The effect of individualization of fiberglass posts using bulk-fill resin-based composites on cementation: an in vitro study
Article information
Abstract
Objectives
This study evaluated the bond strength of various fiberglass post cementation techniques using different resin-based composites.
Materials and Methods
The roots from a total of 100 bovine incisors were randomly assigned to 5 treatment groups: G1, post + Scotchbond Multi-Purpose (SBMP) + RelyX ARC luting agent; G2, relined post (Filtek Z250) + SBMP + RelyX ARC; G3, individualized post (Filtek Z250) + SBMP; G4, individualized post (Filtek Bulk-Fill) + SBMP; G5, individualized post (Filtek Bulk-Fill Flow) + SBMP. The samples were subjected to the push-out (n = 10) and pull-out (n = 10) bond strength tests. Data from the push-out bond strength test were analyzed using 2-way analysis of variance (ANOVA) with the Bonferroni post hoc test, and data from the pull-out bond strength test were analyzed using 1-way ANOVA.
Results
The data for push-out bond strength presented higher values for G2 and G5, mainly in the cervical and middle thirds, and the data from the apical third showed a lower mean push-out bond strength in all groups. No significant difference was noted for pull-out bond strength among all groups. The most frequent failure modes observed were adhesive failure between dentine and resin and mixed failure.
Conclusions
Fiberglass post cementation using restorative and flowable bulk-fill composites with the individualization technique may be a promising alternative to existing methods of post cementation.
INTRODUCTION
The use of intraradicular retainers in endodontically treated teeth, despite great damage to the coronal tooth structure, is necessary to achieve superior longevity of restorative treatment [12]. Clinically, fiberglass posts are commonly used due to aesthetic issues, but they also increase the fracture strength and allow uniform distribution of masticatory forces over the root structure due to their modulus of elasticity, which is similar to that of dentine [34].
Currently, several fiberglass post cementation techniques are scientifically accepted, and these are associated with an auto- or dual-cure luting agent and a self-etch or etch-and-rinse adhesive system. In some challenging clinical situations, it may be necessary to use other techniques, such as in the cases of extensive and large roots, in which it is possible to reline the fiberglass post with a resin-based composite in order to decrease the thickness of the resin cement [3567]. The scientifically recognized techniques that are commonly performed in dental clinics are 1) fiberglass post cementation using traditional methods with a dual-cure luting agent, using a conventional adhesive system and 2) relining with conventional resin-based composites [89]. However, the existence of multiple fiberglass post cementation techniques, as well as the considerable variation in clinical scenarios, requires a specific level of manual ability from the professional; although this factor can be limited or neglected at certain times, it does influence treatment success.
The failure of rehabilitation using fiberglass posts is associated with root characteristics that affect operator visibility and access, as well as with the instrumentation technique and irrigation solution used, endodontic contamination [10], resin composite characteristics (for instance, a high C-factor within the root canal), resin cement thickness [11], the presence of bubbles, and intraradicular retainers [3712].
In this context, an innovative technique for relining the fiberglass post could involve a bulk-fill composite as an alternative material, since its main feature is lower shrinkage stress compared to conventional resin-based composites, as well as increased translucency, which improves light penetration [13]. Therefore, the individualized fiberglass post technique with bulk-fill composites used in this study enables the elimination of extensive cementation protocols. To the best of our knowledge, no previous studies have evaluated the role of bulk-fill composites in fiberglass post cementation; the use of these composites has been described only for relined fiberglass posts [89].
Thus, the aim of this in vitro study was to evaluate the bond strength of different fiberglass post cementation techniques using a conventional resin-based composite, as well as restorative and flowable bulk-fill composites, as a substitute for traditional cementation.
MATERIALS AND METHODS
Specimen preparation
In this study, 100 freshly extracted and intact young bovine incisors were selected, stored in a 0.1% thymol solution, and divided randomly across the mechanical tests (push-out and pull-out bond strength) and treatment groups. All of the roots of the bovine teeth were sectioned using a double-sided diamond disc (KG Sorensen, Barueri, SP, Brazil) at the cemento-enamel junction at a length of 18 mm and a cervical root canal width of 3.5 mm. The roots were endodontically instrumented at a working length of 17 mm with K-files (Dentsply Maillefer, Ballaigues, Switzerland) up to size 40 with 1% NaOCl between each preparation step, and they were filled using gutta-percha and AH 26 Root Canal Sealer (Dentsply Maillefer) as part of the lateral condensation technique [14]. After 24 hours, 12 mm of the endodontic material was removed with #2 Gates-Glidden and #5 and #6 Largo Peeso drills (Dentsply Maillefer), and the cementation protocols proceeded with a fiberglass post #3 (Whitepost DC, FGM, Joinville, SC, Brazil). Product specifications are presented in Table 1.
The 100 bovine incisor roots were divided into 5 groups according to the cementation protocol (Table 2): G1, post + Scotchbond Multi-Purpose (SBMP; 3M ESPE, St. Paul, MN, USA) + RelyX ARC luting agent (3M ESPE); G2, relined post (Filtek Z250, 3M ESPE) + SBMP + RelyX ARC; G3, individualized post (Filtek Z250) + SBMP; G4, individualized post (Filtek Bulk-Fill, 3M ESPE) + SBMP; G5, individualized post (Filtek Bulk-Fill Flow, 3M ESPE) + SBMP. In G2, the resin composite was manipulated onto the fiberglass post, positioned into the canal, and photoactivated for 3 seconds. The relined post was then removed from the canal and light-cured completely for 40 seconds. To attain individualization of the fiberglass posts, in G3, a resin spatula was used with the incremental technique (with a thickness of 2 mm) to insert the conventional resin composite around the fiberglass post that was positioned in the canal. Each layer was photoactivated for 40 seconds from the occlusal end. In contrast, in G4 and G5, the bulk-fill resin composite or bulk-fill flowable resin composite was inserted around the fiberglass post using the bulk-fill technique (with a thickness of 4 mm) and was photoactivated for 20 seconds from the occlusal end. The samples were subjected to the push-out (n = 10) and pull-out (n = 10) bond strength tests.
Push-out bond strength test
After storage for 7 days in relative humidity at 37°C, 50 roots were sectioned into nine 1-mm-thick slices (3 slices from each of the cervical, middle, and apical regions) cut perpendicularly to the long axis using a high-concentration diamond disc (Buehler, Lake Bluff, IL, USA) coupled with a precision cutting machine (Isomet 1000, Buehler). The push-out bond strengths (n = 10) were determined using a universal testing machine (Instron, Norwood, MA, USA) at a speed of 1.0 mm/min, and a cylindrical metal rod was used to exert a compressive load at the centre of the post in the apico-cervical direction until bond failure occurred [15].
The push-out bond strength value in newtons (N) was converted to megapascals (MPa) through the formula A = 2π (R2 + R1) × [h2 + (R2 − R1)]0.5, where π is a constant, h is the thickness of the slice, R2 is the cervical post radius, and R1 is the apical post radius, and was then divided by the bonded interface area (mm2) [16]. The fractured samples were subjected to scanning electron microscopy (SEM) analysis to determine the failure mode.
Pull-out bond strength test
The 50 remaining treated roots underwent the same cementation protocol (n = 10). The roots were embedded in a polystyrene resin cylinder parallel to the long insertion axis, and the fiberglass post end was fixed in an acrylic resin sphere to enable retention in another polystyrene resin cylinder. Next, a metallic hook (2.2 mm × 31 mm, Fixtil, São Paulo, SP, Brazil) was threaded onto both cylinders in order to engage each in a universal testing machine (Instron). In this machine, each cylinder underwent a tensile force at a speed of 1.0 mm/min [17]. The pull-out bond strength value in newtons (N) was converted to megapascals (MPa).
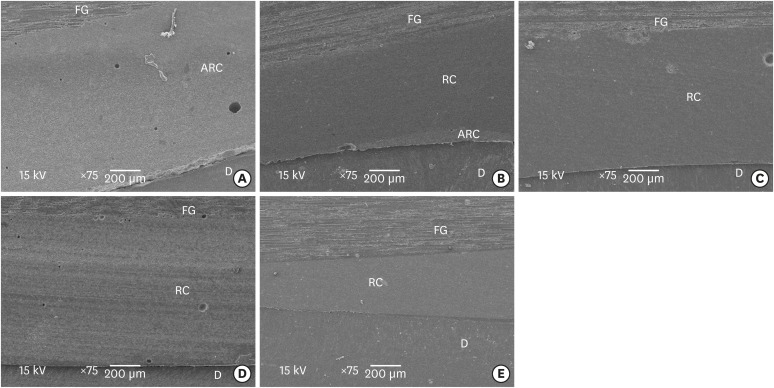
Failure mode and adhesive interface analysis
SEM was used to analyse the fracture modes of the specimens after the push-out bond strength test. The fractured surfaces were sputter-coated with gold, analysed at 15 kV (JEOL JSM-T330A, JEOL Ltd., Tokyo, Japan), and evaluated at magnifications of ×75 and ×200. The fracture modes were classified into 5 types: 1) adhesive failure between the dentine and the adhesive resin cement/resin composite; 2) adhesive failure between the adhesive resin cement/resin composite and the fiberglass post; 3) cohesive failure of the adhesive resin cement/resin composite; 4) cohesive failure of the fiberglass post; 5) mixed failure (a combination of 2 or more failure types) [18].
One sample of each group was sectioned along the longitudinal axis (in the cervical-apical direction) using a high-concentration diamond disc (Buehler) coupled with a precision cutting machine (Isomet 1000, Buehler), allowing visualization of the adhesive interface. The internal side of the sectioned specimens was polished with a silicon carbide paper (4000 grit, Buehler) and placed in an ultrasonic machine for 10 minutes (Marconi, Piracicaba, SP, Brazil). The specimens were dried for 24 hours and were sputter-coated with gold, and the cervical adhesive interfaces resulting from the different cementation protocols were analysed at ×75 magnification using SEM.
Statistical analysis
Statistical analyses were performed using SPSS version 21.0 (IBM Corp., Armonk, NY, USA). The data were tested for a normal distribution (Shapiro-Wilk test, p > 0.05) followed by the 2-way analysis of variance (ANOVA) parametric statistical test and the Bonferroni post hoc test for push-out bond strength, and the 1-way ANOVA parametric statistical test for pull-out bond strength (α = 5%).
RESULTS
The results of the test for push-out bond strength for the experimental groups are presented in Table 3. G2 and G5 presented higher values in the cervical and middle regions when compared to other groups (p < 0.001), with significant differences observed in the cervical region (p = 0.003). G3 presented the lowest results for the middle and apical regions (p = 0.023). Regarding the dentine region, it was observed that the push-out values decreased when approaching the apical region, except for G1 and G4 (p = 0.254). Regarding pull-out bond strength (Table 3), none of the groups showed a statistically significant difference (1-way ANOVA, p = 0.502).
Failure modes as determined using SEM observation are presented in Figure 1. Type 1 was in the majority among the failure modes in all groups tested, followed by mixed failure. Types 2, 3, and 4 occurred rarely. Images obtained using SEM for the adhesive interfaces resulting from the different treatment protocols are shown in Figure 2.
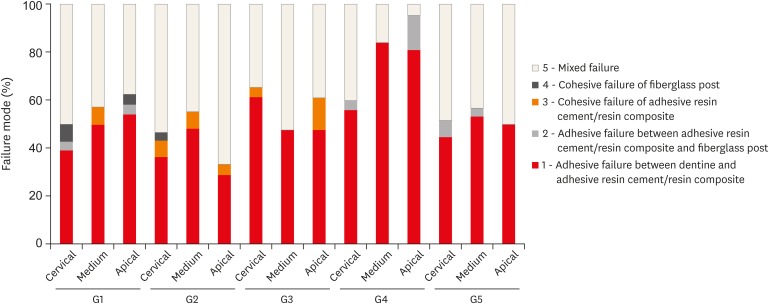
Distribution of failure modes (frequency, %) in 5 different cementation protocols and at 3 locations (the apical, middle, and cervical thirds) of the root canal dentin. The fracture modes were classified into 5 types.
G1, post + SBMP + RelyX ARC luting agent; G2, relined post (Filtek Z250) + SBMP + RelyX ARC; G3, individualized post (Filtek Z250) + SBMP; G4, individualized post (Filtek Bulk-Fill) + SBMP; G5, individualized post (Filtek Bulk-Fill-Flow) + SBMP; SBMP, Scotchbond Multi-Purpose.
DISCUSSION
The present study evaluated the bond strength of fiberglass posts obtained with cementation techniques using a conventional resin-based composite, a bulk-fill composite, and adhesive resin cement. Individualization with bulk-fill composites may be a suitable alternative technique for performing fiberglass post cementation, as it replaces resin cement without affecting the bond strength when compared to conventional resin-based composite and dual-cure adhesive resin cement.
In current dentistry, the most commonly-used and scientifically accepted fiberglass post cementation technique uses a dual-cure luting agent and an etch-and-rinse adhesive system [19], and it was therefore characterized as the first control group for this study. Using a Fiberglass post for intraradicular retention in resin-based composite restorations is currently favoured as a technique for increasing fracture resistance and stress distribution across the dentin of the entire root [20]. However, in cases of a broad root canal, a relined fiberglass post technique with a resin composite is adopted in order to decrease the thickness of the adhesive resin cement layer, greatly influencing the bond strength [21], as observed in our results. However, these techniques require marked manual dexterity of the operator, implying that they could be replaced with more efficient and practical cementation techniques; apart from this issue, adhesion of different dental materials with root dentine is still challenging [16].
Gomes et al. [22] showed that cementation techniques of intraradicular retainers with fewer steps are more favourable for obtaining better bond strength between dentine and adhesive resin cement. For this reason, an innovative cementation technique using a fiberglass post with restorative or flowable bulk-fill composites was adopted, since it eliminates the necessity of using adhesive resin cement. This technique is also favoured by the adhesion characteristics of the SBMP adhesive system [23], and it serves as a simple way to introduce the resin material within the root canal. Resin-based composites present a challenge related to high polymerization shrinkage stress, characterized by the formation of polymer chains though the conversion of carbon-carbon double bonds into single bonds [24]. This transformation induces the accumulation of stress in the adhesive layer during the polymerization process, even apart from the technique of resin-based insertion promoting higher marginal tension [24]; however, the new generation of resin-based composites (bulk-fill composites) has promising properties, such as low polymerization shrinkage stress, suitability for high C-factor cavities, the possibility of inserting a single 4–5-mm layer, greater light penetration along the thickness of the resin cement, and shorter photopolymerization time [25]. In general, the differences in retention observed among the treatment groups for push-out bond strength indicate favourable results for these resin-based materials with low polymerization shrinkage stress. This mainly applies to the bulk fill flowable group (G5), which, due to its low viscosity and appealing mechanical properties [2627], constitutes a promising technique for individualization of a fiberglass post with a resin composite, allowing it to reach the entire treated surface and induce higher bond strength along the root canal.
Evaluation of the bond strength of intraradicular retainers can be accomplished using various mechanical tests [161728]. In the current study, the push-out and pull-out bond strength tests were conducted according to typical fiberglass post cementation protocols in order to evaluate the bond strength obtained through the different methodologies under study. Push-out bond strength is most commonly used for in vitro studies involving the evaluation of specific bond strength between different root canal regions [16]. In this study, the higher push-out bond strength of the cervical and middle thirds observed compared to the apical third, with significant differences for G2, G3, and G5, can potentially be explained by the radicular dentine morphology, since variation in tubular density directly influences hybrid layer thickness and, therefore, bond strength [29]. These structural variations, as well as the technical and operational limitations on fiberglass post cementation, can be suggested as reasons for failure mode occurrence for different root canal regions [37101112]. In our study, a prevalence of adhesive failure between dentine and adhesive resin cement or resin composite and mixed failure was observed, in accordance with the scientific literature [1830]. Cohesive failure of the fiberglass post occurred rarely due to the post having similar mechanical properties to that of dentinal tissue, positively influencing its biomechanical behaviour [31]. Similarly, a low frequency of cohesive failure of the adhesive resin cement or resin composite was observed [32]. An interesting result was the absence of this failure pattern in G4 and G5, most likely due to the bulk-fill resin composite presenting a lower elastic modulus [25]. Another failure mode rarely observed was type 2, most likely because the push-out bond strength between the fiberglass post and the resin material was increased in all treatment groups due to application of a silane agent and adhesive, as observed by Machado et al. [33].
Pull-out bond strength has been used to quantify the fiberglass post bond strength in the entire root canal using parallel extrusion forces [17]. An important calculation that can be made using the pull-out test is frictional retention (the total contact area between the fiberglass post surface and the cementing material or radicular dentin), which has been adopted as a clinical measurement of the cementation technique because axial loading is the predominant form of load on clinical restorations and induces debonding as a failure mode [2134]. Nevertheless, further long-term and clinical studies are required to validate this new technique.
CONCLUSIONS
Fiberglass post cementation using restorative and flowable bulk-fill composites via the individualization of the fiberglass post displayed similar bond strength to that of a conventional resin-based composite and an adhesive resin cement. The simplified technique achieved using bulk-fill composites may be a promising alternative to current dental clinical procedures.
Notes
Funding: The authors acknowledge the financial support of FAPESP (#2016/17701-0).
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
Author Contributions:
Conceptualization: Lins RBE, Martins LRM.
Data curation: Rangel CP, Antunes TBM.
Formal analysis: Cordeiro JM.
Funding acquisition: Martins LRM.
Investigation: Lins RBE.
Methodology: Rangel C, Antunes TBM.
Project administration: Lins RBE.
Resources: Martins LRM.
Supervision: Lins RBE, Martins LRM.
Writing - original draft: Lins RBE.
Writing - review & editing: Cordeiro JM, Martins LRM.