Articles
- Page Path
- HOME > Restor Dent Endod > Volume 47(2); 2022 > Article
- Review Article Deep proximal margin rebuilding with direct esthetic restorations: a systematic review of marginal adaptation and bond strength
-
Hoda S. Ismail1
 , Ashraf I. Ali1
, Ashraf I. Ali1 , Rabab El. Mehesen1
, Rabab El. Mehesen1 , Jelena Juloski2,3
, Jelena Juloski2,3 , Franklin Garcia-Godoy4,5
, Franklin Garcia-Godoy4,5 , Salah H. Mahmoud6
, Salah H. Mahmoud6
-
Restor Dent Endod 2022;47(2):e15.
DOI: https://doi.org/10.5395/rde.2022.47.e15
Published online: March 4, 2022
1Operative Dentistry Department, Faculty of Dentistry, Mansoura University, Egypt.
2Clinic for Pediatric and Preventive Dentistry, School of Dental Medicine, University of Belgrade, Serbia.
3Department of Medical Biotechnologies, University of Siena, Siena, Italy.
4Department of Bioscience Research, College of Dentistry, University of Tennessee Health Science Center, Memphis, TN, USA.
5The Forsyth Institute, Cambridge, MA, USA.
6Operative Dentistry Department, Faculty of Dentistry, Mansoura University, Egypt.
- Correspondence to Jelena Juloski. Assistant Professor, Clinic for Pediatric and Preventive Dentistry, School of Dental Medicine, University of Belgrade, Doktora Subotica Starijeg 11, 11000 Belgrade, Serbia. jelena.juloski@stomf.bg.ac.rs
Copyright © 2022. The Korean Academy of Conservative Dentistry
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
- This review aimed to characterize the effect of direct restorative material types and adhesive protocols on marginal adaptation and the bond strength of the interface between the material and the proximal dentin/cementum. An electronic search of 3 databases (the National Library of Medicine [MEDLINE/PubMed], Scopus, and ScienceDirect) was conducted. Studies were included if they evaluated marginal adaptation or bond strength tests for proximal restorations under the cementoenamel junction. Only 16 studies met the inclusion criteria and were included in this review. These studies presented a high degree of heterogeneity in terms of the materials used and the methodologies and evaluation criteria of each test; therefore, only a descriptive analysis could be conducted. The included studies were individually evaluated for the risk of bias following predetermined criteria. To summarize the results of the included studies, the type of restorative material affected the test results, whereas the use of different adhesive protocols had an insignificant effect on the results. It could be concluded that various categories of resin-based composites could be a suitable choice for clinicians to elevate proximal dentin/cementum margins, rather than the open sandwich technique with resin-modified glass ionomers. Despite challenges in bonding to proximal dentin/cementum margins, different adhesive protocols provided comparable outcomes.
INTRODUCTION
MATERIALS AND METHODS
1. What is the potential best direct restorative material (C) in terms of marginal adaptation and bond strength (O) to elevate (I) the dentin/cementum cervical margins in class II cavities to be restored with direct restoration (P)?
2. What is likely to be the most suitable adhesive protocol (C), in terms of marginal adaptation and bond strength (O), that should be used with restorative materials to bond to (I) dentin/cementum cervical margins in class II cavities to be restored with direct restoration (P)?
RESULTS
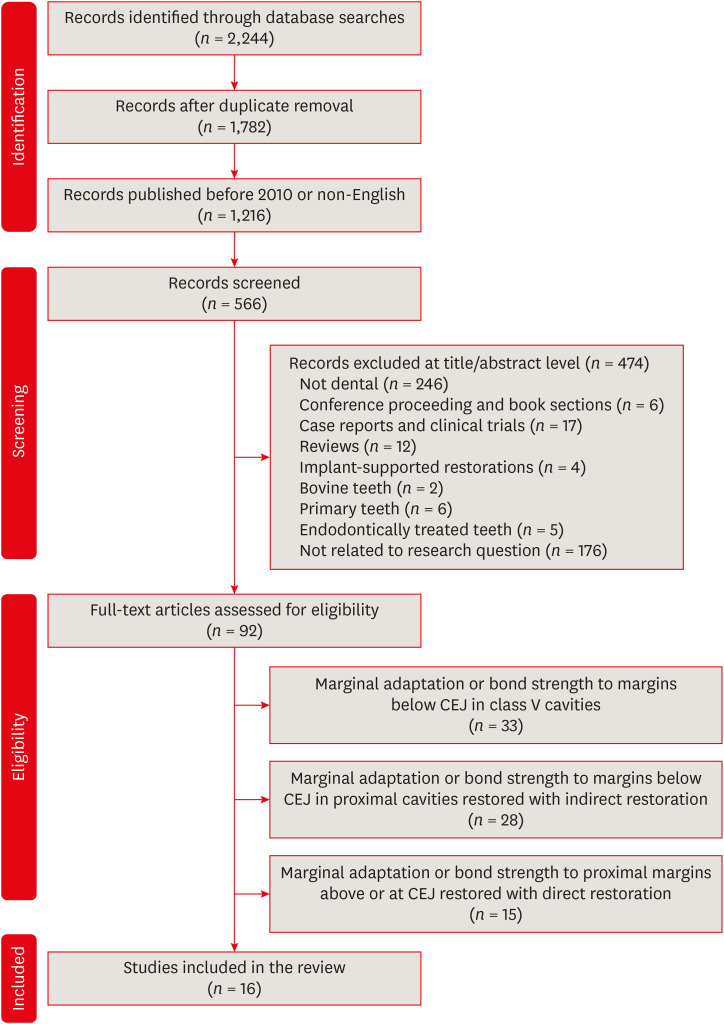
Search flowchart as adapted from the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.
Assessment of sample sizes, test types, and aging methodologies
| Study | Sample type and size and cavity type | Test type | Aging methodology |
|---|---|---|---|
| Aggarwal and Bhasin [20] | 80 molars | Marginal adaptation | Storage in PBS for 6 mon |
| Class II | |||
| Al-Harbi et al. [21] | 91 premolars | Marginal adaptation | 5,000 TC (55°C ± 2°C) (50°C ± 2°C), 1,000 MLC |
| Class II on each side | Margins assessment by FDI ranking | ||
| Kumagai et al. [22] | 44 molars | μTBS | |
| Complex Class II | Failure mode analysis | ||
| Al-Harbi et al. [23] | 91 premolars | μTBS | 5,000 TS (55°C ± 2°C) (50°C ± 2°C), 1,000 MLC |
| Class II on each side | Failure mode analysis | ||
| Marginal adaptation | |||
| Aggarwal et al. [24] | 60 molars | Marginal adaptation | 150,000 MLC, 3 mon PBS storage |
| Class II | |||
| Koyuturk et al. [25] | 60 premolars | μTBS | 10,000 TC (5°C–50°C), 50,000 MLC |
| Class II | Failure mode analysis | ||
| Czarnecka et al. [26] | 10 molars and premolars | Marginal and internal adaptation | |
| Class II on each side | |||
| Campos et al. [27] | 40 molars | Marginal adaptation | 600 TC (5°C–50°C) and 240,000 MLC |
| Class II | |||
| Aggarwal et al. [28] | 90 molars | Marginal adaptation | 150,000 MLC |
| Class II | |||
| Zaruba et al. [29] | 30 molars | Marginal adaptation | 6,000 TC (5°C–50°C) and 1.2 × 106 MLC |
| Class II on each side | |||
| de Mattos Pimenta Vidal et al. [30] | 72 premolars | μTBS | 3,000 TC (20°C–80°C) and 500,000 MLC |
| Class II on each side | |||
| Lefever et al. [31] | 88 molars | Marginal adaptation | |
| Class II | |||
| Rodrigues Junior et al. [32] | 32 molars | Marginal adaptation | 500 TC (5°C–55°C) |
| Class II on each side | |||
| Garcia-Godoy et al. [33] | 32 molars | Marginal adaptation | Half of the specimens were stored in water for 2,190 days, the other half were subjected to 2,500 TC (5°C–55°C) and 100,000 MLC |
| Class II | |||
| Fabianelli et al. [34] | 30 molars | Marginal adaptation | 500 TC (5°C–55°C) |
| Class II | |||
| Cavalcanti et al. [35] | 36 molars | μTBS | |
| Complex Class II |
Scientific categories, brand names of restorative materials, and adhesives used
| Study | Restorative materials used | Adhesives used |
|---|---|---|
| Aggarwal and Bhasin [20] | Nanofilled flowable composite (Filtek Z350 XT) | Ethanol-based ER adhesive (Single Bond) |
| Microhybrid flowable composite (Esthet-X Flow) | Acetone-based ER adhesive (Prime & Bond NT) | |
| Nanofilled RC (Z350) | ||
| CSM (ProRoot MTA White) | ||
| Al-Harbi et al. [21] | Microhybrid heavy body (Tetric Ceram HB) | ER adhesives (Tetric N-Bond, ExciTE F) |
| Microhybrid flowable composite (Tetric EvoFlow) | SE adhesives (Tetric N-Bond Self-Etch, AdheSE) | |
| Bulk-fill flowable composite (SDR) | Silorane-specific adhesive (P90 System) | |
| Bulk-fill low-shrinkage composite (SonicFill Composite) | ||
| Bulk-fill RC (Tetric N-Ceram Bulk Fill, Tetric EvoCeram Bulk Fill) | ||
| Low-shrink silorane-based composite (Filtek P90) | ||
| Kumagai et al. [22] | Bulk-fill flowable composite (SDR) | Two-step ER adhesives (XP Bond) |
| Nanofilled RC (Z350) | ||
| Al-Harbi et al. [23] | Microhybrid heavy body (Tetric Ceram HB) | ER adhesive (Tetric N-Bond, ExciTE F) |
| Microhybrid flowable composite (Tetric EvoFlow) | SE adhesive (Tetric N-Bond Self-Etch, AdheSE) | |
| Bulk-fill flowable composite (SDR) | Silorane-specific adhesive (P90 System) | |
| Bulk-fill low-shrinkage composite (SonicFill Composite) | ||
| Bulk-fill RC (Tetric N-Ceram Bulk Fill, Tetric EvoCeram Bulk Fill) | ||
| Low-shrink silorane-based composite (Filtek P90) | ||
| Aggarwal et al. [24] | CSMs (Biodentine, MTA Plus) | ER adhesive (Single Bond) |
| Nano RMGI (Ketac N100) | Two-step SE adhesive (One Coat Self Etching Bond) | |
| Nanofilled RC (Z350) | ||
| Nanohybrid RC (Synergy D6 Universal) | ||
| Koyuturk et al. [25] | Hybrid composite (ÆLITE LS Posterior/Bisco) | ER adhesive (Prime&Bond NT) |
| Bulk-fill flowable composite (SureFil SDR flow/Dentsply) | SE adhesive (Clearfil S3 Bond) | |
| Czarnecka et al. [26] | GIC (Ketac Molar or Fuji IX) | ER adhesive |
| Nano RMGI and RMGI (N100 or Fuji IILC) | ||
| Microhybrid RC (Filtek Z250) | ||
| Campos et al. [27] | Flowable bulk-fill composites (Venus Bulk Fill, Surefill SDR, Tetric EvoCeram Bulk Fill) | ER adhesive (Optibond FL) |
| Nano-hybrid RC (Venus, Tetric EvoCeram) | ||
| Nano-ceramic RC (Ceram-X) | ||
| Bulk-fill low-shrinkage composite (SonicFill) | ||
| Aggarwal et al. [28] | Nanofilled flowable RC (Filtek Z350, Synergy D6 flow) | ER adhesive (Single Bond) |
| Nano RMGI (N100) | One-step SE adhesive (Adper Easy Bond) | |
| Nanohybrid RC (Z350, Synergy D6 Universal) | Two-step SE adhesive (One Coat) | |
| Zaruba et al. [29] | Nanohybrid RC (Ceram X mono) | ER adhesive (XP Bond) |
| Flowable bulk-fill composites (Surefill SDR) | ||
| Microhybrid flowable RC (x-flow) | ||
| de Mattos Pimenta Vidal et al. [30] | Nanofilled RC (Filtek Supreme Plus Universal Restorative) | ER adhesive (Adper Single Bond Plus) |
| Nanofilled flowable RC (Filtek Supreme Plus Flowable Restorative) | ||
| RMGIC (Vitrebond Plus) | ||
| Lefever et al. [31] | Low-shrink silorane-based composite (Filtek Silorane) | Silorane-specific adhesive (P90 System) |
| Microhybrid composite (CLEARFIL AP-X) | SE adhesive (Clearfil Protect Bond) | |
| Nanofilled RC (Clearfil Majesty Posterior) | ||
| Self-adhering RC (Vertise Flow) | ||
| Self-adhesive resin cement (RelyX Unicem) | ||
| Nanohybrid flowable RC (Clearfil Majesty Flow) | ||
| Flowable bulk-fill composite (Surefill SDR) | ||
| Rodrigues Junior et al. [32] | Microhybrid composite (Z250) | ER adhesive (Single Bond) |
| Dental amalgam (Logic Plus) | ||
| RMGIC (Vitrebond) | ||
| Garcia-Godoy et al. [33] | Nanohybrid composite (Tetric Ceram and Grandio voco) | SE adhesives (Syntac, Solobond M) |
| Fabianelli et al. [34] | Microhybrid RC (Estelite Sigma) | SE adhesive (Bond Force) |
| Microhybrid flowable RC (Palfique Estelite LV) | ||
| Cavalcanti et al. [35] | Microhybrid composite (Z250) | ER adhesive (Single Bond Plus) |
| Two-step SE adhesive (Clearfil SE Bond) | ||
| One-step SE adhesive (Adper Prompt) |
1. Assessment of marginal adaptation
1) Testing methodology
(1) Finishing and polishing of gingival margins pre-test
(2) Direct or replica
(3) Examination method
Assessment of marginal adaptation evaluation methodologies
| Study | F/P of margins prior to testing | Direct or replica | Examination method | No. of margins assessed | Criteria for evaluation |
|---|---|---|---|---|---|
| Aggarwal and Bhasin [20] | Immediate + cleaning with H3PO4 for 5 seconds | Replica | (65–1,500×) SEM | Cervical dentin | % CM |
| Al-Harbi et al. [21] | Immediate | Replica | 200× SEM | Enamel and dentin gingival margins | % CM + FDI ranking |
| Al-Harbi et al. [23] | Immediate | Direct | 1,200× SEM | Enamel and dentin gingival margins | Measuring maximum gap in microns |
| Aggarwal et al. [24] | Immediate | Direct | (25–300×) SEM | Cervical dentin | % CM |
| Czarnecka et al. [26] | Delayed | Direct | 100× Metallographic light microscope | Cervical dentin + internal adaptation | Adequate or inadequate margins |
| Campos et al. [27] | Immediate | Replica before and after aging | 200× SEM | Occlusal, proximal enamel and cervical dentin | % CM |
| Aggarwal et al. [28] | Immediate | Direct | 200× SEM | Cervical dentin | % CM |
| Zaruba et al. [29] | Immediate | Replica before and after aging | 200× SEM | Proximal enamel, proximal and cervical dentin | % CM |
| Lefever et al. [31] | Immediate | Replica | 200× SEM | Proximal enamel, proximal and cervical dentin | % CM |
| Rodrigues Junior et al. [32] | Delayed | Replica | 200× SEM | Enamel and dentin gingival margins | Qualitative analysis |
| Garcia-Godoy et al. [33] | Immediate | Replica before and after aging | 200× SEM | Proximal enamel, proximal and cervical dentin | % CM |
| Fabianelli et al. [34] | -* | Replica | (25–1,400×) SEM | Cervical dentin | Qualitative analysis |
(4) Number of margins assessed
(5) Criteria for evaluation
2) Assessment of marginal adaptation results
(1) OST with RMGI
(2) OST with flowable resin composites
(3) Effect of different liner thicknesses
(4) Flowable bulk-fill composites
(5) Silorane-based composites
(6) The effect of different bonding protocols
2. Assessment of μTBS between restorative materials and tooth structure
1) Testing methodology
(1) Testing machine and crosshead speed
(2) Shape and number of bonded specimens (beams)
(3) Cross-sectional surface area of the bonded specimen
(4) Type of margins and walls examined
(5) Method of failure analysis
(6) Scoring of failure types
(7) Calculation of μTBS values
Assessment of microtensile bond strength testing methodologies
| Study | Testing machine | Crosshead speed | Shape and no. of bonded specimens | Cross-section of bonded specimens | Types of margins and walls evaluated | Method of failure analysis | Scoring of failure type |
|---|---|---|---|---|---|---|---|
| Kumagai et al. [22] | UTM | 1 mm/min | 3 Rectangular S/R | 1 mm2 | Dentin/cementum | 50× Light microscope | 1. Cohesive in dentin |
| 2. Cohesive in resin | |||||||
| 3. Adhesive | |||||||
| Al-Harbi et al. [23] | UTM | 0.5 mm/min | 2 Hourglass S/R | 0.8 mm2 | Enamel and Dentin/cementum | 40× Stereomicroscope + 500× SEM | As above + mixed |
| Koyuturk et al. [25] | -* | - | Rectangular | 1 mm2 | Dentin/cementum | 40× Stereomicroscope | As above + mixed |
| de Mattos Pimenta Vidal et al. [30] | Microtensile tester | 1 mm/min | 2 Hourglass S/R | 1 mm2 | Dentin/cementum | - | - |
| Cavalcanti et al. [35] | UTM | 0.5 mm/min | 3 Hourglass S/R | 1 mm2 | Pulpal, axial and gingival preparation walls | - | Scoring of specimens with premature failure |
2) Assessment of μTBS results
(1) OST with RMGI or flowable composites
(2) Flowable bulk-fill composites
(3) Silorane
(4) The effect of different adhesive protocols
(5) Failure modes
DISCUSSION
CONCLUSIONS
-
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
-
Conflict of interest: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
-
Author Contributions:
Conceptualization: Ismail HS, Ali AI, Mahmoud SH.
Data curation: Ismail HS.
Formal analysis: Ismail HS, Mehesen RE.
Investigation: Ismail HS.
Methodology: Ali AI, Mehesen RE.
Supervision: Mehesen RE, Juloski J, Garcia-Godoy F, Mahmoud SH.
Visualization: Mehesen RE.
Writing - original draft: Ismail HS.
Writing - review & editing: Ali AI, Mehesen RE, Juloski J, Mahmoud SH.
- 1. Shenoy A. Is it the end of the road for dental amalgam? A critical review. J Conserv Dent 2008;11:99-107.ArticlePubMedPMC
- 2. Zhou X, Huang X, Li M, Peng X, Wang S, Zhou X, Cheng L. Development and status of resin composite as dental restorative materials. J Appl Polym Sci 2019;136:48180.ArticlePDF
- 3. Veneziani M. Adhesive restorations in the posterior area with subgingival cervical margins: new classification and differentiated treatment approach. Eur J Esthet Dent 2010;5:50-76.PubMed
- 4. Cardoso MV, de Almeida Neves A, Mine A, Coutinho E, Van Landuyt K, De Munck J, Van Meerbeek B. Current aspects on bonding effectiveness and stability in adhesive dentistry. Aust Dent J 2011;56(Suppl 1):31-44.ArticlePubMed
- 5. Manuja N, Nagpal R, Pandit IK. Dental adhesion: mechanism, techniques and durability. J Clin Pediatr Dent 2012;36:223-234.PubMed
- 6. Kikushima D, Shimada Y, Foxton RM, Tagami J. Micro-shear bond strength of adhesive systems to cementum. Am J Dent 2005;18:364-368.PubMed
- 7. Welbury RR, Murray JJ. A clinical trial of the glass-ionomer cement-composite resin “sandwich” technique in Class II cavities in permanent premolar and molar teeth. Quintessence Int 1990;21:507-512.PubMed
- 8. Andersson-Wenckert IE, van Dijken JW, Hörstedt P. Modified Class II open sandwich restorations: evaluation of interfacial adaptation and influence of different restorative techniques. Eur J Oral Sci 2002;110:270-275.ArticlePubMedPDF
- 9. Kielbassa AM, Philipp F. Restoring proximal cavities of molars using the proximal box elevation technique: Systematic review and report of a case. Quintessence Int 2015;46:751-764.PubMed
- 10. Andersson-Wenckert IE, van Dijken JW, Kieri C. Durability of extensive Class II open-sandwich restorations with a resin-modified glass ionomer cement after 6 years. Am J Dent 2004;17:43-50.PubMed
- 11. Lindberg A, van Dijken JW, Lindberg M. 3-year evaluation of a new open sandwich technique in Class II cavities. Am J Dent 2003;16:33-36.PubMed
- 12. Dietschi D, Spreafico R. Current clinical concepts for adhesive cementation of tooth-colored posterior restorations. Pract Periodontics Aesthet Dent 1998;10:47-54.PubMed
- 13. Grubbs TD, Vargas M, Kolker J, Teixeira EC. Efficacy of direct restorative materials in proximal box elevation on the margin quality and fracture resistance of molars restored with CAD/CAM onlays. Oper Dent 2020;45:52-61.ArticlePubMed
- 14. Vertolli TJ, Martinsen BD, Hanson CM, Howard RS, Kooistra S, Ye L. Effect of deep margin elevation on CAD/CAM-fabricated ceramic inlays. Oper Dent 2020;45:608-617.ArticlePubMedPDF
- 15. Sarfati A, Tirlet G. Deep margin elevation versus crown lengthening: biologic width revisited. Int J Esthet Dent 2018;13:334-356.PubMed
- 16. Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA. PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015;4:1.PubMedPMC
- 17. Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097.ArticlePubMedPMC
- 18. Rosa WL, Piva E, Silva AF. Bond strength of universal adhesives: a systematic review and meta-analysis. J Dent 2015;43:765-776.ArticlePubMed
- 19. Sarkis-Onofre R, Skupien JA, Cenci MS, Moraes RR, Pereira-Cenci T. The role of resin cement on bond strength of glass-fiber posts luted into root canals: a systematic review and meta-analysis of in vitro studies. Oper Dent 2014;39:E31-E44.PubMed
- 20. Aggarwal V, Bhasin SS. Application of calcium silicate materials after acid etching may preserve resin-dentin bonds. Oper Dent 2018;43:E243-E252.ArticlePubMedPDF
- 21. Al-Harbi F, Kaisarly D, Bader D, El Gezawi M. marginal integrity of bulk versus incremental fill class II composite restorations. Oper Dent 2016;41:146-156.ArticlePubMedPDF
- 22. Kumagai RY, Zeidan LC, Rodrigues JA, Reis AF, Roulet JF. Bond strength of a flowable bulk-fill resin composite in class II MOD cavities. J Adhes Dent 2015;17:427-432.PubMed
- 23. Al-Harbi F, Kaisarly D, Michna A, ArRejaie A, Bader D, El Gezawi M. Cervical interfacial bonding effectiveness of class II bulk versus incremental fill resin composite restorations. Oper Dent 2015;40:622-635.ArticlePubMedPDF
- 24. Aggarwal V, Singla M, Yadav S, Yadav H, Ragini . Marginal adaptation evaluation of biodentine and MTA plus in “Open Sandwich” class II restorations. J Esthet Restor Dent 2015;27:167-175.ArticlePubMedPDF
- 25. Koyuturk AE, Tokay U, Sari ME, Ozmen B, Cortcu M, Acar H, Ulker M. Influence of the bulk fill restorative technique on microleakage and microtensile of class II restorations. Pediatr Dent J 2014;24:148-152.Article
- 26. Czarnecka B, Kruszelnicki A, Kao A, Strykowska M, Nicholson JW. Adhesion of resin-modified glass-ionomer cements may affect the integrity of tooth structure in the open sandwich technique. Dent Mater 2014;30:e301-e305.ArticlePubMed
- 27. Campos EA, Ardu S, Lefever D, Jassé FF, Bortolotto T, Krejci I. Marginal adaptation of class II cavities restored with bulk-fill composites. J Dent 2014;42:575-581.ArticlePubMed
- 28. Aggarwal V, Singla M, Yadav S, Yadav H. Effect of flowable composite liner and glass ionomer liner on class II gingival marginal adaptation of direct composite restorations with different bonding strategies. J Dent 2014;42:619-625.ArticlePubMed
- 29. Zaruba M, Wegehaupt FJ, Attin T. Comparison between different flow application techniques: SDR vs flowable composite. J Adhes Dent 2013;15:115-121.PubMed
- 30. de Mattos Pimenta Vidal C, Pavan S, Briso AL, Bedran-Russo AK. Effects of three restorative techniques in the bond strength and nanoleakage at gingival wall of Class II restorations subjected to simulated aging. Clin Oral Investig 2013;17:627-633.ArticlePubMedPDF
- 31. Lefever D, Gregor L, Bortolotto T, Krejci I. Supragingival relocation of subgingivally located margins for adhesive inlays/onlays with different materials. J Adhes Dent 2012;14:561-567.PubMed
- 32. Rodrigues Junior SA, Pin LF, Machado G, Della Bona A, Demarco FF. Influence of different restorative techniques on marginal seal of class II composite restorations. J Appl Oral Sci 2010;18:37-43.ArticlePubMedPMC
- 33. Garcia-Godoy F, Krämer N, Feilzer AJ, Frankenberger R. Long-term degradation of enamel and dentin bonds: 6-year results in vitro vs. in vivo . Dent Mater 2010;26:1113-1118.PubMed
- 34. Fabianelli A, Sgarra A, Goracci C, Cantoro A, Pollington S, Ferrari M. Microleakage in class II restorations: open vs closed centripetal build-up technique. Oper Dent 2010;35:308-313.ArticlePubMedPDF
- 35. Cavalcanti AN, Mitsui FH, Lima AF, Mathias P, Marchi GM. Evaluation of dentin hardness and bond strength at different walls of class II preparations. J Adhes Dent 2010;12:183-188.PubMed
- 36. Bertoldi C, Monari E, Cortellini P, Generali L, Lucchi A, Spinato S, Zaffe D. Clinical and histological reaction of periodontal tissues to subgingival resin composite restorations. Clin Oral Investig 2020;24:1001-1011.ArticlePubMedPDF
- 37. Ferrari M, Koken S, Grandini S, Ferrari Cagidiaco E, Joda T, Discepoli N. Influence of cervical margin relocation (CMR) on periodontal health: 12-month results of a controlled trial. J Dent 2018;69:70-76.ArticlePubMed
- 38. Heintze SD. Systematic reviews: I. The correlation between laboratory tests on marginal quality and bond strength. II. The correlation between marginal quality and clinical outcome. J Adhes Dent 2007;9(Suppl 1):77-106.PubMed
- 39. Francois P, Vennat E, Le Goff S, Ruscassier N, Attal JP, Dursun E. Shear bond strength and interface analysis between a resin composite and a recent high-viscous glass ionomer cement bonded with various adhesive systems. Clin Oral Investig 2019;23:2599-2608.ArticlePubMedPDF
- 40. Moazzami SM, Sarabi N, Hajizadeh H, Majidinia S, Li Y, Meharry MR, Shahrokh H. Efficacy of four lining materials in sandwich technique to reduce microleakage in class II composite resin restorations. Oper Dent 2014;39:256-263.ArticlePubMedPDF
- 41. Heintze S, Forjanic M, Cavalleri A. Microleakage of Class II restorations with different tracers--comparison with SEM quantitative analysis. J Adhes Dent 2008;10:259-267.PubMed
- 42. De Goes MF, Giannini M, Di Hipólito V, Carrilho MR, Daronch M, Rueggeberg FA. Microtensile bond strength of adhesive systems to dentin with or without application of an intermediate flowable resin layer. Braz Dent J 2008;19:51-56.ArticlePubMed
- 43. Baroudi K, Silikas N, Watts DC. Time-dependent visco-elastic creep and recovery of flowable composites. Eur J Oral Sci 2007;115:517-521.ArticlePubMed
- 44. Roggendorf MJ, Krämer N, Appelt A, Naumann M, Frankenberger R. Marginal quality of flowable 4-mm base vs. conventionally layered resin composite. J Dent 2011;39:643-647.ArticlePubMed
- 45. El-Damanhoury H, Platt J. Polymerization shrinkage stress kinetics and related properties of bulk-fill resin composites. Oper Dent 2014;39:374-382.ArticlePubMedPDF
- 46. Moorthy A, Hogg CH, Dowling AH, Grufferty BF, Benetti AR, Fleming GJ. Cuspal deflection and microleakage in premolar teeth restored with bulk-fill flowable resin-based composite base materials. J Dent 2012;40:500-505.ArticlePubMed
- 47. Benetti AR, Havndrup-Pedersen C, Honoré D, Pedersen MK, Pallesen U. Bulk-fill resin composites: polymerization contraction, depth of cure, and gap formation. Oper Dent 2015;40:190-200.PubMed
- 48. Elkaffas AA, Hamama HHH, Mahmoud SH. Do universal adhesives promote bonding to dentin? A systematic review and meta-analysis. Restor Dent Endod 2018;43:e29.ArticlePubMedPMCPDF
- 49. Mahmoud SH, Al-Wakeel ES. Marginal adaptation of ormocer-, silorane-, and methacrylate-based composite restorative systems bonded to dentin cavities after water storage. Quintessence Int 2011;42:e131-e139.PubMed
- 50. Moszner N, Salz U, Zimmermann J. Chemical aspects of self-etching enamel-dentin adhesives: a systematic review. Dent Mater 2005;21:895-910.ArticlePubMed
- 51. Sattabanasuk V, Shimada Y, Tagami J. The bond of resin to different dentin surface characteristics. Oper Dent 2004;29:333-341.PubMed
- 52. Cardoso PC, Lopes GC, Vieira LC, Baratieri LN. Effect of solvent type on microtensile bond strength of a total-etch one-bottle adhesive system to moist or dry dentin. Oper Dent 2005;30:376-381.PubMed
- 53. Reis A, Loguercio AD. A 36-month clinical evaluation of ethanol/water and acetone-based etch-and-rinse adhesives in non-carious cervical lesions. Oper Dent 2009;34:384-391.ArticlePubMedPDF
- 54. Bhadra D, Shah NC, Rao AS, Dedania MS, Bajpai N. A 1-year comparative evaluation of clinical performance of nanohybrid composite with Activa™ bioactive composite in Class II carious lesion: a randomized control study. J Conserv Dent 2019;22:92-96.PubMedPMC
- 55. André CB, Chan DC, Giannini M. Antibacterial-containing dental adhesives’ effects on oral pathogens and on Streptococcus mutans biofilm: current perspectives. Am J Dent 2018;31:37B-41B.PubMed
REFERENCES
Tables & Figures
REFERENCES
Citations

- Influence of thickness and base material in class II restorations with nanofilled composites: finite element study
Fredy Hugo Cruzado-Oliva, Alexander Vega-Anticona, David Arturo Ortiz-Diaz, Heber Isac Arbildo-Vega, Franz Tito Coronel-Zubiate
Frontiers in Dental Medicine.2026;[Epub] CrossRef - An In Vitro Evaluation of Novel Bioactive Liner's Effect on Marginal Adaptation of Class II Composite Restorations: A Scanning Electron Microscope Analysis
Girija S Sajjan, Naveena Ponnada, Praveen Dalavai, Madhu Varma Kanumuri, Venkata Karteek Varma Penmatsa, B V Sindhuja
World Journal of Dentistry.2025; 15(9): 749. CrossRef - Effect of Cervical Margin Relocation With Different Injectable Restorative Materials on Fracture Resistance of Molars Received MOD CAD/CAM Onlay Restorations
Basema N. Roshdy, Radwa I. Eltoukhy, Ashraf I. Ali, Salah Hasab Mahmoud
Journal of Esthetic and Restorative Dentistry.2025; 37(6): 1522. CrossRef - Short dentin etching with universal adhesives: effect on bond strength and gingival margin adaptation
Hoda Saleh Ismail, Hanan Ahmed Nabil Soliman
BMC Oral Health.2025;[Epub] CrossRef - Awareness and Practice of Deep Margin Elevation among Dental Practitioners in India: A Cross-Sectional Survey
Mythri Padaru, Preethesh Shetty, Namith Rai, Raksha Bhat
Pesquisa Brasileira em Odontopediatria e Clínica Integrada.2025;[Epub] CrossRef - Effect of surface treatment on glass ionomers in sandwich restorations: a systematic review and meta-analysis of laboratory studies
Hoda S. Ismail, Ashraf Ibrahim Ali, Franklin Garcia-Godoy
Restorative Dentistry & Endodontics.2025; 50(2): e13. CrossRef - Do irrigation solutions effect bond strength of composite resin to deep margin elevation material? An in-vitro study
Şeref Nur Mutlu, Yasemin Derya Fidancıoğlu, Hatice Büyüközer Özkan, Hayriye Esra Ülker
BMC Oral Health.2025;[Epub] CrossRef - Two-year evaluation of periodontal parameters following deep-margin-elevation and CAD/CAM partial lithium disilicate restorations – a prospective controlled clinical trial
Tim Hausdörfer, Philipp Kanzow, Tina Rödig, Annette Wiegand, Clemens Lechte
Journal of Dentistry.2025; 160: 105901. CrossRef - Deep Margin Elevation: Current Evidence and a Critical Approach to Clinical Protocols—A Narrative Review
Athanasios Karageorgiou, Maria Fostiropoulou, Maria Antoniadou, Eftychia Pappa
Adhesives.2025; 1(3): 10. CrossRef - Comparative Micro-CT Analysis of Internal Adaptation and Closed Porosity of Conventional Layered and Thermoviscous Bulk-Fill Resin Composites Using Total-Etch or Universal Adhesives
Dóra Jordáki, Virág Veress, Tamás Kiss, József Szalma, Márk Fráter, Edina Lempel
Polymers.2025; 17(15): 2049. CrossRef - Effect of different restorative systems and aging on marginal adaptation of resin composites to deep proximal margins
Hoda S. Ismail, Ashraf I. Ali
Journal of Esthetic and Restorative Dentistry.2024; 36(2): 346. CrossRef - Management of subgingival proximal defects
Jagruti Mutalikdesai, K. C. Dhaniba, Supriya Choudhary, Promila Verma, Rhythm Bains
Asian Journal of Oral Health and Allied Sciences.2024; 14: 15. CrossRef - Effect of Deep Margin Elevation on the Pulpal and Periodontal Health of Teeth: A Systematic Review
S Srirama, S Jain, B Arul, K Prabakar, V Natanasabapathy
Operative Dentistry.2024; 49(4): 388. CrossRef - Alternative Direct Restorative Materials for Dental Amalgam: A Concise Review Based on an FDI Policy Statement
Gottfried Schmalz, Falk Schwendicke, Reinhard Hickel, Jeffrey A. Platt
International Dental Journal.2024; 74(4): 661. CrossRef - Comparison of the stress distribution in base materials and thicknesses in composite resin restorations
Min-Kwan Jung, Mi-Jeong Jeon, Jae-Hoon Kim, Sung-Ae Son, Jeong-Kil Park, Deog-Gyu Seo
Heliyon.2024; 10(3): e25040. CrossRef - Influence of curing mode and aging on the bonding performance of universal adhesives in coronal and root dentin
Hoda Saleh Ismail, Ashraf Ibrahim Ali, Mohamed Elshirbeny Elawsya
BMC Oral Health.2024;[Epub] CrossRef - CLINICAL ASSESSMENT OF THE EFFECTIVENESS OF ESTHETIC RESTORATION OF ANTERIOR TEETH
Lyudmila Tatintsyan, Minas Poghosyan, Armen Shaginyan, Hovhannes Gevorgyan, Biayna Hoveyan, Tatevik Margaryan, Arsen Kupelyan
BULLETIN OF STOMATOLOGY AND MAXILLOFACIAL SURGERY.2023; : 16. CrossRef - Deep margin elevation—Present status and future directions
Florin Eggmann, Jose M. Ayub, Julián Conejo, Markus B. Blatz
Journal of Esthetic and Restorative Dentistry.2023; 35(1): 26. CrossRef
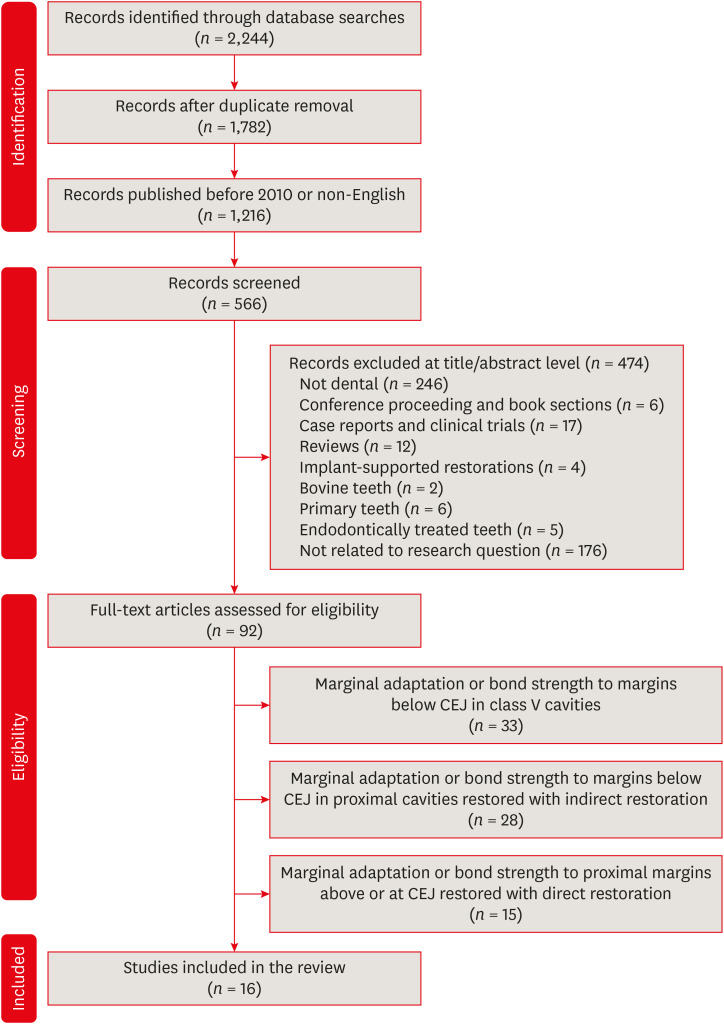
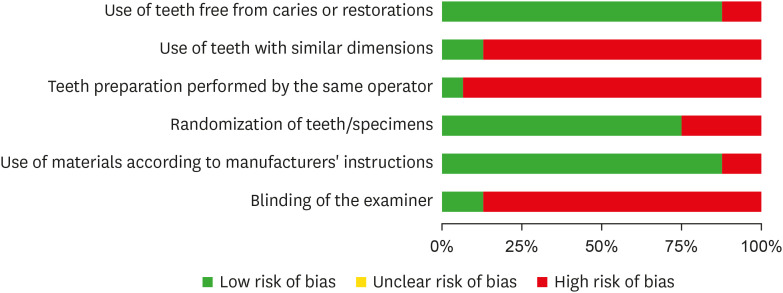
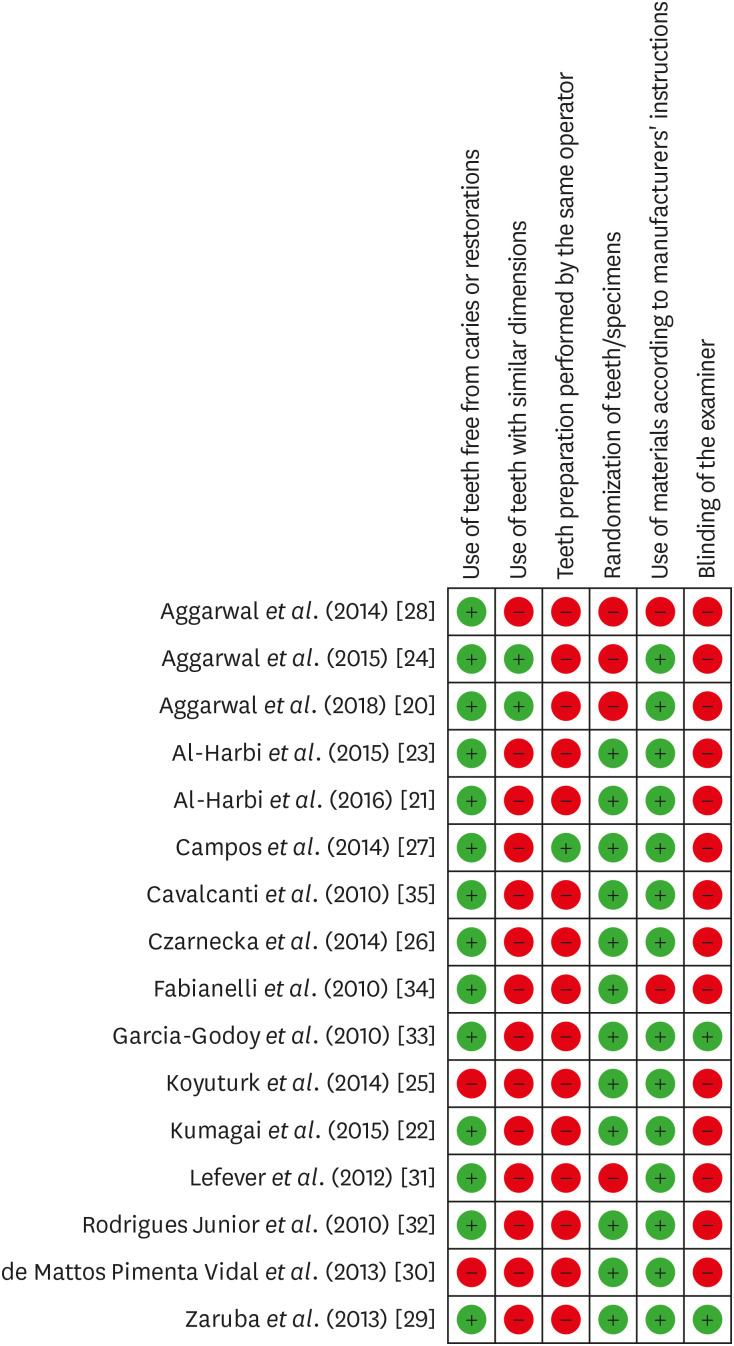
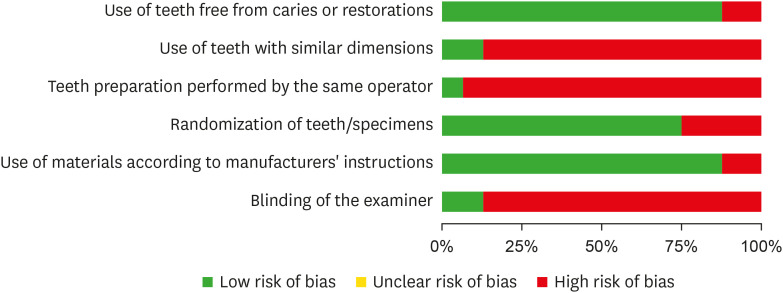
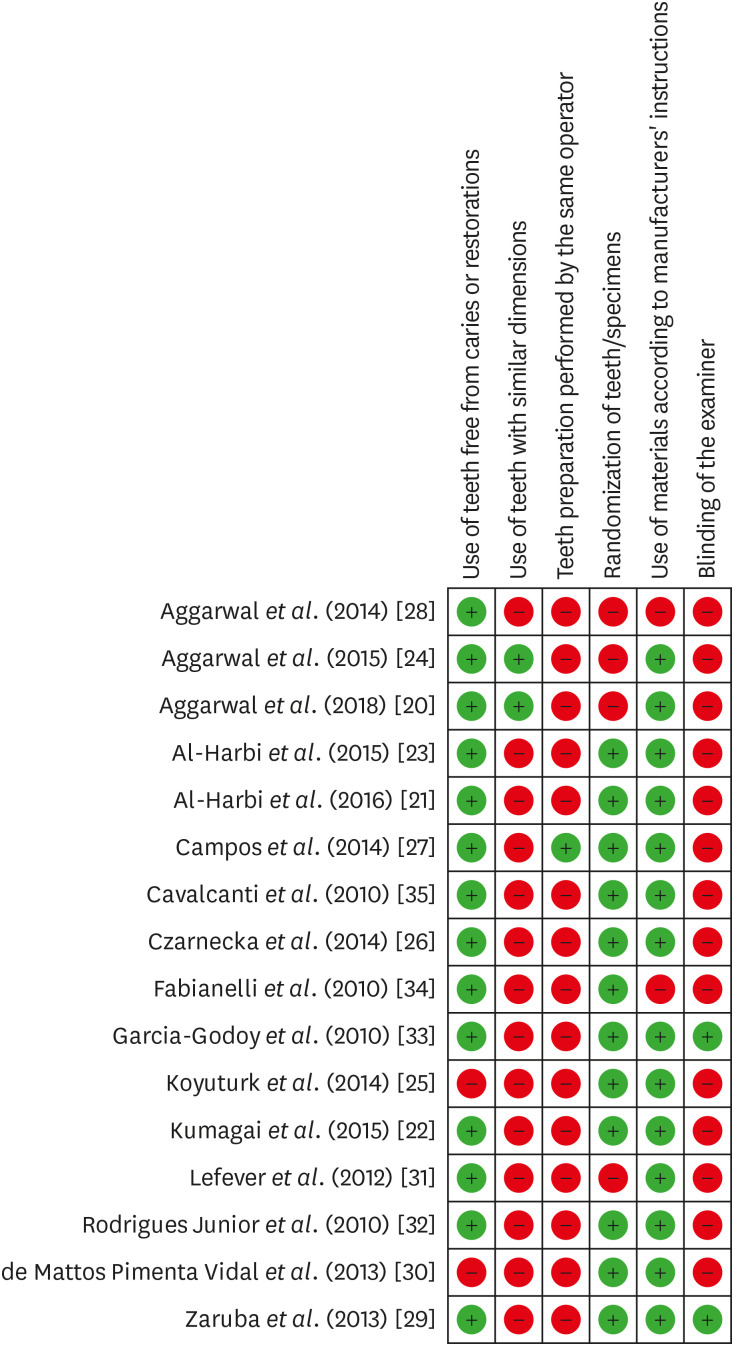
Figure 1
Figure 2
Figure 3
Assessment of sample sizes, test types, and aging methodologies
| Study | Sample type and size and cavity type | Test type | Aging methodology |
|---|---|---|---|
| Aggarwal and Bhasin [ | 80 molars | Marginal adaptation | Storage in PBS for 6 mon |
| Class II | |||
| Al-Harbi | 91 premolars | Marginal adaptation | 5,000 TC (55°C ± 2°C) (50°C ± 2°C), 1,000 MLC |
| Class II on each side | Margins assessment by FDI ranking | ||
| Kumagai | 44 molars | μTBS | |
| Complex Class II | Failure mode analysis | ||
| Al-Harbi | 91 premolars | μTBS | 5,000 TS (55°C ± 2°C) (50°C ± 2°C), 1,000 MLC |
| Class II on each side | Failure mode analysis | ||
| Marginal adaptation | |||
| Aggarwal | 60 molars | Marginal adaptation | 150,000 MLC, 3 mon PBS storage |
| Class II | |||
| Koyuturk | 60 premolars | μTBS | 10,000 TC (5°C–50°C), 50,000 MLC |
| Class II | Failure mode analysis | ||
| Czarnecka | 10 molars and premolars | Marginal and internal adaptation | |
| Class II on each side | |||
| Campos | 40 molars | Marginal adaptation | 600 TC (5°C–50°C) and 240,000 MLC |
| Class II | |||
| Aggarwal | 90 molars | Marginal adaptation | 150,000 MLC |
| Class II | |||
| Zaruba | 30 molars | Marginal adaptation | 6,000 TC (5°C–50°C) and 1.2 × 106 MLC |
| Class II on each side | |||
| de Mattos Pimenta Vidal | 72 premolars | μTBS | 3,000 TC (20°C–80°C) and 500,000 MLC |
| Class II on each side | |||
| Lefever | 88 molars | Marginal adaptation | |
| Class II | |||
| Rodrigues Junior | 32 molars | Marginal adaptation | 500 TC (5°C–55°C) |
| Class II on each side | |||
| Garcia-Godoy | 32 molars | Marginal adaptation | Half of the specimens were stored in water for 2,190 days, the other half were subjected to 2,500 TC (5°C–55°C) and 100,000 MLC |
| Class II | |||
| Fabianelli | 30 molars | Marginal adaptation | 500 TC (5°C–55°C) |
| Class II | |||
| Cavalcanti | 36 molars | μTBS | |
| Complex Class II |
PBS, phosphate-buffered saline; TC, thermal cycle; MLC, mechanical loading cycle; μTBS, micro-tensile bond strength.
Scientific categories, brand names of restorative materials, and adhesives used
| Study | Restorative materials used | Adhesives used |
|---|---|---|
| Aggarwal and Bhasin [ | Nanofilled flowable composite (Filtek Z350 XT) | Ethanol-based ER adhesive (Single Bond) |
| Microhybrid flowable composite (Esthet-X Flow) | Acetone-based ER adhesive (Prime & Bond NT) | |
| Nanofilled RC (Z350) | ||
| CSM (ProRoot MTA White) | ||
| Al-Harbi | Microhybrid heavy body (Tetric Ceram HB) | ER adhesives (Tetric N-Bond, ExciTE F) |
| Microhybrid flowable composite (Tetric EvoFlow) | SE adhesives (Tetric N-Bond Self-Etch, AdheSE) | |
| Bulk-fill flowable composite (SDR) | Silorane-specific adhesive (P90 System) | |
| Bulk-fill low-shrinkage composite (SonicFill Composite) | ||
| Bulk-fill RC (Tetric N-Ceram Bulk Fill, Tetric EvoCeram Bulk Fill) | ||
| Low-shrink silorane-based composite (Filtek P90) | ||
| Kumagai | Bulk-fill flowable composite (SDR) | Two-step ER adhesives (XP Bond) |
| Nanofilled RC (Z350) | ||
| Al-Harbi | Microhybrid heavy body (Tetric Ceram HB) | ER adhesive (Tetric N-Bond, ExciTE F) |
| Microhybrid flowable composite (Tetric EvoFlow) | SE adhesive (Tetric N-Bond Self-Etch, AdheSE) | |
| Bulk-fill flowable composite (SDR) | Silorane-specific adhesive (P90 System) | |
| Bulk-fill low-shrinkage composite (SonicFill Composite) | ||
| Bulk-fill RC (Tetric N-Ceram Bulk Fill, Tetric EvoCeram Bulk Fill) | ||
| Low-shrink silorane-based composite (Filtek P90) | ||
| Aggarwal | CSMs (Biodentine, MTA Plus) | ER adhesive (Single Bond) |
| Nano RMGI (Ketac N100) | Two-step SE adhesive (One Coat Self Etching Bond) | |
| Nanofilled RC (Z350) | ||
| Nanohybrid RC (Synergy D6 Universal) | ||
| Koyuturk | Hybrid composite (ÆLITE LS Posterior/Bisco) | ER adhesive (Prime&Bond NT) |
| Bulk-fill flowable composite (SureFil SDR flow/Dentsply) | SE adhesive (Clearfil S3 Bond) | |
| Czarnecka | GIC (Ketac Molar or Fuji IX) | ER adhesive |
| Nano RMGI and RMGI (N100 or Fuji IILC) | ||
| Microhybrid RC (Filtek Z250) | ||
| Campos | Flowable bulk-fill composites (Venus Bulk Fill, Surefill SDR, Tetric EvoCeram Bulk Fill) | ER adhesive (Optibond FL) |
| Nano-hybrid RC (Venus, Tetric EvoCeram) | ||
| Nano-ceramic RC (Ceram-X) | ||
| Bulk-fill low-shrinkage composite (SonicFill) | ||
| Aggarwal | Nanofilled flowable RC (Filtek Z350, Synergy D6 flow) | ER adhesive (Single Bond) |
| Nano RMGI (N100) | One-step SE adhesive (Adper Easy Bond) | |
| Nanohybrid RC (Z350, Synergy D6 Universal) | Two-step SE adhesive (One Coat) | |
| Zaruba | Nanohybrid RC (Ceram X mono) | ER adhesive (XP Bond) |
| Flowable bulk-fill composites (Surefill SDR) | ||
| Microhybrid flowable RC (x-flow) | ||
| de Mattos Pimenta Vidal | Nanofilled RC (Filtek Supreme Plus Universal Restorative) | ER adhesive (Adper Single Bond Plus) |
| Nanofilled flowable RC (Filtek Supreme Plus Flowable Restorative) | ||
| RMGIC (Vitrebond Plus) | ||
| Lefever | Low-shrink silorane-based composite (Filtek Silorane) | Silorane-specific adhesive (P90 System) |
| Microhybrid composite (CLEARFIL AP-X) | SE adhesive (Clearfil Protect Bond) | |
| Nanofilled RC (Clearfil Majesty Posterior) | ||
| Self-adhering RC (Vertise Flow) | ||
| Self-adhesive resin cement (RelyX Unicem) | ||
| Nanohybrid flowable RC (Clearfil Majesty Flow) | ||
| Flowable bulk-fill composite (Surefill SDR) | ||
| Rodrigues Junior | Microhybrid composite (Z250) | ER adhesive (Single Bond) |
| Dental amalgam (Logic Plus) | ||
| RMGIC (Vitrebond) | ||
| Garcia-Godoy | Nanohybrid composite (Tetric Ceram and Grandio voco) | SE adhesives (Syntac, Solobond M) |
| Fabianelli | Microhybrid RC (Estelite Sigma) | SE adhesive (Bond Force) |
| Microhybrid flowable RC (Palfique Estelite LV) | ||
| Cavalcanti | Microhybrid composite (Z250) | ER adhesive (Single Bond Plus) |
| Two-step SE adhesive (Clearfil SE Bond) | ||
| One-step SE adhesive (Adper Prompt) |
RC, resin composite; CSM, calcium silicate material; MTA, mineral trioxide aggregate; ER, etch and rinse; SE, self-etch; RMGI, resin-modified glass ionomer; GIC, glass ionomer cement.
Assessment of marginal adaptation evaluation methodologies
| Study | F/P of margins prior to testing | Direct or replica | Examination method | No. of margins assessed | Criteria for evaluation |
|---|---|---|---|---|---|
| Aggarwal and Bhasin [ | Immediate + cleaning with H3PO4 for 5 seconds | Replica | (65–1,500×) SEM | Cervical dentin | % CM |
| Al-Harbi | Immediate | Replica | 200× SEM | Enamel and dentin gingival margins | % CM + FDI ranking |
| Al-Harbi | Immediate | Direct | 1,200× SEM | Enamel and dentin gingival margins | Measuring maximum gap in microns |
| Aggarwal | Immediate | Direct | (25–300×) SEM | Cervical dentin | % CM |
| Czarnecka | Delayed | Direct | 100× Metallographic light microscope | Cervical dentin + internal adaptation | Adequate or inadequate margins |
| Campos | Immediate | Replica before and after aging | 200× SEM | Occlusal, proximal enamel and cervical dentin | % CM |
| Aggarwal | Immediate | Direct | 200× SEM | Cervical dentin | % CM |
| Zaruba | Immediate | Replica before and after aging | 200× SEM | Proximal enamel, proximal and cervical dentin | % CM |
| Lefever | Immediate | Replica | 200× SEM | Proximal enamel, proximal and cervical dentin | % CM |
| Rodrigues Junior | Delayed | Replica | 200× SEM | Enamel and dentin gingival margins | Qualitative analysis |
| Garcia-Godoy | Immediate | Replica before and after aging | 200× SEM | Proximal enamel, proximal and cervical dentin | % CM |
| Fabianelli | -* | Replica | (25–1,400×) SEM | Cervical dentin | Qualitative analysis |
F/P, finishing and polishing; SEM, scanning electron microscopy; % CM, percentage of continuous margin to the total margin length.
*The study did not specify this item.
Assessment of microtensile bond strength testing methodologies
| Study | Testing machine | Crosshead speed | Shape and no. of bonded specimens | Cross-section of bonded specimens | Types of margins and walls evaluated | Method of failure analysis | Scoring of failure type |
|---|---|---|---|---|---|---|---|
| Kumagai | UTM | 1 mm/min | 3 Rectangular S/R | 1 mm2 | Dentin/cementum | 50× Light microscope | 1. Cohesive in dentin |
| 2. Cohesive in resin | |||||||
| 3. Adhesive | |||||||
| Al-Harbi | UTM | 0.5 mm/min | 2 Hourglass S/R | 0.8 mm2 | Enamel and Dentin/cementum | 40× Stereomicroscope + 500× SEM | As above + mixed |
| Koyuturk | -* | - | Rectangular | 1 mm2 | Dentin/cementum | 40× Stereomicroscope | As above + mixed |
| de Mattos Pimenta Vidal | Microtensile tester | 1 mm/min | 2 Hourglass S/R | 1 mm2 | Dentin/cementum | - | - |
| Cavalcanti | UTM | 0.5 mm/min | 3 Hourglass S/R | 1 mm2 | Pulpal, axial and gingival preparation walls | - | Scoring of specimens with premature failure |
UTM, universal testing machine; S/R, specimen/restoration; SEM, scanning electron microscopy.
*The study did not mention this information.
PBS, phosphate-buffered saline; TC, thermal cycle; MLC, mechanical loading cycle; μTBS, micro-tensile bond strength.
RC, resin composite; CSM, calcium silicate material; MTA, mineral trioxide aggregate; ER, etch and rinse; SE, self-etch; RMGI, resin-modified glass ionomer; GIC, glass ionomer cement.
F/P, finishing and polishing; SEM, scanning electron microscopy; % CM, percentage of continuous margin to the total margin length.
*The study did not specify this item.
UTM, universal testing machine; S/R, specimen/restoration; SEM, scanning electron microscopy.
*The study did not mention this information.

 KACD
KACD
 ePub Link
ePub Link Cite
Cite

