Effect of the restorative technique on load-bearing capacity, cusp deflection, and stress distribution of endodontically-treated premolars with MOD restoration
Article information
Abstract
Objectives
To evaluate the influence of the restorative technique on the mechanical response of endodontically-treated upper premolars with mesio-occluso-distal (MOD) cavity.
Materials and Methods
Forty-eight premolars received MOD preparation (4 groups, n = 12) with different restorative techniques: glass ionomer cement + composite resin (the GIC group), a metallic post + composite resin (the MP group), a fiberglass post + composite resin (the FGP group), or no endodontic treatment + restoration with composite resin (the CR group). Cusp strain and load-bearing capacity were evaluated. One-way analysis of variance and the Tukey test were used with α = 5%. Finite element analysis (FEA) was used to calculate displacement and tensile stress for the teeth and restorations.
Results
MP showed the highest cusp (p = 0.027) deflection (24.28 ± 5.09 µm/µm), followed by FGP (20.61 ± 5.05 µm/µm), CR (17.72 ± 6.32 µm/µm), and GIC (17.62 ± 7.00 µm/µm). For load-bearing, CR (38.89 ± 3.24 N) showed the highest, followed by GIC (37.51 ± 6.69 N), FGP (29.80 ± 10.03 N), and MP (18.41 ± 4.15 N) (p = 0.001) value. FEA showed similar behavior in the restorations in all groups, while MP showed the highest stress concentration in the tooth and post.
Conclusions
There is no mechanical advantage in using intraradicular posts for endodontically-treated premolars requiring MOD restoration. Filling the pulp chamber with GIC and restoring the tooth with only CR showed the most promising results for cusp deflection, failure load, and stress distribution.
INTRODUCTION
Dental fracture can be a consequence of tooth weakening, abrasion, attrition, erosion, abfraction, caries lesions, restorative procedures, and trauma [1234]. Weakened teeth are characterized by a decrease in their volume and the loss of healthy dentin due to caries lesions and tooth preparation [15]. The most common causes of dental fractures are high-impact loads during chewing or premature occlusal contact [56]. It has been reported that dental fractures occur more frequently in teeth with large restorations than in teeth with small restorations or sound teeth [5].
Extensive restorations are often associated with endodontic treatment due to pulp vitality impairment. Endodontically-treated teeth are at a higher risk of biomechanical failure than vital teeth [7]. The factors posing the highest risk of fracture include loss of dental tissue [8], preparation of an endodontic access cavity to disinfect the root canal [6], and/or changes in the physical properties of dentin due to dehydration [8]. In cases of extensive tooth destruction, intraradicular retainers are required to provide sufficient retention for the restorative material since the dental remnant is insufficient [910]. However, the use of intraradicular posts in order to strengthen dental structure has already been reported to be ineffective [1112].
For posterior teeth with a mesio-occlusal-distal (MOD) cavity, the most suitable treatment consists of a direct restoration using composite resin due to its high bond strength to the dental substrate [3131415]. In cases where dental pulp has been compromised and endodontic treatment has been performed, the best protocol prior to performing the restoration, which may increase the resistance of the dental structure, is still not well-defined [1617]. It has been generally reported in the literature that glass ionomer cement should be used to support the composite resin restoration [1819]. Other authors have reported the use of fiberglass posts and filling the pulp chamber with resin cement [11]. Finally, some manufacturers offer pre-framed metal posts with this indication. Therefore, this study evaluated whether there were any advantages in using a prefabricated post in terms of load-bearing capacity, cusp deflection, and stress distribution of endodontically-treated human upper premolars with MOD restoration. The first null hypothesis was that different techniques would not influence the cusp deflection and load-bearing capacity of human upper premolars with MOD restoration, while the second null hypothesis was that the different restorative techniques would not influence the stress concentration in the cervical area of the teeth.
MATERIALS AND METHODS
Samples preparation
The Ethics Committee of the Institute of Science and Technology—São Paulo State University approved this study under the review protocol approval number 071/2009. Forty-eight extracted upper premolars without caries, restorations, or wear on the cusp tip that could modify their anatomy were collected and stored in saline solution for 30 days [20]. After, the teeth were marked 2 mm below the cementoenamel junction, and the root portion apical to the demarcation was inserted in polyurethane resin (Polyurethane F160, Axson, Cercy, France) [20]. All specimens received MOD-type preparations, with one-third of the intercuspal distance being respected as the maximum width. The cavity dimensions consisted of 3.8 mm bucco-lingually, 2.8 mm of height to the pulpal wall, a proximal cavity length of 2.5 mm, and a proximal box thickness of 1.5 mm. For these purposes, graphite markings were made of the preparation limits, and cylindrical diamond tips (1094, 2095, 2096, KG Sorensen, São Paulo, SP, Brazil) were used with sizes compatible with the cavities to be prepared.
The teeth were randomly distributed into 4 groups (n = 12) according to the use of endodontic treatment and restorative techniques: endodontic treatment + glass ionomer cement + composite resin (the GIC group), endodontic treatment + metallic post + composite resin (the MP group), endodontic treatment + fiberglass post + composite resin (the FGP group), and teeth restored with composite resin without endodontic treatment (the CR group) (Figure 1).
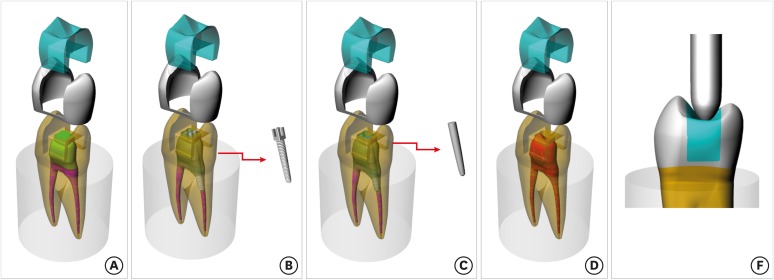
Schematic illustration of the modeled structures used in this study. The groups were distributed according to the restorative modality: (A) GIC group, glass ionomer cement + composite resin; (B) MP group, metallic post + composite resin; (C) FGP group, fiber glass post + composite resin; (D) CR group, composite resin; (E) Load application using a blunt tip of 2 mm in diameter with a load of 50 N.
GIC, glass ionomer cement + composite resin; MP, metallic post + composite resin; FGP, fiber glass post + composite resin; CR, composite resin.
Endodontic treatment
For the groups with endodontic treatment and an MOD cavity, the specimens underwent pulp chamber access preparation with a spherical diamond tip followed by the use of inactive tip drills for complete removal of the pulp chamber ceiling. All root canals were instrumented to the working length, which was defined as the total length minus 1 mm, up to the size of a #40 K-file (Dentsply Maillefer, Ballaigues, Switzerland) and staggered with Gates-Gliden drills #2 and #3 (Dentsply/Maillefer Instruments SA, Ballaigues, Switzerland). For obturation, the master gutta-percha cones (Dentsply/Maillefer) were selected according to the final diameter obtained in the biomechanical preparation. They were then placed in the canal with an endodontic resin sealer (AH Plus, Dentsply/Maillefer), spreading the cement on all the canal walls. Lateral condensation was performed with accessory gutta-percha cones (Dentsply Maillefer) with the aid of a spreader compatible with a size #30 K-file (Dentsply Maillefer) until lateral filling of the root canals was achieved, as confirmed radiographically in the mesio-distal direction. The gutta-percha cones were cut (4 mm short of the apex) with a heated endodontic condenser (Duflex, SS White, Rio de Janeiro, RJ, Brazil), and then with another cold endodontic plugger, after which the cervical accesses were cleaned with 70% alcohol (Miyako do Brasil Ind., Com., Ltd., São Paulo, SP, Brazil). The teeth were then stored in artificial saliva for 24 hours at 37°C.
Restorative treatment in each group
After endodontic treatment, the following tooth restoration procedures were performed for the teeth in each group.
1. Glass ionomer cement + composite resin (the GIC group)
The pulp chamber was sealed and filled with glass ionomer cement (Vidrion F, SS White, Rio de Janeiro, RJ, Brazil) using a Centrix syringe for restorative material injection. Next, direct composite resin restoration was performed by acid conditioning of the tooth with 37% phosphoric acid (Etch-37, BISCO Inc., Schaumburg, IL, USA) for 30 seconds in enamel and 15 seconds in dentin. Then, the tooth was washed for 20 seconds and dried with air jets. The two-step adhesive system (All Bond 3, BISCO Inc.) was used as recommended by the manufacturer. A direct restoration with microhybrid composite resin (AELITE LS, BISCO Inc.) was carried out using an incremental technique. Each increment had a maximum thickness of 2 mm and was polymerized for 40 seconds.
2. Metallic post + composite resin (the MP group)
The root canal was prepared with the aid of the drills of the metallic post system in order to maintain at least one-third of the gutta-percha obturating the root canal. After preparation, a stainless steel metallic root post (REFORPOST, Angelus Indústria de Produtos Odontológicos S/A, Londrina, PR, Brazil) was cemented with Duo-Link dual-cure resin cement (BISCO Inc.). Direct composite resin restoration was performed as in the GIC group.
3. Fiberglass post + composite resin (the FGP group)
The root canal was prepared with the D.T. LightPost Illusion drill system (BISCO Inc.), and the fiberglass post from the same system was then cemented using Duo-Link dual-cure resin cement (BISCO Inc.). Direct composite resin restoration was performed as in the GIC and MP groups.
4. Composite resin (the CR group)
The teeth in this group did not receive endodontic treatment. Thus, the sound tooth was restored following the protocol performed in the GIC, MP, and FGP groups.
Cusp deflection
Strain gauges (KFG-1-120-C1-11L1M2R, KYOWA Electronic Instruments Co., Ltd., Tokyo, Japan: resistance, 119.6% ± 0.4%Ω; gauge length, 1 mm; gauge factor, 2.08% ± 1.0%) were attached with cyanoacrylate adhesive (Super Bonder Loctite, São Paulo, SP, Brazil) in each tooth (Figure 2). The wires of the strain gauges were welded to a circuit board on which copper wires were also welded, and then attached to a terminal to capture the information generated by the devices (Model 5100B Scanner - System 5000, Inter Technology Inc., Raleigh, NC, USA). A multimeter was used to verify the absence of electric terminal defects (Minida ET 2055, Minida, São Paulo, SP, Brazil) [20]. The samples were placed on a steel base perpendicular to the ground, and a blunt tip of 2 mm in diameter was used to apply a load of 50 N for 20 seconds [20], with the tip touching the composite restoration. The generated microstrains were interpreted by specific software (StrainSmart, Inter Technology Inc.).
Load-bearing capacity
After the cusp deflection measurement, the samples underwent the load-bearing capacity test in similar conditions. A compression load was applied to each tooth assembly by a unidirectional vertical platform and loaded with a 0.5 mm/min rate until failure, which was defined as cusp fracture. The maximum load to failure was recorded in newtons [21].
Finite element analysis
The complete structures of the tooth and polyurethane resin [112223] were exported to modeling software (Rhinoceros 4.0 McNeel North America, Seattle, WA, USA). The premolar included 7.5 mm from the buccal cusp to the cementoenamel junction, 6 mm between both cusp, and 9 mm as the buccal-palatal distance. The MOD restoration consisted of a volume of 82 mm3. All materials were considered isotropic, linear, and homogeneous. The mechanical properties of the materials and structures considered in the analysis are summarized in Table 1 [242526]. The contact regions between the structures were considered to be perfectly bonded and the mesh had quadratic tetrahedral elements, being controlled by a sizing method with 0.3 mm, resulting in a total of 624,153 nodes and 462,228 elements. The aspect ratio of the mesh metrics presented an average of 1.77 with a standard deviation of 0.67. The polyurethane base was considered fixed in the three axes, and the load (50 N) was applied with a 2 mm diameter spherical tip (following the in vitro test) parallel to the principal axis to keep the analysis in the elastic field. The set displacement (mm) and maximum principal stress (MPa) for the tooth, restoration, and post were obtained. The data were summarized through colorimetric maps, which enabled visualization of the limit between each stress fringe. Tensile stress (MPa) peaks were recorded and summarized in Table 2 for a quantitative comparison.
Statistical analysis
Mean values and standard deviations were determined for each group. The normality of the data was checked by the Kolmogorov-Smirnov test. One-way analysis of variance (ANOVA) was used, followed by the post hoc Tukey test for multiple comparisons (α = 0.05) to compare the cusp deflection and load-bearing capacity. The stress data were qualitatively evaluated based on the colorimetric stress map and quantitatively evaluated using the stress peaks.
RESULTS
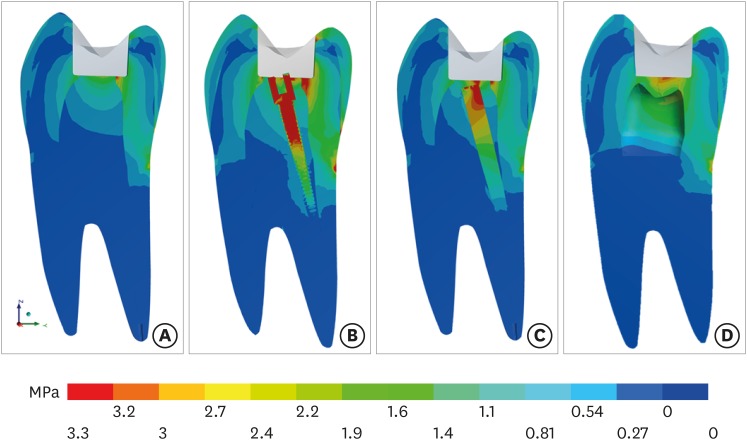
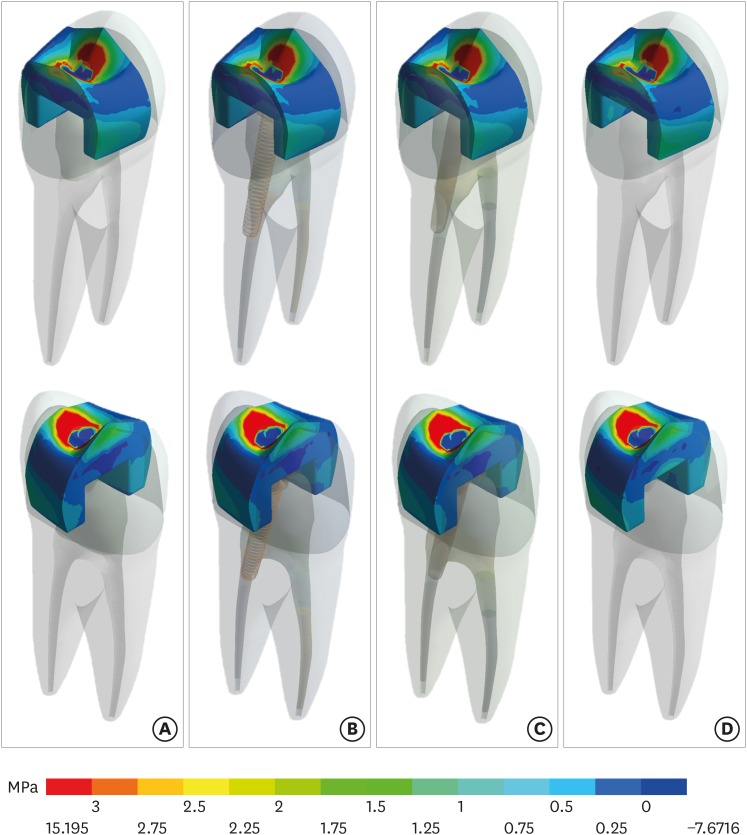
One-way ANOVA revealed that the different treatments significantly influenced the mean values of cusp deflection (p = 0.027) and load-bearing capacity (p = 0.001). The restorations using a metal post (MP group) showed the highest cusp deflection and the lowest mean value for load-bearing capacity. The GIC and CR groups showed lower mean values for cusp deflection and higher mean values for load-bearing capacity. The descriptive statistical analysis and results of the Tukey test are shown in Table 2. According to the finite element analysis, all modalities presented a similar profile for cusp linear deformation (Figure 3). However, more fringes were present in the MP group, followed by the FGP, GIC, and CR groups. In analyzing the tooth surfaces (Figure 4), it was noted that the MP group presented more areas with red color on the colorimetric stress map, meaning that it experienced the highest stress concentration. Figure 5 shows that both metallic and fiber posts concentrated more stress (metal > FGP) in the cervical area, increasing the stress concentration below the restoration compared to the GIC and CR groups. There was no significant difference among the groups in the stress distribution in the composite resin restoration (Figure 6). All groups showed the highest stress peak on the palatal surface (5.45–5.89 MPa), in comparison with the buccal face (2.51–3.23 MPa). The results are summarized in Table 2.
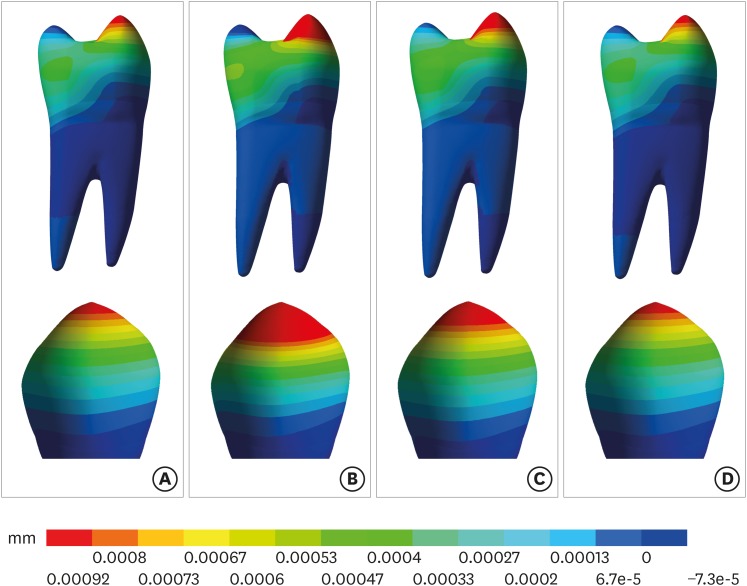
Results of cusp linear deformation (mm) according to the restorative modality: (A) GIC group, glass ionomer cement + composite resin; (B) MP group, metallic post + composite resin; (C) FGP group, fiber glass post + composite resin; (D) CR group, composite resin.
GIC, glass ionomer cement + composite resin; MP, metallic post + composite resin; FGP, fiber glass post + composite resin; CR, composite resin.
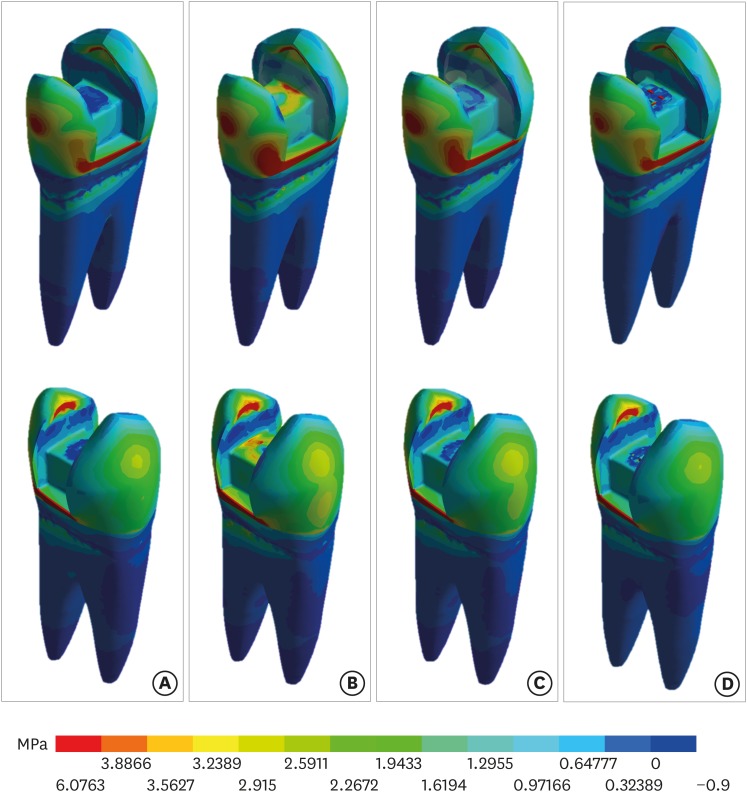
Results of maximum principal stress (MPa) in the tooth according to the restorative modality: (A) GIC group, glass ionomer cement + composite resin; (B) MP group, metallic post + composite resin; (C) FGP group, fiber glass post + composite resin; (D) CR group, composite resin.
GIC, glass ionomer cement + composite resin; MP, metallic post + composite resin; FGP, fiber glass post + composite resin; CR, composite resin.
Results of maximum principal stress (MPa) in the root dentin and post according to the restorative modality: (A) GIC group, glass ionomer cement + composite resin; (B) MP group, metallic post + composite resin; (C) FGP group, fiber glass post + composite resin; (D) CR group, composite resin.
GIC, glass ionomer cement + composite resin; MP, metallic post + composite resin; FGP, fiber glass post + composite resin; CR, composite resin.
Results of maximum principal stress (MPa) in the restoration according to the restorative modality: (A) GIC group, glass ionomer cement + composite resin; (B) MP group, metallic post + composite resin; (C) FGP group, fiber glass post + composite resin; (D) CR group, composite resin.
GIC, glass ionomer cement + composite resin; MP, metallic post + composite resin; FGP, fiber glass post + composite resin; CR, composite resin.
DISCUSSION
This study aimed to evaluate the influence of prefabricated posts on cusp deflection, load-bearing capacity, and stress distribution in endodontically-treated upper human premolars with a MOD restoration. The microstrain results showed statistically significant differences among the experimental groups, leading the first null hypothesis to be rejected. The stress distribution results showed different values among the evaluated treatments, causing the second null hypothesis to be rejected.
Restoration of teeth with composite resin without endodontic treatment has already been reported to show promising mechanical behavior [2728]. These previous studies have suggested that composite resin restoration decreases cusp deflection. This can be explained through the adhesive characteristics of this type of restoration, which partially restore the rigidity of the dental element through adequate bond strength at the tooth/restoration interface [29].
Finite element analysis showed that the mechanical behavior was very similar across all groups in an ideal situation in which the adhesive interface is perfectly bonded between the tooth and restoration (Figure 6). Thus, the possibility of dental fracture due to stress concentration in the dental structure seems to be more influenced by the restorative treatment after endodontic access than by marginal infiltration along the restoration. Figure 4 shows that the palatal cusp was the most susceptible to fracture in response to a load being exerted on the restorative material. This finding is in agreement with previous studies that evaluated the biomechanical behavior of healthy [22] and restored teeth [23] using finite element analysis. In addition, it is important to note that intraradicular posts are often indicated for palatal canals [11], which further contributes to this cusp being stressed during masticatory load. This effect is even greater for metal posts than fiberglass posts (Figures 3 and 4).
Glass ionomer cement is used as a base material for restorations because its mechanical properties are similar to those of dentin [1930]. This advantage is reflected in our results, in which the teeth that had their pulp chamber filled with glass ionomer cement and were directly restored with composite resin presented similar cusp deflection values to those restored with composite resin without endodontic treatment (Table 2). The good performance of glass ionomer cement as a substitute for lost dentin during access opening for endodontic treatment obtained in this study is in agreement with previous studies [2431] which indicated that glass ionomer cement is a suitable material to be used under a composite resin restoration.
The use of a metallic post inside the root canal, in addition to removing more dental tissue [11], means that a non-adhesive restorative material is in contact with the composite resin and the remaining structures; this increases the possibility of cusp movement, and thereby elevates the risk of tooth fracture. The results showed a significance difference between the group restored with a metal post and the group restored with a fiberglass post (Table 2). In addition, as shown in Figure 5, a higher stress concentration was present below the restoration in both groups with an intraradicular post than in the GIC and CR groups, with larger zones of red color for the MP group. This fact corroborates previous reports that fiber posts are preferable to prefabricated metal posts [32]. A correlation between the cusp deflection and fracture resistance values could also be observed, which has also been reported in the literature [3334].
The group that presented the highest cusp deflection means herein also showed the lowest load-bearing capacity. Despite the results of the present study, it is worth noting that it has limitations because it is a laboratory study. The effects of cyclic fatigue, oblique load in the restoration [35], thermal aging [36], different composite materials [37] and sliding occlusal loads can modify the mechanical behavior of restored teeth, thereby weakening the adhesive strength and altering the final results. Moreover, pH variation and defects in the restorative material, such as bubbles within the restoration, were not reproduced in the numerical simulation, as ideal conditions of a homogeneous (without bubbles or defects in the cement or composite) and isotropic material were assumed. Another important limitation of this study is that the finite element simulation was performed with general materials, using mechanical properties reported in the literature [192425]. However, the values used in this study cannot represent the mechanical properties of the current in vitro materials during the strain gauge analysis. This simplification was present for all groups; for that reason, the mechanical behavior may not present precisely the same values for each method, but the same profile is likely to be observed. Finally, even though the results are valid, they should be extrapolated with care and explored in future longitudinal clinical studies to define the best clinical approach.
CONCLUSIONS
There is no mechanical advantage in using intraradicular posts when an endodontically-treated premolar requires MOD restoration. Filling the pulp chamber with glass ionomer cement and restoring the tooth with only composite resin showed the most promising results in terms of cusp deflection, failure load, and stress distribution.
ACKNOWLEDGEMENTS
The first author acknowledges the Coordination for the Improvement of Higher Education Personnel (CAPES) for financial support in the form of a scholarship.
Notes
Author Contributions:
Conceptualization: Rocha DM, Tribst JPM, Borges ALS.
Data curation: Rocha DM, Tribst JPM, Ausiello P, Dal Piva AMO.
Formal analysis: Rocha DM, Tribst JPM, Ausiello P, Dal Piva AMO, Rocha MS, Di Nicoló R, Borges ALS.
Methodology: Rocha DM, Tribst JPM, Dal Piva AMO.
Project administration: Rocha DM, Tribst JPM, Ausiello P, Dal Piva AMO, Rocha MS, Di Nicoló R, Borges ALS.
Supervision: Rocha DM, Ausiello P, Di Nicoló, Borges ALS.
Writing - original draft: Rocha DM, Tribst JPM, Ausiello P, Dal Piva AMO, Rocha MS.
Writing - review & editing: Rocha DM, Tribst JPM, Dal Piva AMO, Borges ALS.





