Articles
- Page Path
- HOME > Restor Dent Endod > Volume 47(3); 2022 > Article
- Research Article Effects of different topical anesthetics on pain from needle insertion and injection, and the influence of anxiety in patients awaiting endodontic treatment
-
Fatih Aksoy1
 , Samet Tosun2
, Samet Tosun2
-
Restor Dent Endod 2022;47(3):e25.
DOI: https://doi.org/10.5395/rde.2022.47.e25
Published online: June 7, 2022
1Department of Endodontics, Faculty of Dentistry, Adıyaman University, Adıyaman, Turkey.
2Department of Endodontics, Faculty of Dentistry, Pamukkale University, Denizli, Turkey.
- Correspondence to Fatih Aksoy, DDS, PhD. Associate Professor, Department of Endodontics, Faculty of Dentistry, Adıyaman University, No:411, 02200, Adıyaman, Turkey. dr.f.aksoy@gmail.com
Copyright © 2022. The Korean Academy of Conservative Dentistry
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
Objectives This study aimed to evaluate the effects of 5% lidocaine and 2.5% lidocaine/2.5% prilocaine topical anesthetic on pain during needle insertion and infiltration injection in the labial mucosa of anterior maxillary teeth, and to assess the relationship between patients’ anxiety and pain scores.
-
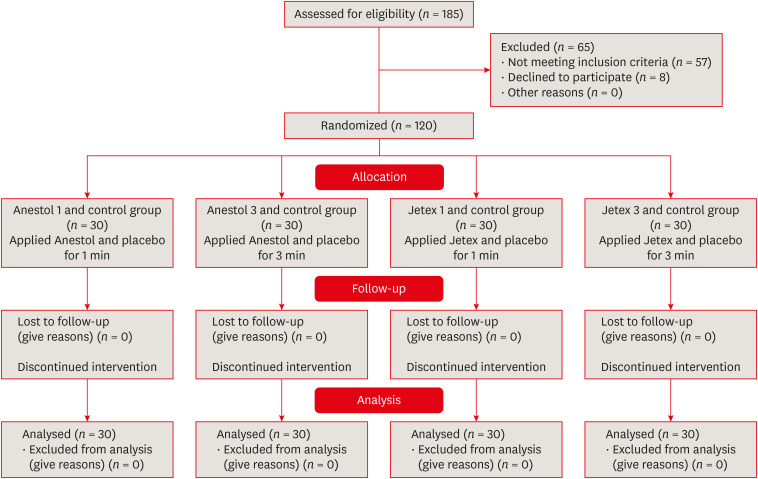
Materials and Methods The Modified Dental Anxiety Scale questionnaire was applied and recorded. Patients were randomly divided into 4 groups (n = 30), as follows: G1 group: 5% lidocaine and placebo for 1 minute, G2 group: 2.5% lidocaine/2.5% prilocaine and placebo for 1 minute, G3 group: 5% lidocaine and placebo for 3 minutes, and G4 group: 2.5% lidocaine/2.5% prilocaine and placebo for 3 minutes. Before the application of topical anesthesia, one side was randomly selected as the topical anesthesia and the contralateral side as the placebo. The pain levels were measured with Visual Analog Scale (VAS) immediately after needle insertion and injection and were compared. The correlation between anxiety and pain scores was analyzed.
-
Results Administration of 5% lidocaine for 1 minute had significantly higher pain scores for both insertion and infiltration injection than the other groups (p < 0.05). There was a significant moderate positive correlation between dental anxiety and the injection-induced VAS pain score in the placebo side in all groups (p < 0.05).
-
Conclusions Topical anesthetics significantly reduced the pain caused by both needle insertion and injection pain in comparison to the placebo side. The pain scores of patients with dental anxiety were lower on the topical anesthesia compared to the placebo side.
-
Trial Registration Thai Clinical Trials Registry Identifier: TCTR20201217002
INTRODUCTION
MATERIALS AND METHODS
RESULTS
Demographic data of the patients; MDAS scores of the all groups
The needle insertion and injection VAS scores of the groups.
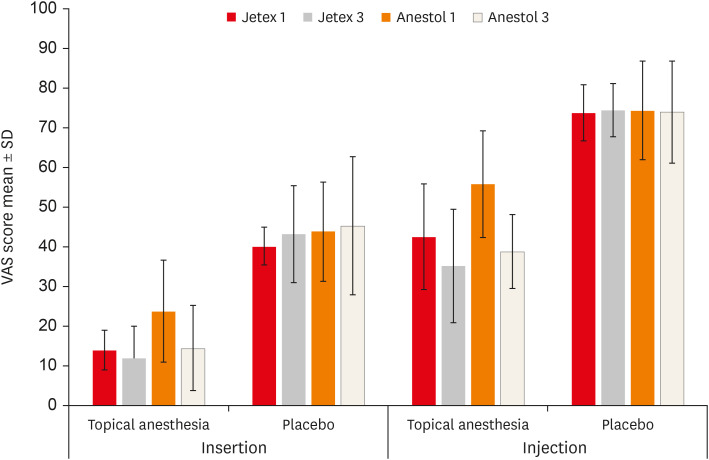
Comparison of Visual Analog Scale scores (mm) between placebo and anesthesia after both the needle insertion and injection in all group
Comparison of the Visual Analog Scale scores according to Modified Dental Anxiety Scale anxiety levels in all group
DISCUSSION
CONCLUSIONS
ACKNOWLEDGEMENTS
-
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
-
Author Contributions:
Conceptualization: Tosun S.
Data curation: Aksoy F.
Formal analysis: Aksoy F, Tosun S.
Investigation: Tosun S.
Methodology: Aksoy F.
Project administration: Aksoy F.
Supervision: Tosun S.
Validation: Tosun S.
Visualization: Tosun S.
Writing - original draft: Aksoy F, Tosun S.
Writing - review & editing: Aksoy F, Tosun S.
- 1. Parirokh M, Sadeghi AS, Nakhaee N, Pardakhty A, Abbott PV, Yosefi MH. Effect of topical anesthesia on pain during infiltration injection and success of anesthesia for maxillary central incisors. J Endod 2012;38:1553-1556.ArticlePubMed
- 2. Singh P. An emphasis on the wide usage and important role of local anesthesia in dentistry: a strategic review. Dent Res J (Isfahan) 2012;9:127-132.ArticlePubMedPMC
- 3. Leopold A, Wilson S, Weaver JS, Moursi AM. Pharmacokinetics of lidocaine delivered from a transmucosal patch in children. Anesth Prog 2002;49:82-87.PubMedPMC
- 4. Nakamura S, Matsuura N, Ichinohe T. A new method of topical anesthesia by using anesthetic solution in a patch. J Endod 2013;39:1369-1373.ArticlePubMed
- 5. Reader AW, Nusstein JM, Hargreaves KM. Local anesthesia in endodontics. Cohen’s pathways of the pulp. 10th ed. St Louis, MO: Mosby Elsevier; 2011. p. 691-719.
- 6. van Wijk AJ, Hoogstraten J. Anxiety and pain during dental injections. J Dent 2009;37:700-704.ArticlePubMed
- 7. van Wijk AJ, Makkes PC. Highly anxious dental patients report more pain during dental injections. Br Dent J 2008;205:E7.ArticlePubMedPDF
- 8. Cho SY, Kim E, Park SH, Roh BD, Lee CY, Lee SJ, Jung IY. Effect of topical anesthesia on pain from needle insertion and injection and its relationship with anxiety in patients awaiting apical surgery: a randomized double-blind clinical trial. J Endod 2017;43:364-369.ArticlePubMed
- 9. Bågesund M, Tabrizi P. Lidocaine 20% patch vs lidocaine 5% gel for topical anaesthesia of oral mucosa. Int J Paediatr Dent 2008;18:452-460.ArticlePubMed
- 10. Weilbach C, Hoppe C, Karst M, Winterhalter M, Raymondos K, Schultz A, Rahe-Meyer N. Effectiveness of various formulations of local anesthetics and additives for topical anesthesia - a prospective, randomized, double-blind, placebo-controlled study. J Pain Res 2017;10:1105-1109.PubMedPMC
- 11. Lee HS. Recent advances in topical anesthesia. J Dent Anesth Pain Med 2016;16:237-244.ArticlePubMedPMCPDF
- 12. Bhalla J, Meechan JG, Lawrence HP, Grad HA, Haas DA. Effect of time on clinical efficacy of topical anesthesia. Anesth Prog 2009;56:36-41.ArticlePubMedPMCPDF
- 13. Sanz R, Calpena AC, Mallandrich M, Clares B. Enhancing topical analgesic administration: review and prospect for transdermal and transbuccal drug delivery systems. Curr Pharm Des 2015;21:2867-2882.ArticlePubMed
- 14. Vickers ER, Punnia-Moorthy A. A clinical evaluation of three topical anaesthetic agents. Aust Dent J 1992;37:266-270.Article
- 15. Humphris GM, Morrison T, Lindsay SJ. The Modified Dental Anxiety Scale: validation and United Kingdom norms. Community Dent Health 1995;12:143-150.PubMed
- 16. Malamed SF. Handbook of local anesthesia-e-book. 7th ed. St Louis, MO: Elsevier Health Sciences; 2019.
- 17. Franz-Montan M, de Paula E, Groppo FC, Silva AL, Ranali J, Volpato MC. Liposomal delivery system for topical anaesthesia of the palatal mucosa. Br J Oral Maxillofac Surg 2012;50:60-64.ArticlePubMed
- 18. Drum M, Reader A, Beck M. Long buccal nerve block injection pain in patients with irreversible pulpitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2011;112:e51-e54.ArticlePubMed
- 19. Rosa AL, Sverzut CE, Xavier SP, Lavrador MA. Clinical effectiveness of lidocaine and benzocaine for topical anesthesia. Anesth Prog 1999;46:97-99.PubMedPMC
- 20. Svensson P, Petersen JK. Anesthetic effect of EMLA occluded with Orahesive oral bandages on oral mucosa. A placebo-controlled study. Anesth Prog 1992;39:79-82.PubMedPMC
- 21. Kincheloe JE, Mealiea WL Jr, Mattison GD, Seib K. Psychophysical measurement on pain perception after administration of a topical anesthetic. Quintessence Int 1991;22:311-315.PubMed
- 22. de Freiras GC, Pozzobon RT, Blaya DS, Moreira CH. Efficacy of benzocaine 20% topical anesthetic compared to placebo prior to administration of local anesthesia in the oral cavity: a randomized controlled trial. Anesth Prog 2015;62:46-50.ArticlePubMedPMCPDF
- 23. Revill SI, Robinson JO, Rosen M, Hogg MI. The reliability of a linear analogue for evaluating pain. Anaesthesia 1976;31:1191-1198.ArticlePubMed
- 24. McCormack HM, Horne DJ, Sheather S. Clinical applications of visual analogue scales: a critical review. Psychol Med 1988;18:1007-1019.ArticlePubMed
- 25. Sharifi R, Salehian S, Sadeghi M, Mozaffari HR. Effect of topical anesthetics on pain during needle insertion of maxillary infiltration anesthesia: a systematic review and meta-analysis study. Sch Acad J Pharm 2017;6:16-26.
- 26. Sharifi R, Nazari H, Bolourchi P, Khazaei S, Parirokh M. The most painful site of maxillary anterior infiltrations. Dent Res J (Isfahan) 2016;13:539-543.ArticlePubMedPMC
- 27. Yonchak T, Reader A, Beck M, Clark K, Meyers WJ. Anesthetic efficacy of infiltrations in mandibular anterior teeth. Anesth Prog 2001;48:55-60.PubMedPMC
- 28. Meechan JG. Intra-oral topical anaesthetics: a review. J Dent 2000;28:3-14.ArticlePubMed
- 29. Daneshkazemi A, Abrisham SM, Daneshkazemi P, Davoudi A. The efficacy of eutectic mixture of local anesthetics as a topical anesthetic agent used for dental procedures: a brief review. Anesth Essays Res 2016;10:383-387.ArticlePubMedPMC
- 30. Yaacob HB, Noor GM, Malek SN. The pharmacological effect of xylocaine topical anaesthetic--a comparison with a placebo. Singapore Dent J 1981;6:55-57.PubMed
- 31. Tunc EP, Firat D, Onur OD, Sar V. Reliability and validity of the Modified Dental Anxiety Scale (MDAS) in a Turkish population. Community Dent Oral Epidemiol 2005;33:357-362.ArticlePubMed
- 32. Humphris GM, Hull P. Do dental anxiety questionnaires raise anxiety in dentally anxious adult patients? A two-wave panel study. Prim Dent Care 2007;14:7-11.ArticlePubMedPDF
- 33. Sghaireen MG, Zwiri AM, Alzoubi IA, Qodceih SM, Al-Omiri MK. Anxiety due to dental treatment and procedures among university students and its correlation with their gender and field of study. Int J Dent 2013;2013:647436.ArticlePubMedPMCPDF
- 34. Dou L, Vanschaayk MM, Zhang Y, Fu X, Ji P, Yang D. The prevalence of dental anxiety and its association with pain and other variables among adult patients with irreversible pulpitis. BMC Oral Health 2018;18:101.ArticlePubMedPMCPDF
- 35. Economou GC. Dental anxiety and personality: investigating the relationship between dental anxiety and self-consciousness. J Dent Educ 2003;67:970-980.ArticlePubMedPDF
- 36. Mehrstedt M, John MT, Tönnies S, Micheelis W. Oral health-related quality of life in patients with dental anxiety. Community Dent Oral Epidemiol 2007;35:357-363.ArticlePubMed
- 37. Neelakantan P, Liu P, Dummer PM, McGrath C. Oral health-related quality of life (OHRQoL) before and after endodontic treatment: a systematic review. Clin Oral Investig 2020;24:25-36.ArticlePubMedPDF
- 38. Armfield JM, Heaton LJ. Management of fear and anxiety in the dental clinic: a review. Aust Dent J 2013;58:390-407.ArticlePubMed
- 39. Dou L, Luo J, Yang D. Anaesthetic efficacy of supplemental lingual infiltration of mandibular molars after inferior alveolar nerve block plus buccal infiltration in patients with irreversible pulpitis. Int Endod J 2013;46:660-665.ArticlePubMed
REFERENCES
Tables & Figures
REFERENCES
Citations

- Rapid local anesthesia in children enhanced by STAR particles: a first-in-humans, randomized clinical trial
Andrew R. Tadros, Mark R. Prausnitz, Eric I. Felner
Drug Delivery and Translational Research.2026; 16(2): 539. CrossRef - Evaluation of Articaine Infiltration Location on the Success Rate of Mandibular Lateral Incisor Anesthesia: A Prospective Crossover Randomized Clinical Trial Study
Alireza Adl, Fahime Alimardani, Fereshte Sobhnamayan
Journal of Endodontics.2026; 52(2): 175. CrossRef - The Case for Transdermal Lidocaine 7.5% in the Management of Localized Pain: A Biopharmaceutical Review
Alexandra LaStella
Scriptum Pharmacologia .2025;[Epub] CrossRef - A Framework for the Modulation and Alleviation of Pain Sensations: A Narrative Review
Rushita Dobariya, Niraj Kinariwala, Nirav Parekh, Dhruvi Gangani, Devshree Dave, Hasti Maru, Nandani Mangukiya, Siddhi Singh
Cureus.2025;[Epub] CrossRef - Phacoemulsification Techniques and Their Effects on Corneal Endothelial Cells and Visual Acuity: A Review of "Direct-Chop" and "Stop-and-Chop" Approaches Under Topical Anesthesia
Devwrath Upasani, Sachin Daigavane
Cureus.2024;[Epub] CrossRef - Local anaesthetics in pediatric dental practice (literature review)
E. V. Ekimov, G. I. Skripkina, A. Zh. Garifullina, N. V. Chumichkin
Pediatric dentistry and dental prophylaxis.2023; 23(3): 211. CrossRef
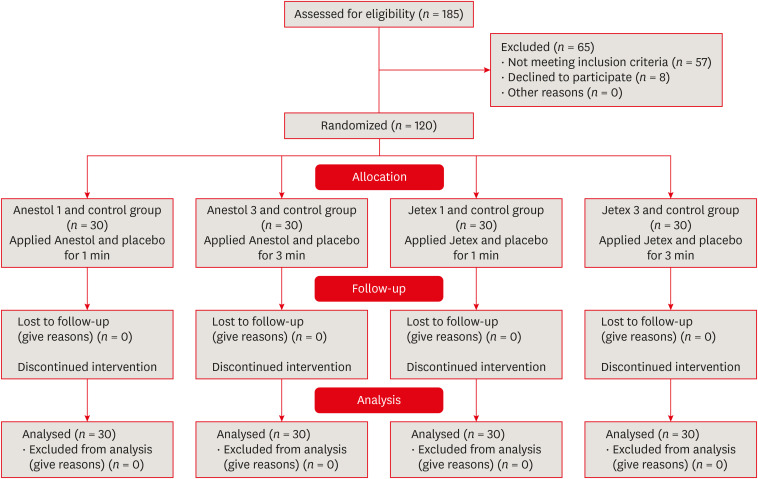
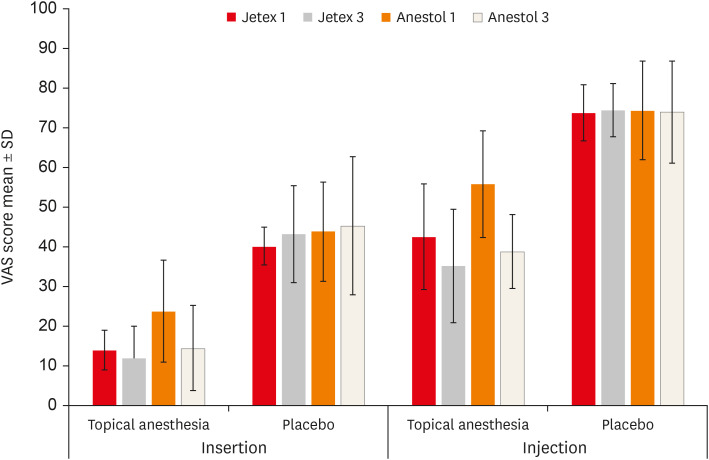
Figure 1
Figure 2
Demographic data of the patients; MDAS scores of the all groups
| Demographic data | G2 ( | G4 ( | G1 ( | G3 ( | Total ( | ||
|---|---|---|---|---|---|---|---|
| Age (yr) | 38.30 ± 12.77 | 38.63 ± 10.04 | 37.57 ± 12.84 | 37.60 ± 12.86 | 38.03 ± 12.06 | 0.959*a | |
| Sex (M/F) | 17/13 (56.7/43.3) | 14/16 (46.7/53.3) | 13/17 (43.3/56.7) | 17/13 (56.7/43.3) | 61/59 (50.8/49.2) | 0.698*b | |
| MDAS score | 12.17 ± 2.57 | 12.23 ± 2.76 | 12.13 ± 4.20 | 12.27 ± 3.62 | 0.970*a | ||
| ≥ 12 | 15 | 14 | 18 | 14 | 59 (49.2) | 0.637*b | |
| < 12 | 15 | 16 | 12 | 16 | 61 (50.8) | ||
Values are presented as number (%) or mean ± standard deviation.
MDAS, Modified Dental Anxiety Scale.
*
aKruskal-Wallis variance analysis; bChi-square test.
Comparison of Visual Analog Scale scores (mm) between placebo and anesthesia after both the needle insertion and injection in all group
| Group | G2 (1) | G4 (2) | G1 (3) | G3 (4) | Intergroup | |
|---|---|---|---|---|---|---|
| Insertion | ||||||
| Topical anesthesia | 14.00 ± 5.02 | 11.93 ± 8.17 | 23.80 ± 12.89 | 14.50 ± 10.71 | 0.0001*a (2–3, 3–4, 1–3) | |
| Placebo | 40.20 ± 4.79 | 43.20 ± 12.21 | 43.90 ± 12.47 | 45.30 ± 17.42 | 0.752a | |
| In-group | 0.0001*f | 0.0001*e | 0.0001*f | 0.0001*f | ||
| Injection | ||||||
| Topical anesthesia | 42.53 ± 13.35 | 35.23 ± 14.3 | 55.8 ± 13.44 | 38.83 ± 9.31 | 0.0001*a (2–3, 3–4, 1–3) | |
| Placebo | 73.77 ± 7.11 | 74.53 ± 6.71 | 74.43 ± 12.4 | 73.97 ± 12.87 | 0.960a | |
| In-group | 0.0001*f | 0.0001*e | 0.0001*e | 0.0001*f | ||
Values are expressed as mean ± standard deviation.
*
aKruskal-Wallis variance analysis; ePaired samples
Comparison of the Visual Analog Scale scores according to Modified Dental Anxiety Scale anxiety levels in all group
| Group | Anxiety | Intergroup | |||
|---|---|---|---|---|---|
| < 12 | ≥ 12 | ||||
| G2 | |||||
| Insertion | |||||
| Topical anesthesia | 14.07 ± 5.86 | 13.93 ± 4.23 | 0.775d | ||
| Placebo | 39.6 ± 4.79 | 40.8 ± 4.87 | 0.539d | ||
| In-group | 0.001*f | 0.0001*e | |||
| Injection | |||||
| Topical anesthesia | 38.67 ± 14.65 | 46.40 ± 11.06 | 0.187d | ||
| Placebo | 70.07 ± 6.17 | 77.47 ± 6.10 | 0.003*d | ||
| In-group | 0.001*f | 0.0001*e | |||
| G4 | |||||
| Insertion | |||||
| Topical anesthesia | 11.56 ± 5.21 | 12.36 ± 10.82 | 0.423d | ||
| Placebo | 40.25 ± 7.79 | 46.57 ± 15.48 | 0.294d | ||
| In-group | 0.0001*e | 0.0001*e | |||
| Injection | |||||
| Topical anesthesia | 33.75 ± 7.80 | 36.93 ± 19.50 | 0.886d | ||
| Placebo | 71.31 ± 4.19 | 78.21 ± 7.27 | 0.003*c | ||
| In-group | 0.0001*e | 0.0001*e | |||
| G1 | |||||
| Insertion | |||||
| Topical anesthesia | 17.17 ± 11.53 | 28.22 ± 12.06 | 0.022*d | ||
| Placebo | 36.17 ± 8.57 | 49.06 ± 12.15 | 0.003*d | ||
| In-group | 0.0001*e | 0.0001*e | |||
| Injection | |||||
| Topical anesthetic | 50.08 ± 14.11 | 59.61 ± 11.88 | 0.072d | ||
| Placebo | 65.83 ± 12.28 | 80.17 ± 8.82 | 0.001*d | ||
| In-group | 0.004*e | 0.0001*e | |||
| G3 | |||||
| Insertion | |||||
| Topical anesthesia | 11.06 ± 6.21 | 18.43 ± 13.43 | 0.334d | ||
| Placebo | 44.19 ± 16.8 | 46.57 ± 18.65 | 0.715c | ||
| In-group | 0.0001*e | 0.001*f | |||
| Injection | |||||
| Topical anesthesia | 39.38 ± 6.95 | 38.21 ± 11.71 | 0.728d | ||
| Placebo | 67.69 ± 10.74 | 81.14 ± 11.51 | 0.001*d | ||
| In-group | 0.0001*e | 0.001*f | |||
Values are expressed as mean ± standard deviation.
*
cIndependent samples
Values are presented as number (%) or mean ± standard deviation.
MDAS, Modified Dental Anxiety Scale.
*
aKruskal-Wallis variance analysis; bChi-square test.
Values are expressed as mean ± standard deviation.
*
aKruskal-Wallis variance analysis; ePaired samples
Values are expressed as mean ± standard deviation.
*
cIndependent samples

 KACD
KACD
 ePub Link
ePub Link Cite
Cite

