A CAD/CAM-based strategy for concurrent endodontic and restorative treatment
Article information
Abstract
This case report describes a technique in which endodontic treatment and permanent indirect restoration were completed in the same clinical appointment with the aid of a computer-aided design/computer-aided manufacturing (CAD/CAM) system. Two patients were diagnosed with irreversible pulpitis of the mandibular first molar. After access preparation, root canals were located, irrigation was performed until bleeding ceased, and the coronal tooth structure was prepared for indirect restoration. Then, utilizing an interim 3-mm build-up of the endodontic access cavity, a hemi-arch digital scan was performed with an intraoral scanner. Subsequent to digital scanning, restoration design was performed simultaneously with the endodontic procedure. The root canals were shaped using the Race system under irrigation with 2.5% sodium hypochlorite followed by root canal filling. The pulp chamber was subsequently filled with a 3-mm-thick composite resin restoration mimicking the interim build-up previously utilized to facilitate block milling in the CAD/CAM system. Clinical try-in of the permanent onlay restoration was followed by acid etching, application of a 5th generation adhesive, and cementation of the indirect restoration. Once the restoration was cemented, rubber dam isolation was removed, followed by occlusal adjustment and polishing. After 2 years of follow-up, the restorations were esthetically and functionally satisfactory, without complications.
INTRODUCTION
High-quality and timely placement of the coronal restoration is a factor determining the long-term success of endodontically treated teeth. An inadequate coronal seal contributes to microbial infiltration [1] and may necessitate endodontic retreatment [2]. Once endodontic treatment is completed, restorative procedures are carried out, taking into account functional characteristics and biomechanical factors such as canine guidance, group function, occlusion type, overjet, overbite, presence or absence of parafunction, thickness of the remaining walls, dimension of the cavity, and the occlusal surface [3]. Onlay restorations are indicated when the ratio between cusp length and cusp diameter is greater than 1:2 [4]. Cusp overlay preserves tooth structure when compared to full-coverage crowns, in addition to its ability to provide greater resistance to fracture when compared to direct adhesive restorations, which increases the longevity of the restored root-filled tooth [3].
Computer-aided design/computer-aided manufacturing (CAD/CAM) is a technology that has been used in dentistry in recent years [56] to enable single-session indirect restorative procedures [78]. The rapid milling process minimizes the waiting time between the preparation and cementation of the restoration [9], thereby eliminating the need for temporary restorations [8]. A variety of materials can be employed, from ceramics (silica or various silicates) to composite resins [10]. Ceramic materials are recommended for onlay restoration. When used with a CAD/CAM system, these materials reduce the fabrication time by up to 90% when compared to conventional methods of fabrication [10]. Furthermore, recent studies have shown that the use of ceramic blocks made with a CAD/CAM system allows better internal adaptation than when composite resin blocks are used [11].
The current literature suggests that endodontic therapy in cases of vital pulp can be performed in a single clinical appointment [12]. Additionally, the success of endodontic treatment in these cases is related to the duration of the restorative procedure [13]. Considering that in cases of vital pulp the endodontic treatment can be performed in a single session [1214] and that CAD/CAM technology allows the fabrication of onlay restoration in a short period of time, the purpose of this study was to present cases in which both endodontic treatment and onlay restoration using leucite-enhanced feldspathic ceramics and a CAD/CAM system were completed in a single clinical session.
CASE REPORTS
Case 1
A 28-year-old female patient presented with spontaneous and continuous pain in tooth #36. Clinically, there was an occlusal restoration, absence of the periodontal pocket, and missing teeth generally. Clinical tests indicated negative palpation and percussion tests, and a positive vitality test with a slow decline in pain. A diagnosis of irreversible pulpitis in tooth #36 was made, with endodontic treatment being indicated. Bearing in mind the presence of canine guidance and the absence of parafunction (Figure 1), endodontic treatment followed by permanent indirect restoration with the aid of the CAD/CAM system in the same clinical session was planned. The patient's consent was obtained.
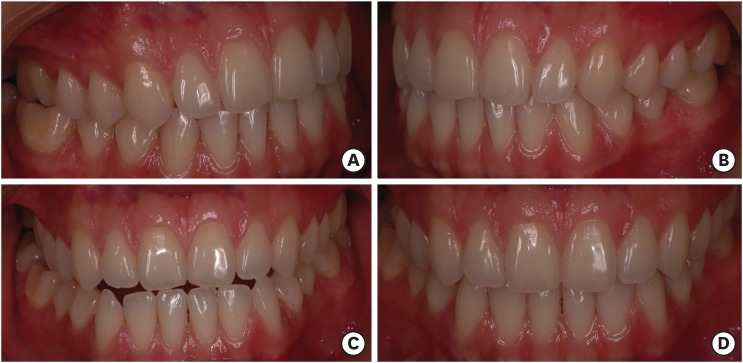
Biomechanical considerations. (A) Right lateral view: canine guidance in lateral excursion; (B) Left lateral view: canine guidance in lateral excursion; (C) Anterior view: protrusion; (D) Anterior view: maximum intercuspation.
Initially, the antagonist hemi-arch and occlusal registration scans were completed using an intraoral scanner Sirona CEREC AC Omnicam (Dentsply Sirona, Bensheim, Germany) to determine intermaxillary relationships and to enable shade and ceramic block selection using the Empress CAD Multi A2 system (Ivoclar Vivadent AG, Schaan, Liechtenstein) (Figure 2). Following inferior alveolar nerve block (2% mepivacaine), rubber dam isolation, surgical access with the Drill Kit for access (Jota AG, Rüthi, Switzerland) and the Ultrasound Tip Kit (Helse, Santa Rosa de Viterbo, SP, Brazil), root canal localization, cervical preparation, and pulp removal and irrigation until cessation of bleeding were performed. In the absence of bleeding, the previous restoration was removed, and the cavity was prepared with tapered truncated diamond drills (KG Sorensen, Cotia, SP, Brazil), determining the expulsive walls, rounded internal angles, and the high cavosurface angle with reduction of the 2 distal cusps to receive the onlay restoration.
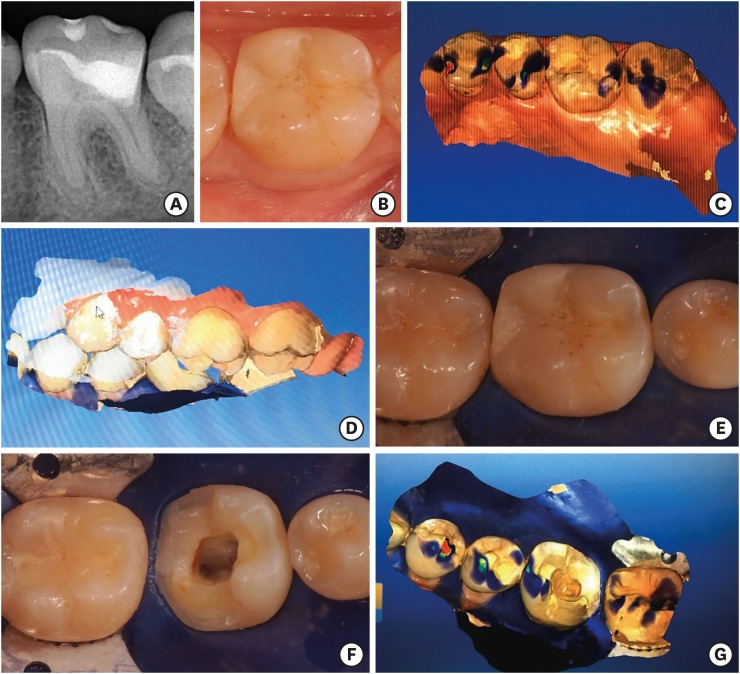
Restorative treatment planning. (A) Preoperative radiograph of tooth #36; (B) Preoperative photograph; (C) Hemi-arch antagonist scan; (D) Hemi-arch occlusal registration scan; (E) Isolated tooth #36 before surgical access; (F) Isolated tooth #36 after surgical access and onlay preparation; (G) Hemi-arch scan for computer-aided design/computer-aided manufacturing onlay fabrication with rubber dam isolation in place.
In order to allow the preparation to be scanned without undercuts, a provisional layer of approximately 3 mm of Clip F resin (VOCO, Cuxhaven, Germany) was placed in the pulp chamber, without any previous surface treatment. The resin was photopolymerized for 45 seconds with a Valo LED Curing Light photopolymerizer (Ultradent Products Inc., South Jordan, UT, USA). Subsequently, intraoral scanning, designing, and fabrication of the prosthetic piece were performed using the CAD/CAM system.
After the scanning, the temporary resin was easily removed with a resin spatula, and there was no treatment of the dentin surface prior to placement. The root canal lengths were established and the biomechanical preparation of the root canals was performed using the Race system (FKG Dentaire, La Chaux-de-Fonds, Switzerland), following the size sequence of 15/0.06, 25/0.04, 30/0.04, 25/0.06, and 35/0.04 for the mesial canals and up to size 40/0.04 for the distal canal. Irrigation between each instrument was performed with 2.2 mL of 2.5% sodium hypochlorite (NaOCl) with a plastic syringe and a 30 G NaviTip (Ultradent Products Inc.), and final irrigation was performed with 2.5% NaOCl, activated 3 times for 20 seconds with ultrasound and an Irrisafe tip at a power setting of 1 (Satelec Acteon, Merignac, France), followed by 18% ethylenediaminetetraacetic acid for 3 minutes (File-Eze, Ultradent Products Inc.) and 2.5% NaOCl with an INP needle (Mikuni Kogyo Co., Inc., Nagano, Japan). The root canals were dried with sizes 35 and 40 absorbent paper points (Hygienic, Coltene, Rio de Janeiro, RJ, Brazil) and filled using the hybrid Tagger technique with a calibrated M cone (Hygienic, Coltene) and AH Plus resin cement (Densply Detrey, Konstanz, Germany) (Figure 3). The cones were then cut at the entrance of each root canal at the level of 1 mm below the furcation region, the cavity was cleaned, and the surface was treated with an antioxidant agent (sodium thiosulfate; Na2S2O3) for 1 minute [1516].
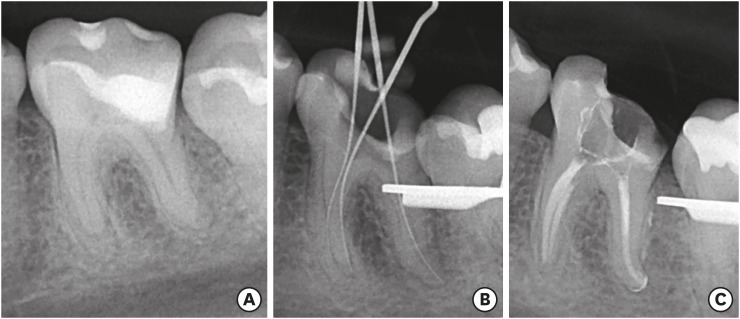
Root canal treatment. (A) Preoperative radiograph; (B) Determination of root canal length; (C) Post-obturation radiograph.
To establish a coronal seal and cementation, 37% phosphoric acid was applied for 15 seconds in dentin and 30 seconds in enamel, it was washed for 10 seconds, and the cavity was air-dried. Then, 5th generation Excite adhesive (Ivoclar Vivadent AG) was applied to the dentin using a disposable microbrush. Excess adhesive was removed with air spray for 5 seconds, and LED light activation for 10 seconds was completed. Approximately 3 mm of Tetric N Ceram flow resin (Ivoclar Vivadent AG) was placed to cover the root canal entrance and pulp chamber region according to the interim resin placed earlier, which had enabled scanning of the onlay preparation prior to the endodontic treatment.
Concurrent with the endodontic treatment, the indirect restoration was designed using the Cerec 4.1 program and IPS Empress II ceramic system (Ivoclar Vivadent AG). The stages included aligning the digital scan in the digital articulator, using the digital die model to mark the margins, assigning the path of insertion, and designing the form of the permanent indirect restoration within the CAD/CAM software. Onlay fabrication was finished by milling the Empress CAD Multi A2 block (Ivoclar Vivadent AG) in a MCXL Milling Machine (CEREC, Dentsply Sirona).
Following root canal obturation and placement of the 3 mm resin layer, clinical try-in of the ceramic onlay was carried out to assess for fit, including correct seating, marginal adaptation, and adequacy of proximal contact. Subsequently, the final restoration was conditioned with 10% hydrofluoric acid for 60 seconds, washed with water and air, air-jet dried, and treated with an application of silane using a microbrush for 1 minute followed by application of Helio bond adhesive (Ivoclar Vivadent AG). Without removing the rubber dam isolation, the ceramic onlay was cemented using Variolink N dual cement (Ivoclar Vivadent AG). After removal of the isolation, occlusal contact was verified, followed by finishing and polishing of the margins with Soflex discs (3M ESPE, St. Paul, MN, USA) and final radiography (Figure 4D and 4E). At 2 years of follow-up, the restoration was esthetically and functionally satisfactory, without complications (Figure 4F and 4G).
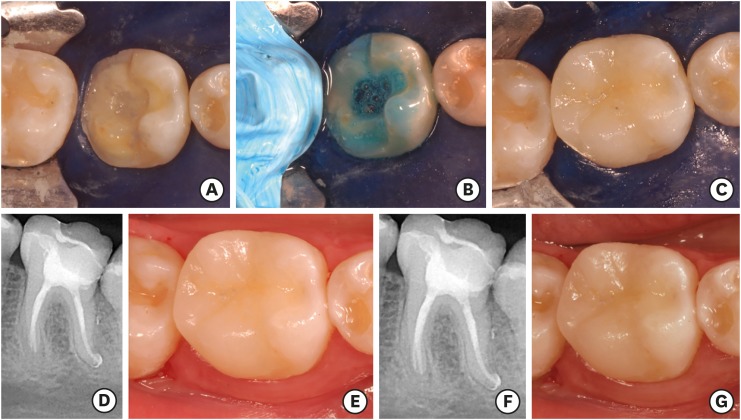
Restorative treatment. (A) Pulp chamber sealed with resin; (B) Acid conditioning; (C) Onlay restoration cemented; (D) Post-onlay cementation radiograph; (E) Onlay restoration in situ after polishing; (F) Radiograph taken 2 years after treatment; (G) Onlay restoration in situ after 2 years of function.
Case 2
A 27-year-old female patient presented with spontaneous and continuous pain in tooth #46. Clinically, there was an unsatisfactory glass ionomer restoration, which was radiographically assessed to extend deep pulpally in tooth #46, with a normal periodontal pocket and no missing teeth. Clinical tests indicated negative palpation and percussion tests, and a positive vitality test with slow pain decline in tooth #46, indicating a diagnosis of irreversible pulpitis for which endodontic treatment was necessary. Considering the presence of canine guidance and absence of parafunction (Figure 5), endodontic treatment followed by permanent indirect restoration with the aid of CAD/CAM in a single clinical session was planned. The patient's consent was obtained.
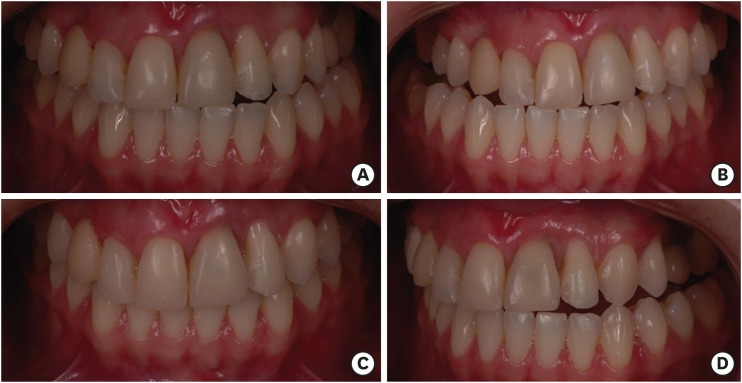
Biomechanical considerations. (A) Anterior view: maximum intercuspation; (B) Right lateral view: canine guidance in lateral excursion; (C) Anterior view: protrusion; (D) Left lateral view: canine guidance in lateral excursion.
To commence the treatment, the antagonist and maximum intercuspation hemi-arch intraoral scans were obtained and analyzed to determine the intermaxillary relationships and for shade and ceramic block selection (Figure 6C). Subsequently, the protocol followed was as described in for case 1. Initially, inferior alveolar nerve block was performed, followed by rubber dam isolation, surgical access, root canal localization, cervical preparation, pulp removal, and irrigation until cessation of bleeding (Figure 6D). Removal of the previous restoration and preparation of the cavity with capping of the mesiobuccal, mesiolingual, and distolingual cusps to receive an onlay restoration followed. As in case 1, an interim layer of 3 mm of resin was inserted over the root canal orifices and pulp chamber to enable the preparation to be scanned without undercuts, allowing fabrication of the permanent ceramic onlay during the root canal biomechanical preparation and obturation procedures. Subsequently, scanning (Figure 6E), design, and milling of the onlay were performed. The provisional resin was removed and the endodontic treatment was performed (Figure 7), followed by placement of a 3-mm resin layer over the root canal orifices and pulp chamber. The restoration fit, seating, marginal adaptation, and proximal contacts were assessed clinically, and without removing the isolation, the restoration was cemented (Figure 8). After removal of the isolation, occlusal contact was verified, followed by finishing and polishing of the margins and final radiography (Figure 8D and 8E). At 2 years of follow-up, the restoration was esthetically and functionally satisfactory, without complications (Figure 8F and 8G).
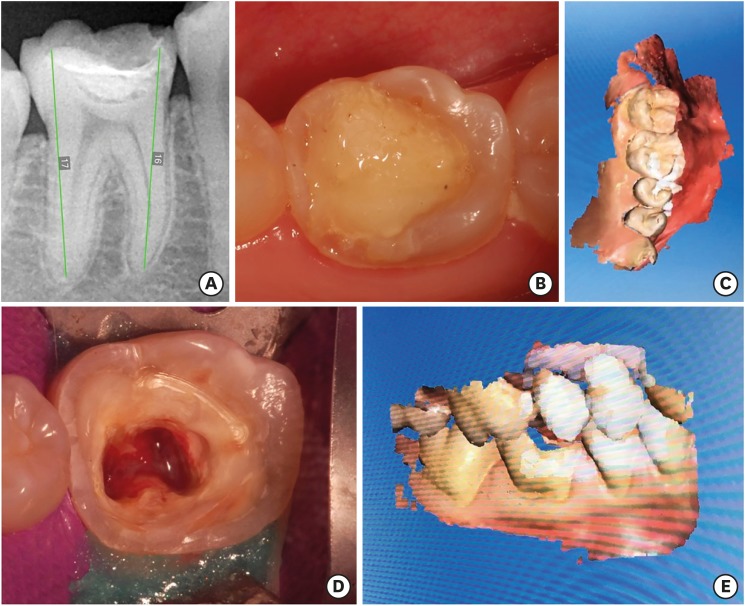
Restorative treatment planning. (A) Preoperative radiograph of tooth #46; (B) Preoperative photograph; (C) Hemi-arch antagonist scan; (D) Isolated tooth #46 after surgical access and onlay preparation; (E) Hemi-arch occlusal registration scan.
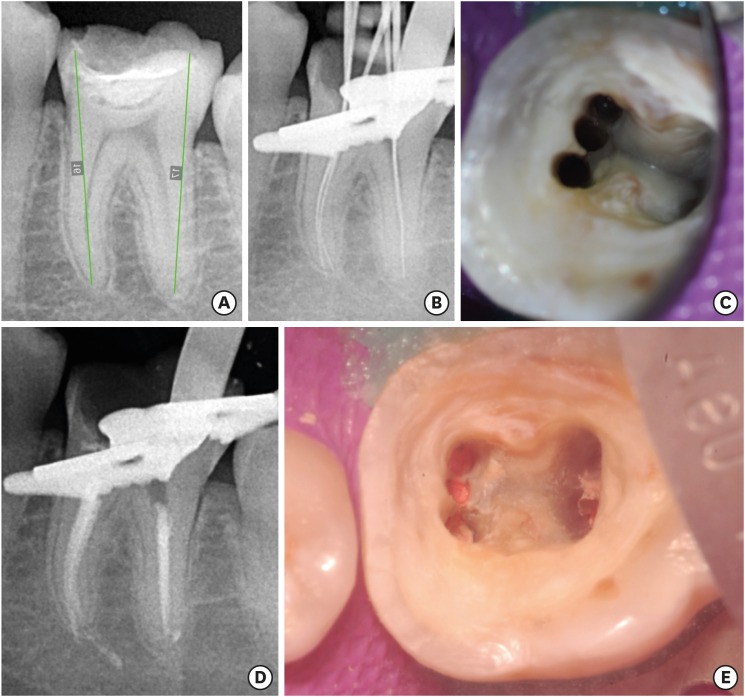
Root canal treatment. (A) Preoperative radiograph; (B) Determination of root canal length; (C) Post-root canal preparation photograph; (D) Post-obturation radiograph; (E) Post-obturation photograph.
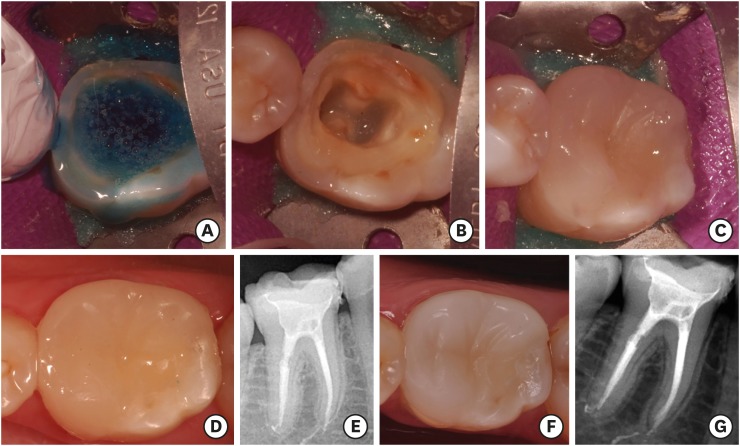
Restorative treatment. (A) Acid conditioning; (B) Pulp chamber sealed with resin; (C) Onlay restoration cemented; (D) Onlay restoration in situ after polishing; (E) Post-onlay cementation radiograph; (F) Onlay restoration in situ after 2 years of function; (G) Radiograph taken 2 years after treatment.
DISCUSSION
Restorative treatment of endodontically treated teeth generally consists of fabrication of indirect restorations, which requires great loss of coronal tooth structure. To this end, 2 separate clinical sessions are conventionally considered necessary to fabricate a temporary restoration and allow for a laboratory phase. However, previous studies have highlighted that a permanent restoration should be performed as soon as possible after the completion of endodontic treatment [117]. Early placement of a permanent restoration helps to avoid recontamination of the root canal system [18] from the loss of the coronal seal between clinical appointments, and also reduces the risk of fracture in root-filled teeth [1920].
The CAD/CAM system used in the current study allowed the endodontic treatment and the restorative treatment to be accomplished in a single session by reducing the time required for fabrication of the indirect restorations, as well as circumventing the step of temporary restorations. Additionally, CAD/CAM-based indirect restorations have been found to promote greater early marginal adaptation and a tighter coronal seal due to low polymerization stress between the restoration and tooth structure [2122]. It should be emphasized that for the proposed technique to be successfully carried out, it is necessary to plan and execute a specific protocol. Occlusal registration, analysis of biomechanical factors, and scanning of the antagonists must be performed prior to absolute isolation, allowing uninterrupted use of the rubber dam from the beginning of the endodontic treatment to the end of cementation of the indirect restoration. Importantly, the isolation step should not just involve the tooth to be treated endodontically, but also the adjacent teeth in order to avoid contamination during the endodontic treatment and restorative procedures [2324]. Correspondingly, Yadav et al. [25] reported clinical cases in which isolation was not considered during the cementation phase, which may favor recontamination of the treated root canals.
The previous literature suggests that in cases of vital pulpectomy, intracanal medication between clinical sessions is not mandatory, and if there is no suspicion of loss of asepsis during endodontic treatment, the ideal approach would be to perform immediate obturation of the root canal system in a single session [121426], as was performed in the present study. Considering that in the 2 cases presented, endodontic therapy was planned with a simultaneous permanent restorative procedure for teeth that exhibited positive preoperative pulp sensibility responses, it is important to emphasize the need to stop the bleeding after the pulp removal to allow the placement of the provisional interim resin layer in the pulp chamber, thereby enabling accurate intraoral scanning of a restorative preparation free of undercuts. It should be noted that no pre-treatment of the dentin was performed (e.g., acid etching or adhesive placement) prior to placement of the interim resin. Therefore, in the absence of adhesion between the resin and dentin surface, it was easy to remove the interim resin buildup from the pulp chamber with the aid of a cement spatula [27].
Race instruments were used for shaping the root canals. These instruments have a triangular cross-sectional design, with alternating sharp cutting edges that may increase cutting efficiency and produce centralized preparation [2829]. Preparation was performed until size 35/0.04 instrumentation for the mesial canals and size 40/0.04 for the distal canal, allowing the removal of at least 150 μm of dentin from the root canal walls [30], which is at least 3 instrument sizes larger than the initial instrument [31].
Concurrent to the endodontic treatment, the laboratory phase of the onlay restoration was performed using feldspar ceramics reinforced by leucite, since it presents greater fluorescence, compression, and wear resistance than composite resins, with a similar coefficient of thermal expansion to dental structures, similar biocompatibility [3233], and lower polymerization contraction [323435]. Moreover, according to Dalpino et al. [36], indirect ceramic restorations in large cavities present greater fracture resistance than direct resin restorations. Therefore, the use of leucite-reinforced feldspathic ceramics was chosen, since both clinical cases presented had extensive restorations with cusp overlays. As indirect restoration procedures such as onlays, overlays, and inlays aim to preserve a greater amount of dental tissue by avoiding the use of intraradicular retainer [37], adhesion is a crucial step in the clinical protocol [38]. Thus, the cementation of the onlay restoration was performed with a fifth-generation adhesive, as well as the previous filling of the cavity with a 3 mm resin layer, a step that aimed to provide a favorable cavity geometry and better adaptation of the onlay restoration [39] as well as a lower thickness of ceramic, allowing the greater passage of light for the cement polymerization [4041]. This protocol allowed the minimization of clinical steps and possible technical errors.
Adhesion immediately after root canal filling can reduce the bond strength of composite materials, since NaOCl, a chemical substance used during biomechanical preparation, can adversely affect the dentin and its interactions with adhesive restorative materials [1516]. However, recent studies have shown that neutralization of the NaOCl oxidizing effect on the dentin surface through the application of antioxidant solutions such as sodium thiosulfate before the adhesive procedure can restore the compromised bond strength [1516].
The fifth-generation adhesion system consists of 2 steps: first, application of an acidic conditioning agent; and second, application of a self-priming adhesive, in which a hydrophilic primer that makes the surface more receptive to adhesion is contained in a single bottle together with a hydrophobic adhesive that binds the complex enamel/dentin and primer to the restoration [42]. Although this adhesive system eliminated a clinical step, comparable properties were observed with a fourth-generation adhesive system [43]. Ernest et al. [43], when comparing the bond strength between fourth- and fifth-generation dentin adhesives, verified that they had similar average shear strength. After conditioning and application of adhesive to the prepared walls, the indirect restorations were cemented with dual-cure resin cement [44]. This allowed the procedure to be accomplished in 1 step, resulting in a reduction of clinical time and simplification of the technique, thereby reducing the probability of errors [45].
After the removal of the absolute isolation, occlusal adjustment was performed, obtaining restorations that were functionally and morphologically adapted in a short period of time. Kollmuss et al. [5], when comparing the original morphology of the teeth and the number of occlusal contacts between the restorations performed by the CAD/CAM and conventional ceramic crowns, showed that there was a reduced need for occlusal adjustments in the crowns made using the CAD/CAM system. By reducing the time needed to fabricate indirect restorations, CAD/CAM technology facilitates completion of endodontic and restorative treatment in a single session. The technique described in this case report 1) avoids the use of inter-appointment temporary crowns, 2) promotes a better early seal between the restoration and the tooth structure, and 3) allows mechanical stability by facilitating cementation and occlusal adjustment of the permanent indirect restoration immediately following endodontic treatment. However, careful treatment planning and following specific treatment protocols are critical for a successful outcome.
CONCLUSIONS
CAD/CAM technology enabled endodontic and restorative treatment in a single session, without the need for temporary restorations, thereby restoring function and preventing coronal microleakage and fracture of the teeth. After 2 years of follow-up, the restorations were esthetically and functionally satisfactory, without complications.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
Author Contributions:
Conceptualization: Escobar PM, Sousa-Neto MD.
Formal analysis: Kishen A, Sousa-Neto MD.
Project administration: Lopes FC, Sousa-Neto MD.
Resources: Escobar PM, Kegler EG.
Supervision: Sousa-Neto MD.
Writing - original draft: Escobar PM, Lopes FC, Borges CC, Kegler EG.
Writing - review & editing: Kishen A, Lopes FC, Sousa-Neto MD.
