Search
- Page Path
- HOME > Search
- Periodontal healing following non-surgical repair of an old perforation with pocket formation and oral communication
- Saeed Asgary, Prashant Verma, Ali Nosrat
- Restor Dent Endod 2018;43(2):e17. Published online April 13, 2018
- DOI: https://doi.org/10.5395/rde.2018.43.e17
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
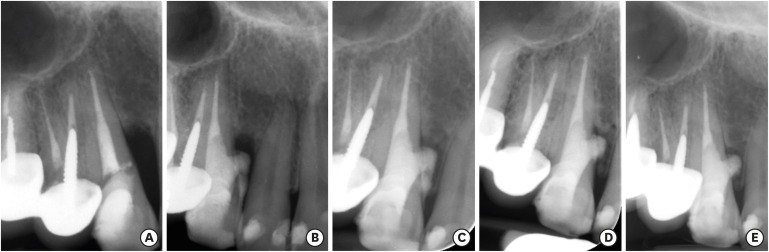
ePub Iatrogenic perforations negatively impact the outcome of endodontic treatments. Studies on prognostic factors showed that perforations in the coronal third of the root with periodontal pocket formation have an unfavorable prognosis. A 36-year-old female was referred for endodontic evaluation of tooth #13 with a history of an iatrogenic perforation, happened 3 years ago. There was a sinus tract associated with perforation, 10 mm probing on the mesial and mesio-palatal, bleeding on probing, radiolucent lesion adjacent to the perforation and complete resorption of the interdental bone between teeth #13 and #12. After the treatment options were discussed, she chose to save the tooth. The tooth was accessed under rubber dam isolation, the perforation site was cleaned and disinfected using 0.5% sodium hypochlorite and sealed with calcium-enriched mixture cement. Eighteen months after treatment the tooth was functional and asymptomatic. The probing depths were normal without bleeding on probing. Radiographically, the interdental crestal bone formed between teeth #13 and #12. Despite all negative prognostic factors in this case (
i.e. , perforations in the coronal third, pocket formation, and radiolucent lesion), healing was unexpectedly achieved via non-surgical repair of the perforation. Further research on biological aspects of healing in the periodontium following iatrogenic perforations are recommended.-
Citations
Citations to this article as recorded by- Managing Internal Inflammatory Root Resorption and Perforation of a Mandibular Primary Molar: A Case Report With 15 Months Follow‐Up
Mana Mowji, Motahareh Khosrojerdi
Clinical Case Reports.2025;[Epub] CrossRef - Nonsurgical Management of Furcation Defects Using Cervical Sealing With Calcium–Silicate Cements: A Clinical Case Series
Saeed Asgary, Shamimul Hasan
Case Reports in Medicine.2025;[Epub] CrossRef - Nonsurgical Management of Simultaneous Double Lateral Root Perforations in Adjacent Teeth Using CBCT and MTA: A Case Report
Beyhan Başkan, Hatice Kübra Başkan, Beyza Güler, Ricardo Faria Ribeiro
Case Reports in Dentistry.2025;[Epub] CrossRef - Comprehensive review of composition, properties, clinical applications, and future perspectives of calcium-enriched mixture (CEM) cement: a systematic analysis
Saeed Asgary, Mahtab Aram, Mahta Fazlyab
BioMedical Engineering OnLine.2024;[Epub] CrossRef - External Cervical Resorption: A Volumetric Analysis on Evolution of Defects over Time
Ali Nosrat, Omid Dianat, Prashant Verma, Martin D. Levin, Jeffery B. Price, Anita Aminoshariae, Fabio Antonio Piola Rizzante
Journal of Endodontics.2023; 49(1): 36. CrossRef - Comparative evaluation of mineral trioxide aggregate, endoseal, and biodentine in furcation perforation repair
Udita Khare Baralay, Srinidhi Surya Raghavendra
Endodontology.2022; 34(1): 22. CrossRef - Calcium Silicate Cements Application in Lateral Root Perforation Repair: A Case Report with 16-Month Follow-Up
Juan G. Robledo, Pablo A. Rodríguez
Open Journal of Stomatology.2021; 11(08): 317. CrossRef - Vital Pulp Therapy as a Conservative Approach for Management of Invasive Cervical Root Resorption: A Case Series
Saeed Asgary, Mahdieh Nourzadeh, Prashant Verma, M. Lamar Hicks, Ali Nosrat
Journal of Endodontics.2019; 45(9): 1161. CrossRef
- Managing Internal Inflammatory Root Resorption and Perforation of a Mandibular Primary Molar: A Case Report With 15 Months Follow‐Up
- 2,617 View
- 13 Download
- 8 Crossref

- Healing outcomes of root canal treatment for C-shaped mandibular second molars: a retrospective analysis
- Hye-Ra Ahn, Young-Mi Moon, Sung-Ok Hong, Min-Seock Seo
- Restor Dent Endod 2016;41(4):262-270. Published online August 29, 2016
- DOI: https://doi.org/10.5395/rde.2016.41.4.262
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Objectives This study aimed to evaluate the healing rate of non-surgical endodontic treatment between C-shaped and non-C-shaped mandibular second molars.
Materials and Methods Clinical records and radiological images of patients who had undergone endodontic treatment on mandibular second molars between 2007 and 2014 were screened. The periapical index scoring system was applied to compare healing outcomes. Information about preoperative and postoperative factors as well as the demographic data of the patients was acquired and evaluated using chi-square and multinomial logistic regression tests.
Results The total healing rate was 68.4%. Healing rates for the mandibular second molar were 70.9% in C-shaped canals (
n = 79) and 66.6% in non-C-shaped ones (n = 117). The difference was not statistically significant.Conclusions The presence of a C-shaped canal in the mandibular second molar did not have a significantly negative effect on healing after treatment. Instead, proper pulpal diagnosis and final restoration were indicated as having significantly greater influence on the healing outcomes of C-shaped and non-C-shaped canals, respectively.
-
Citations
Citations to this article as recorded by- Predicting early endodontic treatment failure following primary root canal treatment
Young-Eun Jang, Yemi Kim, Sin-Young Kim, Bom Sahn Kim
BMC Oral Health.2024;[Epub] CrossRef - Factors Influencing Non-Surgical Root Canal Treatment Outcomes in Mandibular Second Molars: A Retrospective Cone-Beam Computed Tomography Analysis
Da-Min Park, Woo-Hyun Seok, Ji-Young Yoon
Journal of Clinical Medicine.2024; 13(10): 2931. CrossRef - Retrospective Assessment of Healing Outcome of Endodontic Treatment for Mandibular Molars with C-shaped Root Canal
Kishore Kumar Majety, Basanta Kumar Choudhury, Anika Bansal, Achla Sethi, Jaina Panjabi
The Journal of Contemporary Dental Practice.2017; 18(7): 591. CrossRef
- Predicting early endodontic treatment failure following primary root canal treatment
- 1,722 View
- 19 Download
- 3 Crossref

- Management of horizontal root fractures by fabrication of canine protected occlusion using composite resin
- Joo-Hee Shin, Ryan Jin-Young Kim
- Restor Dent Endod 2012;37(3):180-184. Published online August 29, 2012
- DOI: https://doi.org/10.5395/rde.2012.37.3.180
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Traumatic injuries of the face often involve root fractures especially in anterior teeth. The prognosis and the treatment of the root fracture depend on the extent of the fracture line, general health and patient compliance. This case report outlines a new conservative trial treatment modality to stabilize the maxillary central incisors with horizontal root fracture on the cervical to middle third by fabricating canine guidance to remove loading on the traumatized maxillary central incisors during eccentric movements and thus inducing spontaneous healing of the fractured line between the fragments. Radiographs after thirty months showed adequate healing with no signs of pathological changes including root resorption, ankylosis or displacement. Long term follow-up revealed that vitality, stability and aesthetics were maintained and the patient was satisfied with the outcome.
-
Citations
Citations to this article as recorded by- Healing after horizontal root fractures: 3 cases with 2-year follow-up
Yoorina Choi, Sung-Ok Hong, Seok-Ryun Lee, Kyung-San Min, Su-Jung Park
Restorative Dentistry & Endodontics.2014; 39(2): 126. CrossRef
- Healing after horizontal root fractures: 3 cases with 2-year follow-up
- 1,269 View
- 4 Download
- 1 Crossref

- Histology of dental pulp healing after tooth replantation in rats
- Eun-Jin Go, Han-Seong Jung, Eui-Seong Kim, Il-Young Jung, Seung-Jong Lee
- J Korean Acad Conserv Dent 2010;35(4):273-284. Published online July 31, 2010
- DOI: https://doi.org/10.5395/JKACD.2010.35.4.273
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub The objective of this study was to observe the histology of dental pulp healing after tooth replantation in rats. The maxillary right first molars of 4-week-old rat were extracted, and then the teeth were repositioned in the original socket. At 3 days after replantation, there was localized inflammatory reaction. But, pulp revasculization and healing had already begun in the root area. At 5 days after replantation, odontoblast-like cells were observed. Tertiary dentin deposition was observed beneath the pulp-dentin border from 1 week after replantation. And tertiary dentin was increased at 2 weeks after replantation. The presence of odontoblast-like cells and the formation of tertiary dentin were continued to 4 weeks after replantation. At 4 weeks after replantation, the deposition of bone-like tissues and cementum-like tissues was observed. This results show that there is a possibility of pulp healing after tooth replantation in rats and the mineralization of tooth can progress. The mineralization of tooth after replantation was initially occurred by the deposition of tertiary dentin, but as time passed, the deposition of bone-like tissues and cementum-like tissues was begun and increased.
-
Citations
Citations to this article as recorded by- Doxycycline-Loaded Nitric Oxide-Releasing Nanomatrix Gel in Replanted Rat Molar on Pulp Regeneration
Kwan-Hee Yun, Mi-Ja Ko, Yong-Kown Chae, Koeun Lee, Ok-Hyung Nam, Hyo-Seol Lee, Kyounga Cheon, Sung-Chul Choi
Applied Sciences.2021; 11(13): 6041. CrossRef - Bio-Photonic Detection and Quantitative Evaluation Method for the Progression of Dental Caries Using Optical Frequency-Domain Imaging Method
Ruchire Wijesinghe, Nam Cho, Kibeom Park, Mansik Jeon, Jeehyun Kim
Sensors.2016; 16(12): 2076. CrossRef
- Doxycycline-Loaded Nitric Oxide-Releasing Nanomatrix Gel in Replanted Rat Molar on Pulp Regeneration
- 1,962 View
- 22 Download
- 2 Crossref


 KACD
KACD

 First
First Prev
Prev


