Silver nanoparticles in endodontics: recent developments and applications
Article information
Abstract
The elimination of endodontic biofilms and the maintenance of a leak-proof canal filling are key aspects of successful root canal treatment. Several materials have been introduced to treat endodontic disease, although treatment success is limited by the features of the biomaterials used. Silver nanoparticles (AgNPs) have been increasingly considered in dental applications, especially endodontics, due to their high antimicrobial activity. For the present study, an electronic search was conducted using MEDLINE (PubMed), the Cochrane Central Register of Controlled Trials (CENTRAL), Google Scholar, and EMBASE. This review provides insights into the unique characteristics of AgNPs, including their chemical, physical, and antimicrobial properties; limitations; and potential uses. Various studies involving different application methods of AgNPs were carefully examined. Based on previous clinical studies, the synthesis, means of obtaining, usage conditions, and potential cytotoxicity of AgNPs were evaluated. The findings indicate that AgNPs are effective antimicrobial agents for the elimination of endodontic biofilms.
INTRODUCTION
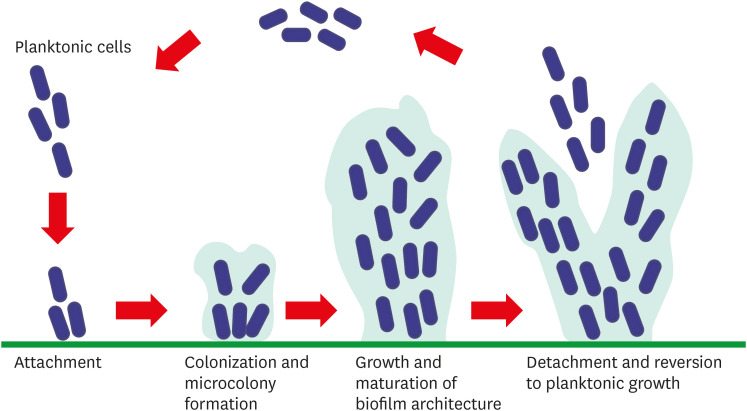
A main cause of failure and secondary infection in root canal treatment (RCT) is the presence of biofilms [1], which are organized polymeric structures formed by microorganisms. The extracellular matrix of a biofilm is secreted by bacteria and is composed of metabolic-output polymers that adhere strongly to surfaces [23]. Biofilms develop in stages: initial adherence of microbes to a surface or bacterial cell, generation of microcolonies, maturation, and finally, the expansion of the biofilm [45]. The main purpose of endodontic treatment is to eliminate the complex, resistant polymeric biofilm structure. Therefore, in RCT, chemical irrigation agents and medicaments are used in addition to mechanical preparation. During the irrigation process, sodium hypochlorite (NaOCl), EDTA, and chlorhexidine (CHX) solutions are applied at different concentrations to eradicate the smear layer [6]. A number of hydrogel-based pharmaceuticals have also been produced for placement in the root canal between treatments. However, no approach to treating stubborn infections has been entirely successful. Clinical research has shown variable success rates for non-surgical endodontic therapies, ranging from 73.5% to 92.3% [7].
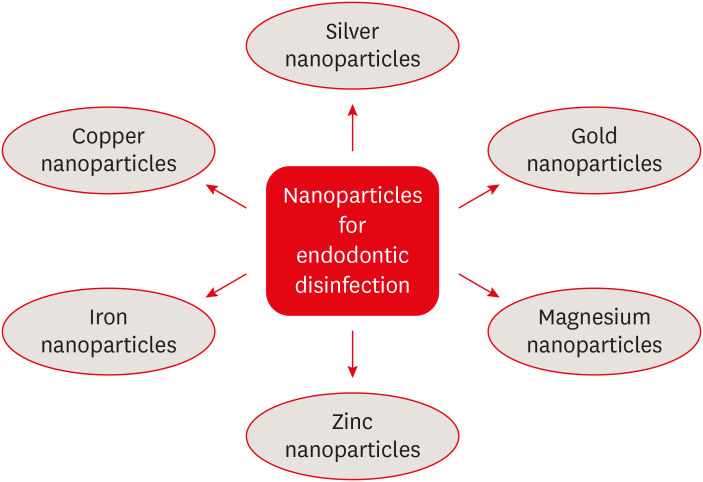
Nanotechnology, which emerged in the 21st century, led to a paradigm shift in dentistry (Figure 1). Nanoparticles (1–100 nm) form the foundation of this technology [8]. Many nanomaterials occur naturally or arise via chemical synthesis. Because of their antibacterial properties and high surface-area-to-volume ratio [9], nanoparticles have attracted considerable attention from endodontic researchers and clinicians.
Metallic nanoparticles that disrupt bacterial cell membranes have long been available [10]. To treat persistent infections [11], nanoparticles of silver, gold, copper, or zinc—all of which have unique physical properties and mechanisms underlying their antimicrobial activities—have been used [1213]. Silver nanoparticles (AgNPs) are among the most well-studied due to their wide range of antimicrobial properties against various bacteria, viruses, and fungi [1114]. In endodontics, AgNPs have been tested for use as endodontic retrofill materials, canal sealers, root canal pharmaceuticals, and irrigation solutions [15]. In this study, recent evidence from in vitro and in vivo studies was reviewed regarding the chemical, physical, and antimicrobial properties of AgNPs, as well as their dosage and cytotoxicity.
REVIEW
Biofilm in endodontic diseases
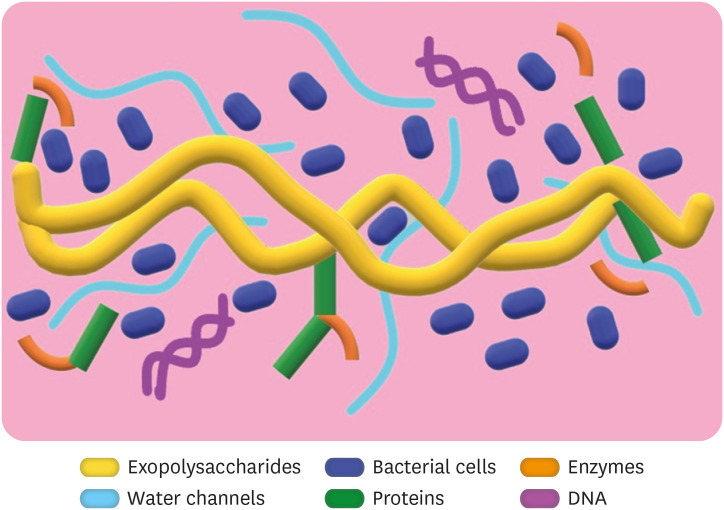
Biofilms are highly organized, surface-adherent structures of microcolonies [16] (Figure 2). The main component of biofilms is an exopolymeric matrix consisting of polysaccharides, proteins, enzymes, and bacterial metabolites [1718]. Exopolysaccharides are synthesized both intracellularly and extracellularly, and have skeletal functions [19] (Figure 3). Moreover, biofilms are in contact with other compounds that play roles in bacterial adhesion and resistance [20]. Another component of biofilms is protein, which facilitates stabilization and binding to dentin. The glucan-binding proteins of Streptococcus mutans, a major cause of dental caries, are well-studied components that are critical to biofilm formation [2122]. The maturing biofilm varies depending on environmental and nutritional factors as well as fluid movement [23]. The bacterial cells in these structures communicate via their own signals or those of other microbial cells [24]. Based on extracellular signal generation and detection, quorum sensing (a cell-to-cell communication process) increases with population density [2526]. Microbial biofilm infections can reappear after long periods of inactivity [27]. Secondary endodontic infections can become acute due to asymptomatic processes. The main known cause of recurrent apical periodontitis after RCT is Enterococcus faecalis [28], a Gram-positive facultative anaerobic bacteria species that is among the most commonly isolated from root canal systems [29]. The removal of these bacteria from the canal is a major obstacle, since they can remain alive under a wide variety of acidic and basic conditions, as well as under conditions of long-term nutritional deprivation [28].
The biofilm of E. faecalis contains extracellular DNA (eDNA), which is released from the cell in various ways, as well as exopolysaccharides, proteins, and lipids [30]. A previous report showed that eDNA is produced during an early stage of E. faecalis biofilm formation [31]. This species also has a peptidoglycan cell wall, which improves bacterial survival [32]. Scanning electron microscopy has shown that E. faecalis adheres to collagen structures, colonizes dentin surfaces, and can progress along dentin tubules of the root canal, resulting in organized biofilms [33].
Chemical irrigation solutions, intracanal preparations, and local antibiotics have been used for years to eliminate biofilms. However, microorganisms may develop resistance to these antimicrobial agents over time. Therefore, research has focused on new antibiofilm strategies [3435].
Antimicrobial nanoparticles
Nanotechnology, or the examination and application of certain objects of extremely small size, can be adapted in different scientific fields, such as chemistry, biology, physics, materials science, and engineering, as well as the health sciences. A nanoparticle is defined as a nano-object, approximately 1 to 100 nm, with 3 external nanoscale dimensions.
Nanoparticles have gained many new applications in dentistry due to their remarkable physical properties, such as small size, large surface area, surface charge, and shape. To eliminate root canal infections, chemical and mechanical instrumentation is performed before filling. The use of nanoparticles in the disinfection process is a new strategy to reduce the treatment failure rate [3637]. Previous studies have reported that particle size is an important factor in the antimicrobial activity of nanoparticles [38]. In addition, the high charge density and large surface areas of nanoparticles allow bacterial cells to interact more with the negatively charged surface [39]. Metallic and organic nanoparticles with different morphologies have been used in dentistry to combat drug-resistant bacteria. In addition, nanoparticles obtained from natural biopolymers such as chitosan or nanoparticle-incorporated biomaterials have been found to exhibit superior antimicrobial properties [3740]. Metallic nanoparticles, such as copper, gold, titanium, cerium, magnesium, iron, and zinc, exhibit antimicrobial activity upon contact with bacterial cells. After attachment to the cell membrane and entrance into the cell, nanoparticles interact with vital cell components such as DNA and RNA and alter the cell membrane permeability, genetic material, ribosomes, and proteins. These effects mainly depend on the capacity of metallic nanoparticles to produce reactive oxygen species (ROS), which can alter the metabolic activity of bacteria [13]. Major ROS that can cause oxidative cellular damage include superoxide, hydrogen peroxide, and hydroxyl radicals. Additionally, after metal ions are released from metal oxides and attach to the cell membrane, they can bind to functional groups of proteins and adversely impact normal cellular functions.
Although these nanoparticles are a potential technology for endodontic disinfection, their long contact time and toxicity can be significant disadvantages [41]. Among the metallic nanoparticles, AgNPs stand out due to their surface properties, particle reactivity in solution, and ion release.
Synthesis of AgNPs
Various physical, chemical, and biological methods have been adopted for the synthesis of AgNPs. A reliable and environmentally friendly methodology for the synthesis of metal nanoparticles is a key goal in nanotechnology [42]. Physical and chemical syntheses tend to be more difficult, expensive, and dangerous than the biosynthesis of AgNPs [4344]. Biological procedures for the synthesis of AgNPs, which involve microorganisms and plants, have enormous advantages over physical and chemical methods due to the use of nontoxic and biocompatible substrates and relatively easier synthesis in environmental terms [45]. In recent years, the development of bio-inspired green synthesis of AgNPs has been a focus in medical science and disease treatment [46]. Biomolecules in plant extracts, which are involved in the reduction of metal ions to nanoparticles, provide a single-stage and environmentally friendly synthesis. In addition to serving as reducing agents in the green synthesis of AgNPs and gold nanoparticles, these biomolecules act as capping or stabilizing agents [47]. Previous studies have suggested that the antimicrobial properties of AgNPs are affected by factors such as shape, size, and concentration. In a study by Hong et al., [48] 3 types of AgNPs were synthesized, and their antimicrobial effects were compared against Escherichia coli. According to the results, nanocubes and nanospheres exhibited stronger antibacterial effects than nanowires. This can be attributed to the fact that nanocups and nanospheres interact faster and more frequently with the cell membrane, as they have larger surface areas and greater reactivity. Most such research has focused on various plant sources for synthesis, diverse characterization techniques for identification, and antimicrobial activity against pathogens [42]. Information about the physical appearance and the characterization of AgNPs can be revealed using ultraviolet-visible spectroscopy, electron microscopy, and energy-dispersing spectroscopy [49].
Mechanisms of action of AgNPs
Many studies have shown that the antimicrobial effects of AgNPs are associated with oxidative dissolution and silver ion release. Silver ions have high affinity for electron-donating groups (such as sulfhydryl, amino, imidazole, phosphate, and carbonyl groups), which are densely located on membranes or proteins [50]. Thus, they can act on diverse components of bacterial cells (Figure 4). These ions can adhere to the cell wall and cytoplasmic membrane via electrostatic attraction, and they can also adhere to sulfur-rich proteins, thereby increasing the permeability of the membrane and damaging these structures [51]. This can also result in the uptake of free silver ions into the cell, disrupting ATP molecules, thus preventing DNA replication or resulting in the formation of ROS via AgNPs [52]. In Gram-negative bacteria, pores in the outer membrane also promote the uptake of AgNPs [53]. In addition, AgNPs modify the effects of phosphotyrosine, impairing communication between organelles [5254]. All of these mechanisms result in oxidative stress in the cell and increased quantities of free oxygen radicals, as well as cell lysis due to protein denaturation [5055]. Another important property of nanoparticles is their large surface area. AgNPs with a larger surface area have greater silver ion density [5657]. Additionally, AgNPs further destabilize bacterial membranes, increase permeability, and cause leakage of cell components [37]. The response of microbial cells to silver ions can differ, so the properties of AgNPs and their relationships with cells should be elucidated to better understand antibiofilm activity [58].
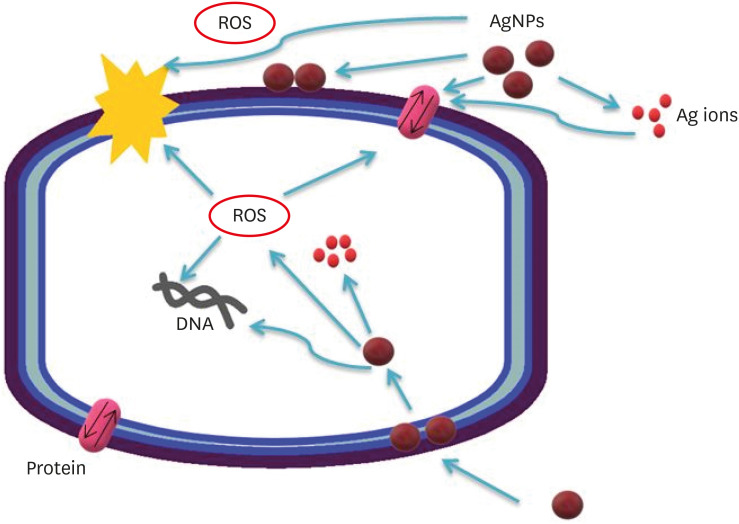
Possible antibacterial mechanisms of AgNPs. AgNPs can: 1) bind to the cell membrane, membrane proteins, and DNA bases, leading to the disruption of normal function; 2) release silver ions, affecting the membrane, DNA, and proteins; and 3) generate ROS, which may also affect DNA, the cell membrane, and membrane proteins.
AgNP, silver nanoparticle; ROS, reactive oxidative species.
AgNP characterization and analysis
Many techniques have been introduced and applied in laboratory research (Table 1), including scanning electron microscopy [3359], transmission electron microscopy [44], scanning electrochemical microscopy [60], atomic force microscopy [61], dynamic light scattering [62], ultraviolet-visible spectroscopy [63], and confocal laser scanning microscopy analysis [64].
Endodontic applications of AgNPs
The success of RCTs depends on the removal of endodontic biofilms from canal walls, the elimination of microorganisms, and leak-proof canal filling. For the endodontic treatment of teeth with complex root canal anatomy, chemomechanical canal preparation should be performed during instrumentation. Nanoparticles have also been used for disinfection in endodontics. Metallic nanoparticles are attractive due to their clinically effective antimicrobial properties. Many studies have involved the use of AgNPs to eliminate biofilm layers, which are the main cause of secondary infections [91534]. Lotfi et al. compared the effectiveness of AgNPs against E. faecalis with that of NaOCl in an irrigation solution; 5.25% NaOCl and low-concentration AgNPs showed similar bactericidal effects [65]. Hiraishi et al. reported that biofilms were completely eliminated 60 minutes after administration of 3.8% sodium diamine fluoride [66]. Another study found that an AgNP solution destroyed fewer bacteria than a CHX solution, but dissolved more biofilm [67]. Wu et al. suggested that antimicrobial efficacy varies by application technique [68]. Treatment with 0.02% AgNP medicament gel was significantly more successful in disrupting biofilm structure than treatment with 0.01% AgNP gel, 0.01% AgNP irrigation solution, and calcium hydroxide. When AgNPs are employed as a medicament, an extended interaction occurs between positively-charged AgNPs and negatively-charged biofilm bacteria. In another in vitro study, researchers investigated the effectiveness of AgNPs against E. faecalis, Klebsiella pneumoniae, and Candida albicans, and they found that the greatest antimicrobial effect was achieved with a combination of 15 µg/mL AgNP and 2% CHX solution [69].
Recently, Yousefshahi et al. applied calcium hydroxide with silver, copper, zinc, or magnesium; the combination of 1% AgNP and calcium hydroxide was more effective against biofilms than calcium hydroxide paste alone, but a mixture of 1% copper and calcium hydroxide paste was the most effective [70]. Additionally, less leakage has been found to occur when using nanosilver-coated gutta-percha points [71]. In another study, calcium-disilicate-based mineral trioxide aggregate (MTA), which has known antibacterial properties, was combined with AgNPs; the AgNP-MTA formulation inhibited the growth of Aggregatibacter actinomycetemcomitans, Fusobacterium nucleatum, Porphyromonas gingivalis, and Prevotella intermedia [72]. Additionally, Baras and Melo et al. combined 5% dimethylaminohexadecyl methacrylate sealer with 0.15% AgNPs and reported a strong antibiofilm effect with no reduction in sealing ability [73].
In summary, nanotechnology has been used in a wide range of endodontic applications (Table 2). Clinicians should be aware of the latest developments and information on how best to use nanoparticles.
Efficacy of AgNPs against E. faecalis
Endodontic treatments aim to annihilate microorganisms and their biofilm architecture and thereby minimize the treatment failure rate. In many studies, AgNPs have been applied through various methods for this purpose. Almedia et al. reported that a solution of 1% AgNPs had effects against E. faecalis similar to those of conventional irrigation solutions [74]. Likewise, Halkai et al. found that biosynthesized AgNPs greatly inhibited E. faecalis [75]. Calcium hydroxide paste has been used as a medication for RCT for many years [76]. However, this material has also been shown to fail to provide adequate disinfection and biofilm elimination. Afkhami et al. used AgNPs as carriers for calcium hydroxide and found that this treatment had the potential to remove E. faecalis from root dentin [78]. In another study, Wu et al. noted that the effectiveness of AgNPs depends on the method of application; 0.02% AgNP medicament gel significantly altered biofilm structures and resulted in fewer post-treatment E. faecalis cells than treatment with 0.01% AgNP gel and calcium hydroxide [68]. In another study, it was found that Ag–Ca–Si mesoporous nanoparticles had an enhanced ability to prevent the growth of E. faecalis on the dentin surface. Findings also included high pH and the continuous release of Ag, Ca2+, and SiO3 2− ions, although this method did not completely eliminate E. faecalis [79]. Laboratory research on this subject is still ongoing.
Potential toxicity of AgNPs
Over the years, numerous in vitro and in vivo experiments have been conducted to investigate the toxic effects of AgNPs on living tissues and organisms [80]. The factors that affect the toxicity of AgNPs include particle shape, size, and surface chemistry; crystallinity; capping agents; ionic strength; pH; and the presence of ligands, divalent cations, and macromolecules [81]. Due to the exposed and complex nature of AgNPs, uncertainty (and to some degree controversy) remains regarding the extent to which each constituent ion, ion-protein complex, and particle contributes to cellular toxicity [82]. In some in vitro studies, it has even been reported that AgNPs cause oxidative stress and disrupt the mitochondrial function of human cells [83]. Paná\\xc4\\x8dek et al. used low concentrations of AgNPs against multiresistant bacteria and noted that low concentrations were not cytotoxic for potential medical applications in mammalian cells [84]. It has also been suggested that the green synthesis of AgNPs does not affect human dermal fibroblasts when administered at a concentration of less than 32 μg/mL [85]. This underscores the importance of the method of synthesis and the concentration density. Importantly, the toxicity is always related to the dose and duration of contact. Direct contact with the oral cavity, teeth, and surrounding tissues is an important consideration due to the potentially harmful effects of AgNP treatment in endodontic applications.
Over the past decades, the application of AgNPs in endodontics has attracted increasing attention. Using the published literature, we reviewed recent findings regarding the unique chemical, physical, and antimicrobial properties of AgNPs, as well as dosage and cytotoxicity. Although several studies have revealed promising clinical treatment results, the potential cytotoxicity of AgNPs should also be taken into consideration, even given the superior antimicrobial properties of these particles in endodontic disinfection.
CONCLUSIONS
Biofilms are an important factor that should be eliminated in the treatment of primary and recurring endodontic infections. Nanoparticles present new opportunities for endodontic disinfection. Based on their superior antimicrobial properties, AgNPs have attracted attention in this field, and many studies have been conducted. Based on these studies, it can be concluded that treatment with AgNPs is an effective method to eliminate endodontic biofilms. In light of this finding, studies on the applications of nanoparticles in endodontics should be continued.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
Author Contributions:
Conceptualization: Celikten B.
Data curation: Amasya G.
Investigation: Oncu A, Amasya G.
Methodology: Oncu A.
Project administration: Celikten B.
Resources: Sevimay FS.
Supervision: Huang Y.
Validation: Orhan K.
Visualization: Sevimay FS.
Writing - original draft: Oncu A, Amasya G.
Writing - review & editing: Huang Y.