Search
- Page Path
- HOME > Search
- Fifty-year follow-up of dens invaginatus treated by nonsurgical and surgical endodontic treatments: a case report
- Qais Arow, Eyal Rosen, Galit Sela, Shlomo Elbahary, Igor Tsesis
- Received April 9, 2025 Accepted August 26, 2025 Published online December 18, 2025
- DOI: https://doi.org/10.5395/rde.2026.51.e1 [Epub ahead of print]
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - This case report presents a lateral maxillary incisor with dens invaginatus (DI) type IIIb that was treated both nonsurgically and surgically over 50 years. Treatment of teeth with DI can be challenging. Suggested options may include nonsurgical root canal treatment, endodontic surgery, or extraction. In this case report, a 13-year-old patient with a lateral maxillary incisor with DI type IIIb was treated by nonsurgical root canal treatment, modern endodontic surgery, and reoperation over the course of 50 years. There was complete healing at the last follow-up, 11 years after the reoperation. Correct diagnosis and proper treatment using modern endodontic techniques can enable teeth with DI to survive throughout the life span of the patient.
- 426 View
- 34 Download

- Effect of quality of radiographs taken during root canal treatment on technical quality of root canal fillings and endodontic outcome
- Jia Min Ng, Yan Yee Lee, Prashanti Chippagiri, Elaheh Ahanin, Abhishek Parolia
- Restor Dent Endod 2025;50(1):e3. Published online January 7, 2025
- DOI: https://doi.org/10.5395/rde.2025.50.e3
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Objectives
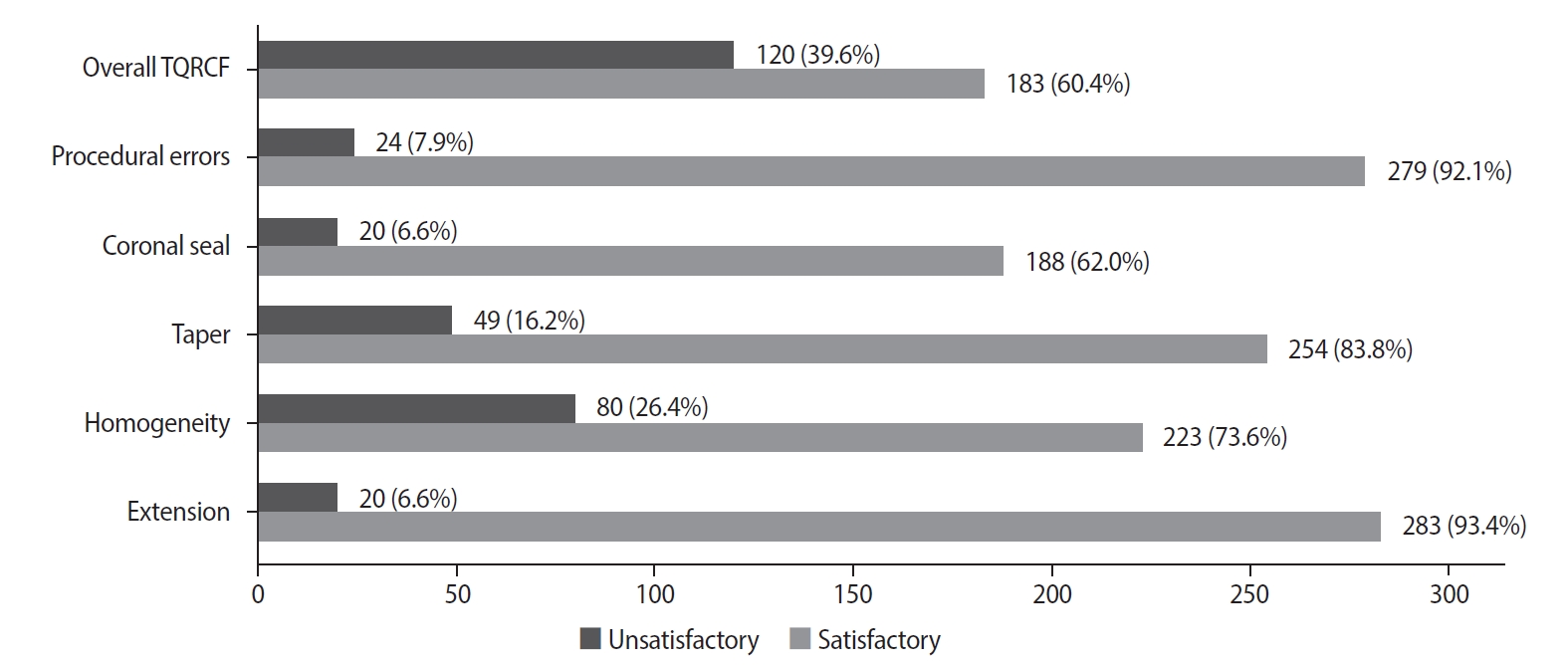
This study evaluated the number and quality of working length (WL) and master cone (MC) radiographs taken during root canal treatment by dental undergraduates, and their associations with the technical quality of root canal fillings (TQRCF) and endodontic outcomes (EO).
Methods
A retrospective evaluation of radiographs from 303 root canal-treated teeth in 231 patients was conducted, with 72 patients attending recall visits to assess EO. The chi-square and one-way analysis of variance tests were performed.
Results
A total of 505 WL and 557 MC radiographs were reviewed, with 72.9% and 75% deemed satisfactory, respectively. Satisfactory TQRCF was achieved in 60.4% of cases. Significant associations were found between the extension of the file in WL and gutta-percha in MC radiographs and TQRCF (p = 0.000). Misinterpretation of these radiographs resulted in poor TQRCF. Furthermore, 64.2% of teeth had satisfactory EO. A significant relationship was noted between the quality of MC radiographs and both TQRCF (p = 0.043) and EO (p = 0.003).
Conclusions
Unsatisfactory MC radiographs were linked to poor TQRCF and unfavorable EO. Regular radiographic training is recommended to enhance EO. -
Citations
Citations to this article as recorded by- Assessment of radiographic errors and repetition rates in undergraduate endodontic education: a retrospective clinical study
Marwa Ameen, Abdul Rahman Saleh, Dunia Alhadi, Manal Almaslamani
The Saudi Dental Journal.2025;[Epub] CrossRef - Application of Periapical Radiography in Root Canal Treatment: A Literature Review
Jennifer Lois Violita Malau, Keizha Allysia Nabila, Widiani Harrista, Regina Amara Ginting, Tassa Kusuma Arya Putri, Jatu Rachel Keshena
Acta Odontologica Indonesia.2025; 1(2): 49. CrossRef
- Assessment of radiographic errors and repetition rates in undergraduate endodontic education: a retrospective clinical study
- 11,142 View
- 249 Download
- 1 Web of Science
- 2 Crossref

- Prevalence of apical periodontitis and quality of root canal treatment in an adult Kuwaiti sub-population: a cross-sectional study
- Abdulrahman A. Alhailaa, Saad A Al-Nazhan, Mazen A Aldosimani
- Restor Dent Endod 2024;49(2):e16. Published online March 22, 2024
- DOI: https://doi.org/10.5395/rde.2024.49.e16
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives This cross-sectional study evaluated the prevalence of apical periodontitis (AP) and the technical quality of root canal fillings in an adult Kuwaiti subpopulation using cone-beam computed tomography (CBCT) images.
Materials and Methods Two experienced examiners analyzed 250 CBCT images obtained from Kuwaiti patients aged 15–65 years who attended government dental specialist clinics between January 2019 and September 2020. The assessment followed the radiographic scoring criteria proposed by De Moor for periapical status and the technical quality of root canal filling. Chi-square and Fisher’s exact tests were used for statistical analysis, with significance level set at
p < 0.05.Results Among the 2,762 examined teeth, 191 (6.91%) exhibited radiographic signs of AP, and 176 (6.37%) had undergone root canal filling. AP prevalence in root canal-treated teeth was 32.38%, with a significant difference between males and females. Most of the endodontically treated teeth exhibited adequate root canal filling (71.5%).
Conclusions The study demonstrated a comparable prevalence of AP and satisfactory execution of root canal treatment compared to similar studies in different countries.
-
Citations
Citations to this article as recorded by- A Retrospective Study of CBCT-Based Detection of Endodontic Failures and Periapical Lesions in a Romanian Cohort
Oana Andreea Diaconu, Lelia Mihaela Gheorghiță, Anca Gabriela Gheorghe, Mihaela Jana Țuculină, Maria Cristina Munteanu, Cătălina Alexandra Iacov, Virginia Maria Rădulescu, Mihaela Ionescu, Adina Andreea Mirea, Carina Alexandra Bănică
Journal of Clinical Medicine.2025; 14(18): 6364. CrossRef
- A Retrospective Study of CBCT-Based Detection of Endodontic Failures and Periapical Lesions in a Romanian Cohort
- 4,659 View
- 81 Download
- 1 Web of Science
- 1 Crossref

- Incidence of interappointment emergencies in multiple-visit root canal treatments performed with or without intracanal medicament by undergraduate students
- Annemarie Baaij, Corine Mirjam Visscher, Manon Jansen, Ahmet Rifat Özok
- Restor Dent Endod 2023;48(3):e31. Published online August 14, 2023
- DOI: https://doi.org/10.5395/rde.2023.48.e31
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives This retrospective cohort study examined the incidence of interappointment emergencies during multiple-visit molar root canal treatments conducted by undergraduate students. Treatments performed without the use of intracanal medicament were compared to treatments that incorporated calcium hydroxide as an intracanal medicament.
Materials and Methods Interappointment emergencies, defined as instances of pain or swelling that required the patient to make an unscheduled follow-up visit, were recorded for up to 2 months after the intervention. To avoid the influence of obturation on the observed incidence of emergency visits, only unscheduled visits occurring between the start and end of the root canal treatment were included.
Results Of the 719 patients included in this study, 77 (10.7%) were recorded as experiencing interappointment emergencies. Of these emergencies, 62% occurred within 2 weeks following the most recent intervention. In the group of patients who did not receive intracanal medicament, the incidence of interappointment emergencies was 11.9% (46 of 385 patients). In comparison, this rate was 9.3% (31 of 334 patients) among those who received calcium hydroxide as an intracanal medicament (odds ratio, 1.33; 95% confidence interval, 0.82–2.15;
p = 0.249).Conclusions Interappointment emergencies may arise at any point during root canal treatment, but they most commonly occur within the first 2 weeks following intervention. The omission of intracanal medicament in multiple-visit molar root canal treatments, performed by undergraduate students, did not significantly increase the incidence of these emergencies.
-
Citations
Citations to this article as recorded by- An Observational Study on Pain Occurrence After Root Canal Treatment: Role of Operator Experience When Using a Bioceramic Sealer
Mihai Merfea, Ioana Sofia Pop-Ciutrila, Mindra Eugenia Badea, Ada Gabriela Delean, Oana Cimponeriu, Razvan Corneliu Pop, Maria Peter, Iulia Clara Badea, Sanda Ileana Cimpean
Journal of Clinical Medicine.2025; 14(13): 4558. CrossRef
- An Observational Study on Pain Occurrence After Root Canal Treatment: Role of Operator Experience When Using a Bioceramic Sealer
- 4,010 View
- 43 Download
- 1 Web of Science
- 1 Crossref

- Outcome of endodontic treatments performed by Brazilian undergraduate students: 3- to 8-year follow up
- Jéssica Gabriele da Rocha, Isabella Marian Lena, Jéssica Lopes Trindade, Gabriela Salatino Liedke, Renata Dornelles Morgental, Carlos Alexandre Souza Bier
- Restor Dent Endod 2022;47(3):e34. Published online August 18, 2022
- DOI: https://doi.org/10.5395/rde.2022.47.e34
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives This study aimed to evaluate the success rate of endodontic treatments performed by undergraduate students and the factors associated with the outcome.
Materials and Methods A follow-up of 3 to 8 years after root canal filling was carried out in 91 patients. At the follow-up visits, medical and dental history questionnaires were applied along with clinical and radiographic examinations. Data collected in the clinical exam included: the presence of pain, swelling, sinus tract, mobility, tenderness to palpation and percussion, periodontal probing profile, and type/quality of coronal restoration. Postoperative and follow-up radiographs were digitalized and analyzed by 2 trained and calibrated examiners to assess periapical healing. The treatment outcome was based on strict clinical and radiographic criteria and classified as success (absence of any clinical and radiographic sign of apical periodontitis) or failure (other combination). Logistic regression was used to investigate the impact of clinical and radiographic variables on endodontic treatment outcomes at a 5% significance level.
Results The success rate of endodontic treatments was 60.7%. The only risk factor significantly associated with failure was the presence of a periapical lesion on the postoperative radiograph (odds ratio, 3.35; 95% confidence interval, 1.17–9.54).
Conclusions The success rate of endodontic treatments performed by undergraduate students was low and was jeopardized by the presence of a periapical lesion on the postoperative radiograph.
-
Citations
Citations to this article as recorded by- Effect of quality of radiographs taken during root canal treatment on technical quality of root canal fillings and endodontic outcome
Jia Min Ng, Yan Yee Lee, Prashanti Chippagiri, Elaheh Ahanin, Abhishek Parolia
Restorative Dentistry & Endodontics.2025; 50(1): e3. CrossRef - Outcomes of root canal treatment performed by undergraduate students: A systematic review and meta‐analysis
Philip Y.‐H. Chien, Sepanta Hosseinpour, Ove A. Peters, Christine I. Peters
International Endodontic Journal.2025;[Epub] CrossRef - Factors Influencing the Long-Term Survival and Success of Endodontically Treated and Retreated Teeth: An Ambispective Study at an Educational Hospital
Reem Barakat, Rahaf Almohareb, Ghaliah Alsawah, Hadeel Busuhail, Shahad A. Alshihri, Ghadah T. Alrashid, Ghadeer Y. Alotaibi, Mamata Hebbal
Journal of Clinical Medicine.2025; 14(21): 7826. CrossRef - A bibliometric comparison of undergraduate and postgraduate endodontic education publications: The topics, trends, and challenges
Jinglan Zhang, Xiaowei Liu, Lei Yang, Yiran Wang, Dingming Huang, Xuelian Tan
Journal of Dental Education.2023; 87(12): 1661. CrossRef
- Effect of quality of radiographs taken during root canal treatment on technical quality of root canal fillings and endodontic outcome
- 4,653 View
- 41 Download
- 5 Web of Science
- 4 Crossref

- Clinical and radiographic outcomes of regenerative endodontic treatment performed by endodontic postgraduate students: a retrospective study
- Hadi Rajeh Alfahadi, Saad Al-Nazhan, Fawaz Hamad Alkazman, Nassr Al-Maflehi, Nada Al-Nazhan
- Restor Dent Endod 2022;47(2):e24. Published online May 9, 2022
- DOI: https://doi.org/10.5395/rde.2022.47.e24
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
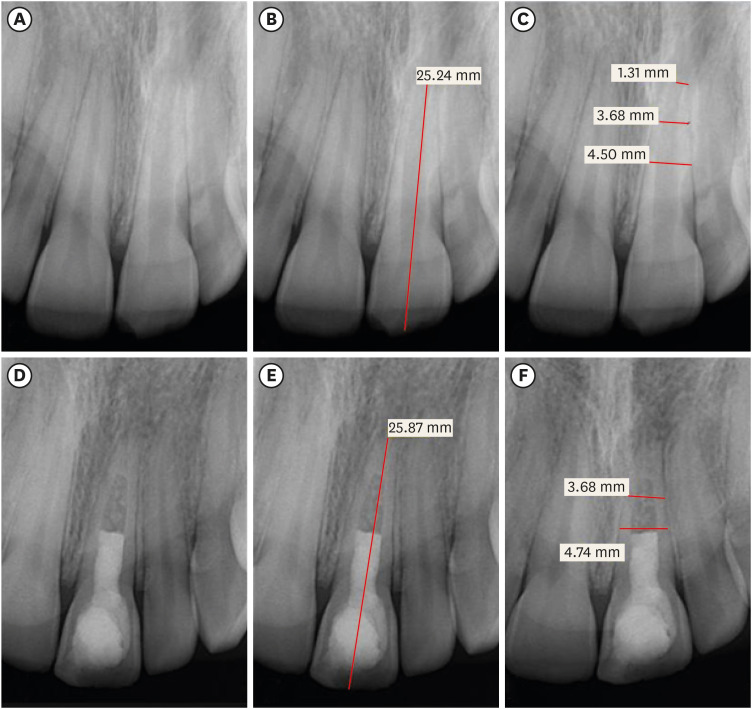
ePub Objectives Regenerative endodontic treatment is a clinical procedure aimed at biologically regenerating damaged root canal tissue of immature permanent teeth. This study aimed to report the outcomes of regenerative endodontic treatment performed by endodontic postgraduate students.
Materials and Methods Clinical and radiographic data of 27 patients, aged 10–22 years, who underwent regenerative treatment of immature permanent teeth from 2015 to 2019 were followed up, wherein clinical and radiographic examinations were performed for each patient. Postoperative success rate and tooth survival were analyzed, and the postoperative radiographic root area changes were quantified.
Results A total of 23 patients attended the dental appointments, showing that all teeth survived and were asymptomatic. Specifically, 7 periapical pathosis cases were completely healed, 12 were incompletely healed, and 4 cases failed. Moreover, significant differences were found between discolored and non-discolored teeth, and between the presence or absence of periapical radiolucency. Additionally, 3 anterior teeth showed complete closure of the apical foramen, while the apical foramen width was reduced in 17 teeth and failed in 3 teeth. Root length was also found to have been increased in 7 anterior and 4 posterior teeth, and the average length ranged from 4.00–0.63 mm in the anterior teeth, 2.85–1.48 mm of the mesial root, and 2.73–2.16 mm of the molar teeth distal root. Furthermore, calcified tissue deposition was observed in 7 teeth.
Conclusions A favorable outcome of regenerative endodontic treatment of immature permanent teeth with necrotic pulp was achieved with a high survival rate.
-
Citations
Citations to this article as recorded by- Pre‐Operative Factors on Prognosis of Regenerative Endodontic Procedures: A Systematic Review and Meta‐Analysis
Filipe Colombo Vitali, Alexandre Henrique dos Reis‐Prado, Pablo Silveira Santos, Ana Paula Portes Zeno, Patrícia de Andrade de Risso, Lucianne Cople Maia, Francine Benetti, Cleonice da Silveira da Teixeira
International Endodontic Journal.2025; 58(12): 1814. CrossRef - Clinical, radiographic, and biomarker perspectives of low-level laser therapy during regenerative endodontic procedures in necrotic immature young teeth: a randomized clinical study
Pragya Pandey, Neha Jasrasaria, Ramesh Bharti, Rakesh Kumar Yadav, Monika Kumari, Abinia Vaishnavi, Rahul Pandey
Lasers in Medical Science.2025;[Epub] CrossRef - Allogeneic Bone Marrow Mesenchymal Stromal Cell Transplantation Induces Dentin Pulp Complex-like Formation in Immature Teeth with Pulp Necrosis and Apical Periodontitis
Jose Francisco Gomez-Sosa, José E. Cardier, Olga Wittig, Dylana Díaz-Solano, Eloisa Lara, Kharelys Duque, Giselle Ramos-González
Journal of Endodontics.2024; 50(4): 483. CrossRef - Radiographic assessment of dental post and core placement at different educational levels in an undergraduate student clinic: a 4-year retrospective study
Turki Alshehri, Nourhan M. Aly, Raand Altayyar, Deena Alghamdi, Shahad Alotaibi, Passent Ellakany
F1000Research.2024; 12: 976. CrossRef - Evaluation of the efficacy of injectable platelet‐rich fibrin versus platelet‐rich plasma in the regeneration of traumatized necrotic immature maxillary anterior teeth: A randomized clinical trial
Maha Mohamed Abo‐Heikal, Jealan M. El‐Shafei, Samia A. Shouman, Nehal N. Roshdy
Dental Traumatology.2024; 40(1): 61. CrossRef - Radiographical assessment of post and core placement errors encountered by Saudi dental students at different educational levels
Turki Alshehri, Nourhan M. Aly, Raand Altayyar, Deena Alghamdi, Shahad Alotaibi, Passent Ellakany
F1000Research.2023; 12: 976. CrossRef
- Pre‐Operative Factors on Prognosis of Regenerative Endodontic Procedures: A Systematic Review and Meta‐Analysis
- 3,905 View
- 70 Download
- 6 Web of Science
- 6 Crossref

- Periodontal healing following non-surgical repair of an old perforation with pocket formation and oral communication
- Saeed Asgary, Prashant Verma, Ali Nosrat
- Restor Dent Endod 2018;43(2):e17. Published online April 13, 2018
- DOI: https://doi.org/10.5395/rde.2018.43.e17
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
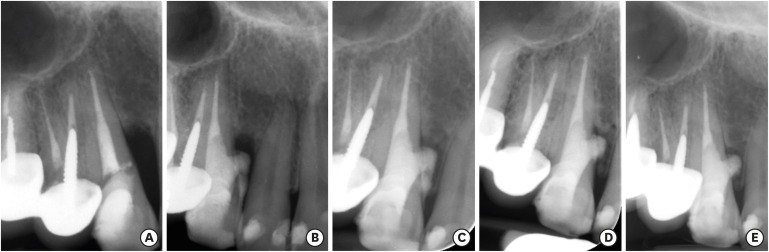
ePub Iatrogenic perforations negatively impact the outcome of endodontic treatments. Studies on prognostic factors showed that perforations in the coronal third of the root with periodontal pocket formation have an unfavorable prognosis. A 36-year-old female was referred for endodontic evaluation of tooth #13 with a history of an iatrogenic perforation, happened 3 years ago. There was a sinus tract associated with perforation, 10 mm probing on the mesial and mesio-palatal, bleeding on probing, radiolucent lesion adjacent to the perforation and complete resorption of the interdental bone between teeth #13 and #12. After the treatment options were discussed, she chose to save the tooth. The tooth was accessed under rubber dam isolation, the perforation site was cleaned and disinfected using 0.5% sodium hypochlorite and sealed with calcium-enriched mixture cement. Eighteen months after treatment the tooth was functional and asymptomatic. The probing depths were normal without bleeding on probing. Radiographically, the interdental crestal bone formed between teeth #13 and #12. Despite all negative prognostic factors in this case (
i.e. , perforations in the coronal third, pocket formation, and radiolucent lesion), healing was unexpectedly achieved via non-surgical repair of the perforation. Further research on biological aspects of healing in the periodontium following iatrogenic perforations are recommended.-
Citations
Citations to this article as recorded by- Managing Internal Inflammatory Root Resorption and Perforation of a Mandibular Primary Molar: A Case Report With 15 Months Follow‐Up
Mana Mowji, Motahareh Khosrojerdi
Clinical Case Reports.2025;[Epub] CrossRef - Nonsurgical Management of Furcation Defects Using Cervical Sealing With Calcium–Silicate Cements: A Clinical Case Series
Saeed Asgary, Shamimul Hasan
Case Reports in Medicine.2025;[Epub] CrossRef - Nonsurgical Management of Simultaneous Double Lateral Root Perforations in Adjacent Teeth Using CBCT and MTA: A Case Report
Beyhan Başkan, Hatice Kübra Başkan, Beyza Güler, Ricardo Faria Ribeiro
Case Reports in Dentistry.2025;[Epub] CrossRef - Comprehensive review of composition, properties, clinical applications, and future perspectives of calcium-enriched mixture (CEM) cement: a systematic analysis
Saeed Asgary, Mahtab Aram, Mahta Fazlyab
BioMedical Engineering OnLine.2024;[Epub] CrossRef - External Cervical Resorption: A Volumetric Analysis on Evolution of Defects over Time
Ali Nosrat, Omid Dianat, Prashant Verma, Martin D. Levin, Jeffery B. Price, Anita Aminoshariae, Fabio Antonio Piola Rizzante
Journal of Endodontics.2023; 49(1): 36. CrossRef - Comparative evaluation of mineral trioxide aggregate, endoseal, and biodentine in furcation perforation repair
Udita Khare Baralay, Srinidhi Surya Raghavendra
Endodontology.2022; 34(1): 22. CrossRef - Calcium Silicate Cements Application in Lateral Root Perforation Repair: A Case Report with 16-Month Follow-Up
Juan G. Robledo, Pablo A. Rodríguez
Open Journal of Stomatology.2021; 11(08): 317. CrossRef - Vital Pulp Therapy as a Conservative Approach for Management of Invasive Cervical Root Resorption: A Case Series
Saeed Asgary, Mahdieh Nourzadeh, Prashant Verma, M. Lamar Hicks, Ali Nosrat
Journal of Endodontics.2019; 45(9): 1161. CrossRef
- Managing Internal Inflammatory Root Resorption and Perforation of a Mandibular Primary Molar: A Case Report With 15 Months Follow‐Up
- 2,616 View
- 13 Download
- 8 Crossref

- Prognostic factors influencing clinical outcome of nonsurgical endodontic treatment
- Seonah Kim
- J Korean Acad Conserv Dent 2010;35(6):436-444. Published online November 30, 2010
- DOI: https://doi.org/10.5395/JKACD.2010.35.6.436
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives This study aimed to assess prospectively the clinical outcome of nonsurgical endodontic treatment and identify patient- and tooth-related factors, rather than treatment-related factors, that were the best predictors of this outcome.
Materials and Methods The inception cohort comprised 441 teeth (320 patients) and 175 teeth (123 patients) were followed up for 1-2 years. Age, gender, presence of medical disease, number of canals, previous endodontic treatment, presence of sensitivity and pain, pulp vitality, swelling or sinus tract of pulpal origin on the gingiva, periapical radiolucency and tendency of unilateral bite on the affected tooth were recorded at treatment start.
Results The outcome was classified on the basis of periapical radiolucency as healed or non healed. The overall healed rate in these cases, including nonsurgical retreatment, was 81.1%. Four tooth-related factors had a negative impact in the bivariate analysis: previous endodontic treatment, necrotic pulp, preoperative gingival swelling or sinus tract of pulpal origin, and preoperative periapical radiolucency. Stepwise logistic regression analysis including patient-, tooth-related factors and level of the root canal filling as a treatment-related factor showed that preoperative gingival lesion (odds ratio [OR]: 4.4;
p = 0.005), preoperative periapical radiolucency (OR: 3.6;p = 0.011), and ≤ 1-2 mm under root filling length (OR: 9.6;p = 0.012) were significant predictors of failure.Conclusions A preoperative gingival lesion of pulpal origin can influence the outcome of nonsurgical endodontic treatment in addition to preoperative periapical radiolucency.
-
Citations
Citations to this article as recorded by- A retrospective study on the prognostic factors and success, survival, and failure outcomes of treated endodontic‐periodontal lesions
Ingar Wong, An Ton, Amiel J. Cassidy, Nicolette Fozzard, Lavanya Ajay Sharma, Robert M. Love, Ajay Sharma
Clinical and Experimental Dental Research.2024;[Epub] CrossRef - Evaluation of gutta-percha removal from the dentinal tubules using different instrumentation techniques with or without solvent: An In vitro study
MukeshKumar Hasija, Babita Meena, Deepti Wadhwa, KulvinderKaur Wadhwani, Virender Yadav
Journal of the International Clinical Dental Research Organization.2020; 12(1): 27. CrossRef - Surgical endodontic management of infected lateral canals of maxillary incisors
Ji-Hyun Jang, Jung-Min Lee, Jin-Kyu Yi, Sung-Baik Choi, Sang-Hyuk Park
Restorative Dentistry & Endodontics.2015; 40(1): 79. CrossRef - Single visit nonsurgical endodontic therapy for periapical cysts: A clinical study
Ipsita Maity, N. Meena, R. Anitha Kumari
Contemporary Clinical Dentistry.2014; 5(2): 195. CrossRef
- A retrospective study on the prognostic factors and success, survival, and failure outcomes of treated endodontic‐periodontal lesions
- 4,125 View
- 34 Download
- 4 Crossref


 KACD
KACD

 First
First Prev
Prev


