Push-out bond strength and marginal adaptation of apical plugs with bioactive endodontic cements in simulated immature teeth
Article information
Abstract
Objectives
This study evaluates the bond strength and marginal adaptation of mineral trioxide aggregate (MTA) Repair HP and Biodentine used as apical plugs; MTA was used as reference material for comparison.
Materials and Methods
A total of 30 single-rooted teeth with standardized, artificially created open apices were randomly divided into 3 groups (n = 10 per group), according to the material used to form 6-mm-thick apical plugs: group 1 (MTA Repair HP); group 2 (Biodentine); and group 3 (white MTA). Subsequently, the specimens were transversely sectioned to obtain 2 (cervical and apical) 2.5-mm-thick slices per root. Epoxy resin replicas were observed under a scanning electron microscope to measure the gap size at the material/dentin interface (the largest and smaller gaps were recorded for each replica). The bond strength of the investigated materials to dentin was determined using the push-out test. The variable bond strengths and gap sizes were evaluated independently at the apical and cervical root dentin slices. Data were analyzed using descriptive and analytic statistics.
Results
The comparison between the groups regarding the variables' bond strengths and gap sizes showed no statistical difference (p > 0.05) except for a single difference in the smallest gap at the cervical root dentin slice, which was higher in group 3 than in group 1 (p < 0.05).
Conclusions
The bond strength and marginal adaptation to root canal walls of MTA HP and Biodentine cement were comparable to white MTA.
INTRODUCTION
White mineral trioxide aggregate (MTA) is considered the gold standard for the single-visit apexification technique [12]. However, this material presents certain shortcomings including a long set-up time and handling difficulties [3]. Recently, a new type of MTA known as MTA Repair HP (Angelus, Londrina, Brazil) has been proposed. This cement comprises a vehicle containing both water and an organic plasticizer, resulting in greater plasticity, higher flow, and improved handling characteristics in comparison to white MTA (Angelus, Londrina, Brazil) [4]. In addition, the substitution of tungstate for bismuth oxide used as the radiopacifier has been shown to reduce the incidence of coronal color change [56].
Another commercially available bioactive material is Biodentine (Septodont, Saint-Maur-des-Fossés, France), which also offers color stability and is easier to apply in several clinical procedures including the management of immature necrotic teeth [78].
During apexification procedures, the apical plug must be able to remain bonded to the root canal walls without displacement while maintaining the dentin/material interfacial integrity either by frictional retention or adhesion [910].
Limited information is available concerning MTA HP and Biodentine cement performance in terms of adhesion and adaptation to root dentin in teeth with open apices. Considering the desirable properties of these materials, evaluations of the strength of the interfacial dentin when using the apical plug technique are pertinent [8]. In this context, the present study evaluated the bond strength and marginal adaptation of MTA HP and Biodentine cements when used as apical plugs in an ex vivo apexification model; MTA was used as reference material for comparison. The following hypothesis was tested: No differences between the 3 types of cement regarding the pertinent properties will be observed.
MATERIALS AND METHODS
Sample selection
The sample size for the primary outcome (push-out bond strength) was estimated from a given effect size f value of 0.72 calculated by a similar previous study, using a level of significance of 5% and a power of 90%, into a one-way analysis of variance (ANOVA) (G*Power 3.1.9.7 for Macintosh; Heinrich Heine, Universität Düsseldorf, Dusseldorf, Germany) [11]. The estimated total sample size was 30 for the 3 study groups (10 samples for each group). A total of 30 extracted single-rooted permanent human teeth were selected after the study was approved by the scientific review committee (protocol #2.660.333) of the local university.
Any extraneous tissue and calculus were removed using curettes; teeth with straight roots and similar lengths were selected. The specimens were analyzed under 13× magnification (M-900, Df Vasconcelos, São Paulo, Brazil). Teeth presenting caries, cracks/fractures, internal/external resorption, or root filled were excluded. Mesiodistal and buccolingual radiographs were used to ensure the complete root formation of the selected teeth. Prior to sectioning, the specimens were stored in sterile saline (0.9%) for 7 days at room temperature in a 100% moist environment.
Open apex model
To simulate an immature tooth, an open apex model was created by sectioning the dental crowns to the cemento-enamel junction using a low-speed diamond saw (S.S. White Artigos Dentários, Rio de Janeiro, Brazil) [1213]. The roots were also sectioned in the apical portion to standardize root length at 13 mm. Subsequently, 3 mm of the apical third were removed to eliminate apical deltas and to standardize the canal exit at the center of the root, thereby maintaining a root length of 10 mm. The open apices were artificially created using Gates Glidden drills #6-1 (Dentsply Sirona, Baden, Switzerland) in a crown-down manner until the #1 bur passed through the apical foramen. Apical preparation divergence was conducted through retrograde instrumentation with a #40 taper 0.6 mm Reciproc instrument (VDW, Munich, Germany) inserted up to the length of the cutting blade and reaching a 1.36-mm-diameter in the foramen.
The canals were irrigated using conventional needle irrigation 23-G (2 mL after every instrument) coupled with a 3-mL syringe with a 5.25% sodium hypochlorite solution (VDW). After removing the smear layer with 5 mL of a 17% EDTA solution (Biodinâmica Química e Farmacêutica, Ibiporã, PR, Brazil) for 5 minutes, a final rinse consisting of 10-mL distilled water was used; the canals were then dried with #80 absorbing paper points (Tanari-Tanariman Indústrial, Manacapuru, AM, Brazil).
Apical plugs
The samples were randomly divided into 3 groups according to the material used as an apical plug (n = 10 per group): group 1 – MTA Repair HP (Angelus); group 2 – Biodentine (Septodont); group 3 – white MTA (Angelus) (Table 1). The materials were manipulated according to the manufacturers’ recommendations, and their insertion into the root canal was aided by an MTA carrier (Angelus) using the microscopic view (M-900; Df Vasconcelos) at 13× magnification. Material condensation was performed with hand pluggers (Odous de Deus, Belo Horizonte, MG, Brazil) under ultrasound vibration by means of an ultrasonic device (ENAC; Osada, Los Angeles, CA, USA) for 5 seconds to form 6-mm-thick apical plugs. The thickness and quality of the apical plugs, as well as the coronal space, were verified using Schilder hand pluggers with cursors and through mesiodistal and buccolingual radiographs. A moistened foam was used to simulate periapical tissue characteristics and offer slight resistance to material extrusion [13]. The roots were stored at 37°C in a 100% moist environment for 7 days prior to cutting procedures.
Root sectioning
The specimens were fixed to acrylic plates with wax (Asfer Indústria Química, São Caetano do Sul, SP, Brazil) so that the long axis of the root remained parallel to the plate surface. Next, the plates were coupled to a precision cutting machine (Buehler, Lake Bluff, IL, USA) fitted with a high-precision diamond disc (Buehler). The apical part of each specimen was then cut perpendicularly to the long axis at 350 rpm under continuous water cooling, producing 2 (cervical and apical) 2.5-mm-thick slices. The thickness of each slice was verified using a digital caliper (precision level +/− 0.001 mm).
Resin replica preparation
The apical surface of each root slice was uniformly polished with 600-, 1200-, and 2000-grit SiC papers (3M ESPE, São Paulo, Brazil) for 10 seconds each. The surface needed to be polished in order to flatten the surface and eliminate roughness caused by the diamond saw as a rough surface would make it difficult to interpret images during SEM analysis. In addition, polishing to flatten the surface makes GAPS measurement more reliable as the assessment points are at the same height. After polishing, the specimens were washed with distilled water and dried with air blasts. Impressions of the root slice surfaces were obtained using a polyvinylsiloxane material (Aquasil ULV; Dentsply De Tray, Konstanz, Germany) delivered through microtip syringes. After 5 minutes, the impressions were removed from the root slices, and replicas were obtained with a low-viscosity epoxy resin (Polipox Indústria e Comércio, São Paulo, Brazil).
Scanning electron microscope (SEM) analyses
Resin replicas were fixated in aluminum stubs and sputter-coated with gold for SEM analysis of gaps between the apical plug and the dentin walls. The replicas were photographed at 60× and 700× magnifications, and interfacial gap measurements (μm) were performed by one calibrated and blinded examiner with the aid of the SEM Control User Interface software (Version 2.01, 2008, 2009; JEOL Technics, Tokyo, Japan). The largest and smaller gaps were recorded for each replica [14].
Push-out test
After 2 weeks of cement placements, the push-out test was performed on the original root slices individually positioned on a stainless steel base (2.5-mm orifice diameter) fixed to the testing machine (Instron Model 3344; Instron, Norwood, MA, USA). Slice positioning was performed in the same direction as the metal base orifice with the cervical face turned down.
A metal rod with an active 1-mm-diameter tip fixed in the superior portion of the testing machine was positioned over the apical plug, and the push-out test was conducted at 0.5 mm/min until the material was dislodged.
The newtons of force was divided by the internal area of the radicular dentin. The surface area was obtained using the following formula: A = π(R2+R1) [h2 + (R2-R1)2]0.5, where π = 3.14, R2 = coronal radius of the plug (larger radius), R1 = apical radius of the plug (smaller radius), and h = slice width.
Statistical analyses
The D'Agostino-Pearson test was applied to verify data distribution. An overall normal distribution was noted for the variable bond strength, while no normal distribution was verified for the variable gap size.
The 1-way ANOVA and Tukey's post-hoc test were used to assess differences in the variable bond strength between the 3 groups. This analysis was performed independently for the apical and cervical root dentin slices and for the mean values of both slices.
The Kruskal-Wallis test and Dunn's post-hoc test were conducted to assess differences in the variable gap size between the 3 groups. This analysis was performed independently for the apical section and for the cervical section as well as for the largest and the smallest gap.
All analyses were performed using GraphPad Prism software (Version 6.05; GraphPad Software, San Diego, CA, USA) at a significance level of 5%.
RESULTS
The push-out test results did not reveal significant differences in the bond strength variable between the 3 assessed groups, including apical and cervical root dentin slices as well as the mean values of both slices (p > 0.05; Table 2). No significant differences in the gap-size variable were noted in the SEM photomicrographic analyses of positive replicas between the 3 evaluated groups, either for apical or for cervical root dentin slices, independently evaluating both the largest and the smallest gap (p > 0.05; Table 3; Figure 1). A single exception was the difference in regard to the smallest gap at the cervical root dentin slice, which was higher in group 3 than in group 1 (p < 0.05; Table 3; Figure 1).
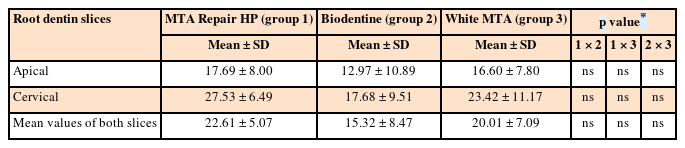
Means and standard deviations of the bond strength values and comparisons among the investigated groups
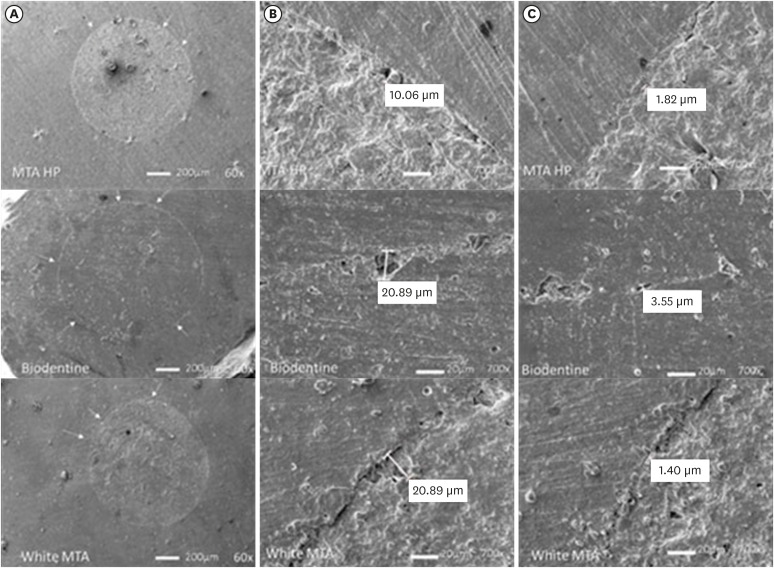
Scanning electron microscope resin replica photomicrographies of HP MTA, Biodentine and white MTA cements. Plug circumference (A); Largest gap (B); Smallest gap (C). Arrows indicate small defects seen at 60× magnification. The largest and smallest gaps are shown at 700×.
MTA, mineral trioxide aggregate.
DISCUSSION
The use of bioactive calcium silicate cement continues to spread and has gained increasing attention in the dental literature, especially in the field of endodontics. The satisfactory characteristics of this cement make it an excellent candidate for several clinical procedures including apexification [215].
Bond strength and marginal adaptation are crucial and desirable properties for all materials used for endodontic purposes, and failure to ensure these characteristics is one of the main causes of root canal treatment failure [1617]. In the present study, the results for MTA HP, Biodentine, and white MTA cements revealed similar bond strength and marginal adaptation.
As in other studies, bond strength was assessed in vitro using the push-out test, a widely accepted method used to estimate the adherence of a certain material to root dentin simulating clinical stresses [181920]. However, when comparing the 3 types of cement, no significant difference was observed, and the chemical/molecular similarity of the 3 materials may be a possible justification for this result. Few studies, however, have compared the bond strengths of MTA HP, Biodentine, and white MTA, thus limiting direct comparisons of these results with those reported in other investigations [21].
Previous assessments have also reported no significant differences when comparing the bond strength of MTA Angelus, ProRoot MTA, and Biodentine cements used as root-filling material, thereby corroborating the results presented herein [22].
By contrast, Silva et al. [23], in one of the few articles comparing white MTA, MTA HP, and Biodentine cements, observed significantly different performances when evaluating bond-strength values. The authors reported that Biodentine presented higher resistance values than MTA HP and white MTA. MTA and Biodentine particle-size variations and the high plasticity of MTA HP were 2 of the factors cited as justifications for this result [23].
According to Bodanezi et al. [24], restorative procedures with MTA should be postponed for at least 72–96 hours after mixing to allow the material to attain its ideal physical properties. Moreover, Bachoo et al. [25] reported that the initial reaction of Biodentine takes approximately 12 minutes, but the delivery of complete maturation takes 2 weeks to 1 month. Such factors could justify the non-significant but lower values of bond strength when compared to MTA.
The other property evaluated was marginal adaptation quality. The presence of marginal gaps between the cement and the root dentin can potentially be responsible for apical infiltration, allowing bacteria and their by-products to permeate the periapical tissue and generating several pathologies [26]. Thus, this property becomes critically important in the selection of material to be used in apexification procedures [27].
There are a variety of different approaches to testing marginal adaptation quality, including microleakage methods such as the dye penetration method, electrical method, the fluid filtration technique, radioisotope tracing, and marginal adaptation by SEM [28]. In accordance with several studies, SEM was applied to assess the quality of marginal cement adaptation due to its ability to provide high magnification and suitable resolution [2930]. In this study, a SEM was utilized for marginal gap assessment. In SEM, the defects at the submicron level can be observed at required magnification, and final evaluations can be performed by preserving microphotographs.
In spite of the precautions taken, the process of preparing biological samples for analysis may be associated with the introduction of artifacts, consequently resulting in alterations. Evaporation under high vacuum and dehydration for sample spray coating culminate in expansion and/or contraction processes, which can, in turn, cause cracking in hard tissues and lead to the filling material shifting from the surrounding dental structure [31]. In the present study, the replication technique was used in order to mitigate these adverse situations and corroborate with other studies that have reported the successful use of this method [3233]. According to Teaford et al. [34] and Gondim et al. [35], the replicas accurately maintain the details of the copied structure. Thus, its use allows for the preservation of the original specimens and enables their use in other tests and analyses [36].
Regarding marginal adaptation, no significant differences between the materials were observed in the present study. In addition, as noted for the property of strength of the joint, the number of articles that investigated the marginal adaptation between white MTA, MTA HP, and Biodentine is also minimal.
In line with the findings of this study, previous assessments have also detected similarities in the marginal adaptation of MTA and Biodentine when compared to two other calcium-silicate-based cements [37]. The authors attribute this to calcium silicate being the main constituent of these materials, as well as methodological similarities in sample preparation and material handling and insertion, which create similar consistencies and flow [3738]. Findings from other studies also reveal the absence of significant differences between gap percentages and diameter in the interface when comparing MTA and Biodentine cement [113940].
It is relevant to note that the present study has limitations resulting from an in vitro investigation. In addition, the sample comprised simulated immature teeth since the selection of human teeth in this condition, which would be ideal, is impractical. In addition, it is important to consider the limitations of the methodology used in relation to the gap assessment resource. If we consider sealing ability as the seal reproduction in the whole canal perimeter, a gap may not represent what has actually occurred in the entire apical plug. Therefore, it is extremely difficult to establish a correlation between sealing ability and marginal adaptation.
Considering the similar and excellent results for MTA application in recent years, it seems appropriate to emphasize the importance of the findings observed herein. Thus, the improvement in the clinical applicability of MTA Repair HP qualifies it as a highly suitable material, especially compared to white MTA. At the same time, the results obtained for the Biodentine cement also seem favorable since this material was developed to replace dentin, and its applicability has been proven in several therapies. Future studies are needed to corroborate the results of this study and to investigate the behavior of these materials when exposed to in vivo conditions.
CONCLUSIONS
Based on the results reported herein, it can be concluded that the bond strength and marginal adaptation quality of calcium silicate cement-based on MTA Repair HP, Biodentine, and white MTA are comparable when used as apical plugs.
ACKNOWLEDGEMENTS
School of Dentistry - Federal University of Minas Gerais - UFMG for using the testing machine (Instron Model 3344; Instron, Norwood, MA, USA) and carrying out the push-out test.
Notes
Funding: This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior Brasil (CAPES) - Finance Code 001. MCRH is a research fellow of Fundação de Amparo à Pesquisa do Estado de Minas Gerais (FAPEMIG CDS-PPM-00653-16).
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
Author Contributions:
Conceptualization: Sá MAB, Nunes E, Brito Jr M, Silveira FF.
Data curation: Sá MAB, Nunes E, Brito Jr M, Amaral RR, Silveira FF, Horta MCR, Antunes ANG, Cohen S.
formal analysis: Sá MAB, Horta MCR, Silveira FF.
Funding acquisition: Sá MAB, Brito Jr M, Silveira FF.
Investigation: Sá MAB, Silveira FF.
Methodology: Sá MAB, Brito Jr M, Silveira FF, Antunes ANG.
Project administration: Sá MAB, Brito Jr M, Silveira FF.
resources: Sá MAB, Silveira FF.
Software: Silveira FF, Horta MCR.
Supervision: Sá MAB, Nunes E, Brito Jr M, Amaral RR, Silveira FF, Horta MCR, Antunes ANG, Cohen S.
Validation: Sá MAB, Nunes E, Brito Jr M, Amaral RR, Silveira FF, Horta MCR, Antunes ANG, Cohen S.
Visualization: Sá MAB, Nunes E, Brito Jr M, Amaral RR, Silveira FF, Horta MCR, Antunes ANG, Cohen S.
Writing original draft: Sá MAB, Silveira FF.
Writing review and editing: Sá MAB, Nunes E, Brito Jr M, Amaral RR, Silveira FF, Horta MCR, Antunes ANG, Cohen S.





