biomaterials 2006;27:2865-2873.ArticlePubMed
- 24. Neelakantan P, Romero M, Vera J, Daood U, Khan AU, Yan A, Cheung GSP. Biofilms in endodontics-current status and future directions. Int J Mol Sci 2017;18:E1748.Article
- 25. Hargreaves KA. Regenerative endodontics. In: Hargreaves KM, Cohen S, editors. Cohen's pathways of the pulp. 10th ed. St. Louis: Elsevier; 2011. p. 602-619.
- 26. Banchs F, Trope M. Revascularization of immature permanent teeth with apical periodontitis: new treatment protocol? J Endod 2004;30:196-200.ArticlePubMed
- 27. Alsubait S, Al-Haidar S, Al-Sharyan N. A comparison of the discoloration potential for EndoSequence bioceramic root repair material fast set putty and ProRoot MTA in human teeth: an in vitro study. J Esthet Restor Dent 2017;29:59-67.ArticlePubMedPDF
- 28. Chen I, Karabucak B, Wang C, Wang HG, Koyama E, Kohli MR, Nah HD, Kim S. Healing after root-end microsurgery by using mineral trioxide aggregate and a new calcium silicate-based bioceramic material as root-end filling materials in dogs. J Endod 2015;41:389-399.ArticlePubMedPMC
- 29. Shokouhinejad N, Hoseini A, Gorjestani H, Raoof M, Assadian H, Shamshiri AR. Effect of phosphate-buffered saline on push-out bond strength of a new bioceramic sealer to root canal dentin. Dent Res J (Isfahan) 2012;9:595-599.ArticlePubMedPMC
- 30. Ciasca M, Aminoshariae A, Jin G, Montagnese T, Mickel A. A comparison of the cytotoxicity and proinflammatory cytokine production of EndoSequence root repair material and ProRoot mineral trioxide aggregate in human osteoblast cell culture using reverse-transcriptase polymerase chain reaction. J Endod 2012;38:486-489.ArticlePubMed
- 31. Candeiro GT, Moura-Netto C, D'Almeida-Couto RS, Azambuja-Júnior N, Marques MM, Cai S, Gavini G. Cytotoxicity, genotoxicity and antibacterial effectiveness of a bioceramic endodontic sealer. Int Endod J 2016;49:858-864.ArticlePubMedPDF
 , Bruna Souza Andrade1
, Bruna Souza Andrade1 , Marina Bardelli Araujo1
, Marina Bardelli Araujo1


 KACD
KACD
 ePub Link
ePub Link Cite
Cite

