Unwanted effects due to interactions between dental materials and magnetic resonance imaging: a review of the literature
Article information
Abstract
Magnetic resonance imaging (MRI) is an advanced diagnostic tool used in both medicine and dentistry. Since it functions based on a strong uniform static magnetic field and radiofrequency pulses, it is advantageous over imaging techniques that rely on ionizing radiation. Unfortunately, the magnetic field and radiofrequency pulses generated within the magnetic resonance imager interact unfavorably with dental materials that have magnetic properties. This leads to unwanted effects such as artifact formation, heat generation, and mechanical displacement. These are a potential source of damage to the oral tissue surrounding the affected dental materials. This review aims to compile, based on the current available evidence, recommendations for dentists and radiologists regarding the safety and appropriate management of dental materials during MRI in patients with orthodontic appliances, maxillofacial prostheses, dental implants, direct and indirect restorative materials, and endodontic materials.
INTRODUCTION
Imaging is an integral step in diagnosis in medicine and dentistry. Conventional radiographic methods (intraoral radiographs, orthopantomograms) have inherent limitations, since they capture 3-dimensional anatomy on a 2-dimensional image and because they involve ionizing radiation. Advanced imaging techniques include computed tomography (CT), cone-beam CT, magnetic resonance imaging (MRI), ultrasonography, and positron emission tomography [12]. MRI, when indicated, is advantageous over other imaging techniques because it provides high spatial resolution images of hard and soft tissues, the images are obtained in various planes, and it involves no ionizing radiation, unlike intraoral radiographs and CT scans [3].
MRI creates images using a strong uniform static magnetic field and radiofrequency pulses [4]. When placed in a magnetic field, all substances are magnetized to a degree that depends on their magnetic susceptibility [45]. Unfortunately, variations in the magnetic field strength that occur at the interface between dental materials and the adjacent tissue can lead to spatial distortions and signal loss, thereby generating an artifact in the image [6]. Apart from artifact formation, other unwanted effects of MRI are radiofrequency heating (a physical effect) and magnetically-induced displacement (a mechanical effect) of the dental material [7].
In addition to the medical applications of MRI, newer approaches have been proposed in various branches of dentistry with regard to MRI applications, including in the fields of endodontics, caries diagnosis, prosthodontics, and orthodontics [89101112131415]. However, information on the capacity of dental materials to induce unwanted effects is not readily available.
REVIEW
A search in PubMed and Google Scholar was conducted using the keywords ‘safety’, ‘artefacts’, ‘artifacts’, and ‘magnetic resonance imaging’. Only articles from dental journals were selected. No restrictions were used regarding the language of the articles. The literature search yielded 81 articles from 1988 to 2018, of which 45 were found to be relevant. In addition to the articles in the English language, 3 were in Chinese, 2 in French, and 1 in German. There were 3 case reports, 14 clinical studies, and 22 in vitro studies. There were also 3 review articles (Sinkiewicz et al. [7], Hubálková et al. [16], Hu et al. [17]), and 1 letter to the editor (Hunt et al. [18]).
Mechanism of MRI
MRI creates detailed images of organs and tissues within the body using a strong uniform static magnetic field and radio waves [4]. The images are constructed from the rate of decay or relaxation of proton resonance in a plane longitudinal (T1 images) or transverse (T2 images) to the magnetic field plane. Modern MRI machines use magnets with a field strength of 0.5–2 tesla (T). The strength of the magnet is directly proportional to its sensitivity in detecting small lesions [19]. Most MRI machines are large tube-shaped magnets that align the water molecules in the body, which in turn produce signals through the induction of radio waves. The result is the creation of cross-sectional magnetic resonance (MR) images [20].
Types of unwanted effects
The potential unwanted effects caused by the interaction of MRI and dental materials fall into 3 broad categories (Table 1) [20212223].
1. Artifact formation in MRI
An MRI-induced artifact is defined by pixels that do not faithfully represent the tissue components under study [23]. The shape of the artifact (elicited by a cubic sample) depends on the scanning plane. Artifacts have a circular pattern when scanned in the axial plane, and a ‘clover-like’ pattern in the sagittal plane [24]. Artifact severity depends on the following factors: the magnetic properties of the metal object that causes the artifact; the shape, position, orientation, and number of objects; the homogeneity of the alloy; the MRI sequence; and the sequence parameters used [68].
Owing to differences in the magnetic susceptibility of human tissues and dental alloys, metallic dental restorations produce serious artifacts, especially in maxillofacial imaging [23]. Alloys may behave very differently from ‘pure’ metals, and manufacturers are often reluctant to disclose the composition of their ‘trademark’ alloys [721]. The literature contains contradictory results regarding the severity of image artifacts caused by different dental materials such as high gold-content alloys, titanium, and dental amalgam [825262728293031323334]. If a material is capable of causing an artifact on a scan, it can do so on a ‘slice’ of the scan several sections distant from the slice that contains the material [29]. Whether materials cause strong artifacts, moderate artifacts, or no effect strongly depends on the specific application. For example, a material that is compatible with brain MRI can severely affect the quality of orofacial MRI [8].
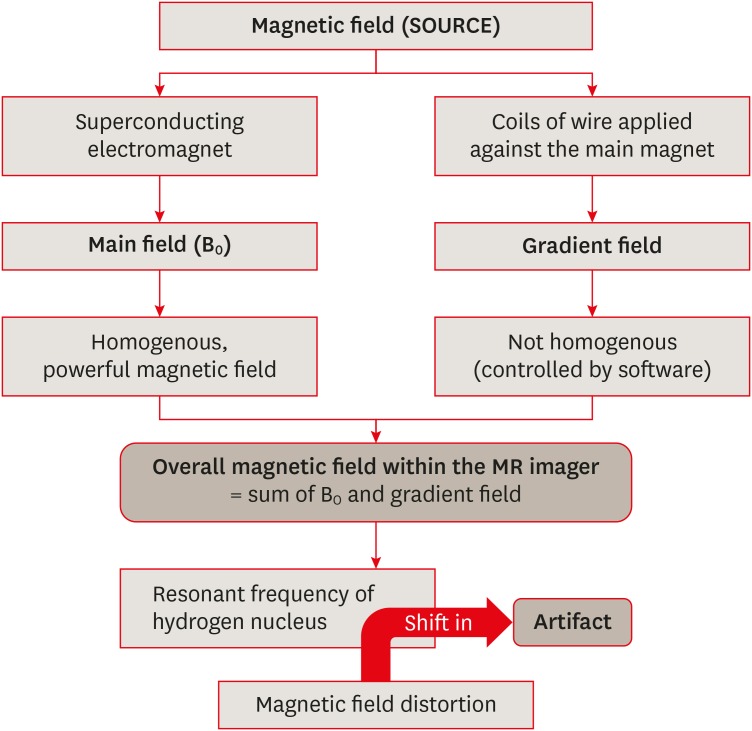
The mechanisms of artifact formation and other interactions can be understood by reviewing the principles of MRI (Figure 1). MR is based on the dependence of the resonant frequency of a hydrogen (H) nucleus on the strength of the magnetic field to which the nucleus is exposed. Any distortion of the magnetic field, either by intrinsic or extrinsic effects, will therefore result in spatial distortion of the image; that is, the distortion of the magnetic field at a certain point shifts the resonant frequency of the H nuclei at that point [6]. Figure 1 summarizes the mechanism of MRI and artifact formation. In the case of dental materials, there are 2 potential sources of artifacts in MRI.
1) Distortion of the static magnetic field (B0) due to differences in the magnetic susceptibility of materials and body tissues
A susceptibility artifact (SA) is defined as signal incoherence generated by the intermingling of substances with discrepant capacities to be magnetized (measured by x, susceptibility). Because most body tissues are diamagnetic (not very magnetizable), proximity to substances with highly magnetic properties (i.e., ferromagnetic materials) induces SAs.
2. Unwanted mechanical (magnetically-induced displacement) effects
The term ‘MR environment’ encompasses the static, gradient, and radiofrequency electromagnetic fields that may affect implants and other devices in the body. The most immediate risk associated with the MR environment is the attraction between the MRI device (a magnet) and ferromagnetic metal objects [173637]. The magnetic field is strong enough to pull heavy objects towards the scanner at a very high velocity (known as the projectile effect) [38]. The translational attraction (dependent on magnetic field strength and the object's mass, shape, and magnetic susceptibility) and resultant torque may cause the movement or dislodgment of ferromagnetic implants, resulting in uncomfortable sensation or injury to the patient [223940].
According to testing standards (ASTM F2052-06) of magnetically-induced deflection, if the device under testing is deflected by < 45°, the risk induced by this deflection force is no greater than that imposed by normal daily activity in the earth's gravitational field [41]. Hasegawa et al. [22] found that the deflection angles were > 90° with deflection forces of 0.03–0.3 N for magnetic dental attachments with castable alloys (components of removable partial denture prostheses) during 3 T MRI. The authors concluded that magnetic dental attachments may cause patient discomfort, but the retention force of dental luting cement (48–150 N) is strong enough to prevent prosthesis dislodgment. Nevertheless, the fixation of the ferromagnetic prosthesis to the tooth must be checked before and after MRI, due to the possibility of cement degradation [40].
Patients in which MRI poses a high risk include those with biomedical devices and implants such as pacemakers, cochlear implants, neurostimulators, infusion pumps, fixed metal prostheses, and aneurysm clips. MRI is contraindicated in such patients because the magnetic field of MRI can cause these devices to become non-functional, thus generating life-threatening situations, dislocation (due to torsion), and soft tissue burns (due to the absorption of radiofrequency energy) [327384243].
3. Unwanted physical effects (radiofrequency heating)
Due to interactions with MRI, metallic objects in the human body can undergo radiofrequency-induced heating [17]. The heat-pain threshold for the oral mucosa is a temperature rise of 8°C–10°C. A temperature increase above 10°C for more than 1 minute constitutes the safety threshold for the periodontal ligament, which is a highly vascular tissue compared to bone [2240]. The aforementioned study by Hasegawa et al. [22] assessed the increase in the temperature of magnetic dental attachments with castable alloys (components of removable partial denture prostheses). Using 3 T MRI, the maximum elevation in temperature was 1.42°C. This temperature increase was not high enough to cause pain or damage to periodontal tissues.
Factors influencing unwanted effects
1. Magnetic susceptibility and magnetic permeability
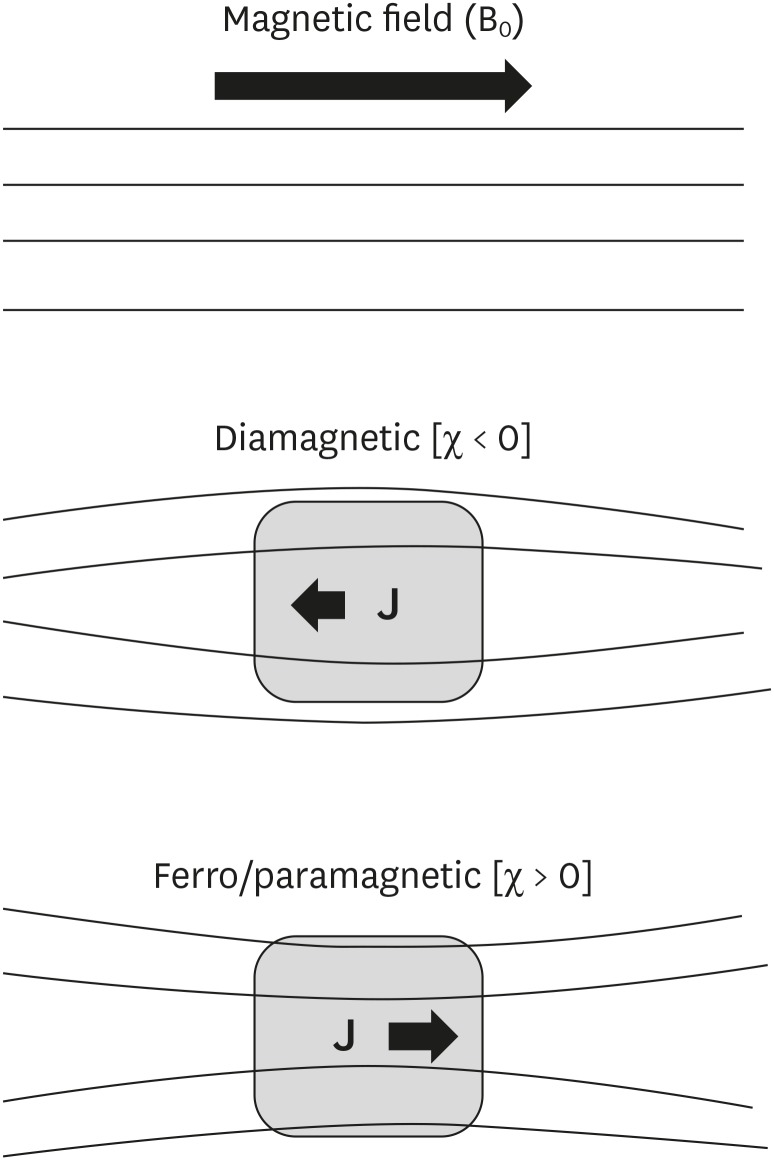
During MRI, when no matter is present (i.e., in a vacuum), the induced field (B) and applied field (H) are essentially equivalent. Whenever matter is present within a given region of space, the induced field (B) is generally not equal to the applied field (H) because various electromagnetic interactions (internal magnetization [Mi] or polarization [J]) occur that concentrate or disperse the magnetic lines of force. This magnetization is proportional to the applied field by a dimensionless constant known as magnetic susceptibility (χ), which is synonymous with magnetizability. It is a measure of the extent to which a substance becomes magnetized when it is placed in an external magnetic field. Another dimensionless factor is magnetic permeability, a physical constant. It is related to magnetic susceptibility by the expression: µ = 1 + χ.
With regard to magnetic effects, 3 classes of materials exist (Table 2; Figure 2). Nearly all biological tissues are weakly diamagnetic. Other than trace amounts of magnetite, there are no endogenous ferromagnetic substances in the human body. However, many extrinsic metallic foreign bodies and surgical implants commonly encountered in MR imaging are ferromagnetic [82734444546].
Classification of materials according to their interactions with magnetic fields.
χ, magnetic susceptibility (synonym = magnetizability); J, Polarization or Internal magnetization.
The greater the magnetic permeability of a material, the more magnetic field distortion (size of the resultant artifact) it will produce [627]. Thus, alloy composition is important in creating artifacts on MRI. Other important factors include the size and shape of the metallic material, as well as its position in the body [34]. MRI without artifacts is possible, even in close proximity to dental materials (such as amalgam, precious metal alloys, and titanium), provided that they have a low magnetic susceptibility. Unfortunately, not all current dental materials meet this criterion of low magnetic susceptibility [ 34]. Schenck [45] described the role of magnetic susceptibility of a material in MRI. Tymofiyeva et al. [8] analyzed and classified dental materials into 3 categories according to differences in susceptibility, as shown in Table 3.
2. Electrical conductivity of the dental material
The magnetic field in MRI can also be distorted by electric currents flowing in materials within or close to the machine. Currents are induced in materials (especially in good conductors) by fluctuating magnetic fields [8]. The main magnetic field (Bo) is time-invariant, but gradient magnetic fields induce an electric current in any conductor in the field regardless of its magnetic properties. These induced currents, called ‘eddy currents’, themselves generate a magnetic field and cause spatial distortion of the image. The magnitude of the eddy current is determined by the rate of change of the magnetic field and the electrical resistance and configuration of the material [8].
3. Mechanical history (tensile strength) of the dental material
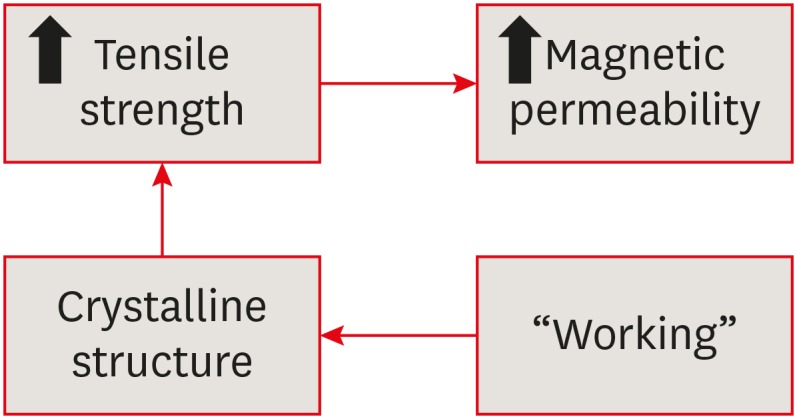
Although materials with sufficiently high nickel content (> 10%) show low magnetic permeability, those with lower nickel content show no correlation between composition and magnetic permeability. This lack of correlation is explained by the association between magnetic permeability and tensile strength [646]. As tensile strength increases, so does magnetic permeability. Tensile strength depends on the crystalline structure of the metal, and may be changed by ‘working’, or the extent to which the metal has been formed, bent, twisted, or cut by cold, which has a major effect on its crystalline structure. Hence, the past mechanical history of stainless steel alloys determines their effect on the images (Figure 3) [6].
4. Imaging sequence used for MRI
In a study done by Bartels et al. [47], paramagnetic substances in vascular stents caused artifacts on MRI. The authors explained that the artifacts that were generated depended on the MRI sequence used and material size and thickness. Some sequences are more sensitive to SAs (Table 4) [34]. However, in the sequence protocol adopted by Costa et al. [27], a short echo time was not sufficient to reduce SAs.
Recommended guidelines
According to a literature review and the available evidence (Table 5), the following conclusions can be drawn regarding the use, safety, and diagnostic value of MRI in the presence of various dental materials and devices.

Summary of unwanted effects due to interactions of dental materials with MRI, according to a literature search (1988–2018)
1. Orthodontic materials: the issue of artifacts
In fixed orthodontic treatment, NiTi and stainless steel arch wires are used with stainless steel brackets (austenitic stainless steel: 18% Cr; 8% Ni) [20]. Since nickel and chromium are ferromagnetic metals, they distort local magnetic fields, causing large artifacts that make image interpretation impossible [27]. Debonding procedures, apart from potentially damaging enamel, are time-consuming, uncomfortable for the patient, and costly [48]. Orthodontists may be asked for recommendations regarding the removal of fixed orthodontic appliances for MRI scans of the head and neck region, and the following guidelines may be useful in that context:
When firmly bonded and carefully ligated, fixed orthodontic appliances are safe for use in MRI scanners. Steel retainer bonds should be checked prior to the scan to ensure their attachment.
Leaving a non-ferromagnetic wire in place keeps the brackets together even if the enamel bond fails.
If the dento-alveolar region is to be studied, the plane of the scan should be altered to avoid the site of metal devices. If not feasible, the orthodontic brackets and wires should be removed [721].
Artifacts may not always interfere with the diagnosis, especially when they are present in areas that are not of interest (Table 6) [22].
2. Orthodontic materials: issues regarding physical and mechanical effects
Due to interactions with MRI, metallic objects in the human body can undergo radiofrequency-induced heating. A study by Gorgulu et al. [20] found that the radiofrequency-induced heating of NiTi arch wires and continuous stainless steel ligature wires was statistically significant (3.04°C), but this was not the case for stainless steel arch wires combined with elastic or continuous stainless steel ligatures (≤ 2.12°C). Although this temperature increase was regarded as insufficient to cause pain or damage to periodontal tissues (heat-pain threshold = 8°C–10°C), the authors stated that it would be safer to replace NiTi and stainless steel wires before MRI; however, brackets were considered to be ‘MR safe’ [20].
3. Maxillofacial prostheses
Hasegawa et al. [22] evaluated the behavior of removable partial denture magnetic dental attachments (keeper and copings) in terms of radiofrequency-induced heating and displacement (torque), and arrived at the following conclusions:
Radiofrequency-induced heating of magnetic dental attachments during 3 T MRI should not pose a risk to patients.
Since the magnetically-induced torque was within the acceptable limits, but the deflection forces exceeded those limits, ferromagnetic devices should ideally be removed from the oral area before MRI. Since this may not always be possible, for safety purposes, the fixation (cement degradation) of such devices should be inspected before and after MRI [22].
4. Dental implants
Dental implants are made of non-ferromagnetic materials (titanium) and contain traces of ferromagnetic iron, which causes a drop-out of signal near the metallic surface [2746]. Costa et al. [27] found that titanium implants caused artifacts in all planes, resulting in severe blooming that led to issues in diagnosis, but less so than orthodontic appliances [49]. Other authors reported that titanium caused only minor artifacts and allowed good visualization [650]. Devge et al. [44] also found that artifacts caused by implants were minor and did not jeopardize scan evaluation. However, magnet keepers attached to implants caused major artifacts, so they are recommended to be removed before an implant patient is referred for an MRI examination.
5. Direct restorative materials
1) Glass-ionomer cements (GIC)
GIC restorations produce no detectable distortions on MR imaging. They are classified as compatible with MRI (the material produces no detectable distortions; Δx < 3 ppm, Table 3) [8].
2) Composite resin
Tymofiyeva et al. [8] found that the composite resins of some manufacturers were compatible on MRI, whereas other brands were compatible I (the material produces noticeable distortions, with the acceptability depending on the application; 3 < Δx < 200 ppm) (Table 3). Ingredients such as ytterbium trifluoride, ferric oxide, and lanthanum oxide (coloring agents) cause image disturbances in MRI because they are ferromagnetic.
3) Amalgam
Amalgam is composed of several metals (silver, tin, copper, zinc, platinum, palladium, and mercury), with silver being the major component [79]. Dental amalgam alloy has little influence in dental MRI because silver is a diamagnetic (non-ferromagnetic) metal [49]. However, MRI is not completely devoid of any effects on amalgam restorations. Shahidi et al. [80] found a statistically significant increase in microleakage when teeth restored with amalgam were exposed to MRI.
Interestingly, during the setting reaction with mercury, diamagnetic silver becomes paramagnetic [8182]. Yilmaz et al. [3] studied the effects of a 3 T magnetic field on amalgam restoration materials with different ratios of silver content (40%, 50%, and 70%), and found no significant differences in microleakage between the amalgam types (non-gamma-2 spherical amalgam versus non-gamma-2 admixed amalgam).
6. Indirect restorative materials
1) Gold crowns
The metals commonly used to manufacture crowns are gold, palladium, nickel, and chromium [79]. Although gold is a diamagnetic substance, gold alloys contain traces of other ferromagnetic metals [27]. According to Eggers et al. [29], even small amounts of a ferromagnetic substance can cause an extensive blank in the image. This compositional difference accounts for discrepancies in study results regarding artifact formation with gold crowns. Abbaszadeh et al. [25] found significant image distortion in MRI; whereas Costa et al. [27] found that gold crowns generated little image distortion, visible only in the sagittal plane.
It has been speculated that the only reason why dental gold might produce distortion may be because it supports large eddy currents caused by its high electrical conductivity [6]. Camacho et al. [35] investigated MRI artifacts caused by radiofrequency eddy currents and found substantial artifacts. However, Fache et al. [6] found that the impact of eddy currents was negligible, as a piece of dental gold studied in vitro, and extensive gold restorations in the mouth of a volunteer revealed no distortions on the MRI scanner.
Tymofiyeva et al. [8] classified gold alloy and gold-ceramic crowns as compatible I, with the acceptability depending on the application (Table 3).
2) Ceramic and metal-ceramic crowns
Tymofiyeva et al. [8] classified gold-ceramic crowns as compatible I (Table 3). Precious metal alloys, nickel-chromium alloy, and cobalt-chromium ceramic alloy used as metal copings for dental porcelain display MRI artifacts. The artifact area increases with the strength of the magnetic field.
Cortes et al. [58] analyzed the impact of nickel-chromium metal-ceramic restorations (i.e., dental crowns and fixed bridges) and found a significant correlation between echo time and artifact area in gradient echo pulse sequence images. They suggested that it is possible to compensate for the effect of higher field strength on MRI artifacts by setting optimized pulse sequences for scanning patients with metal-ceramic restorations [59].
Xu et al. [57] found that zirconia and casting ceramics presented almost no or faint artifacts. In contrast, the study by Klinke et al. [46] found that ceramic (zirconium dioxide) led to the same effect as metal-based materials on MRI of the lower mid-face. Wedge-shaped specimens (1 – 3.5 × 9 × 16 mm) of the ceramic materials IPS Empress and Ducera gold showed artifacts less than 15 mm, while Cergo and Vita Omega 900 showed artifacts between 15 and 30 mm, and zirconium dioxide showed artifacts larger than 30 mm (the same as metal alloys).
7. Endodontic materials
Endodontic materials such as resin-based sealer (AH Plus) and gutta-percha produce no detectable distortions on MRI. They are classified as compatible with MRI (Table 3). No data are available on silver cones, or separated NiTi and stainless steel instruments used in root canal therapy [8].
CONCLUSIONS
As MRI is becoming widely used in dentistry, it is critical that dental practitioners are aware of the potential of dental materials to cause adverse interactions during MRI. Dental practitioners must be acquainted with the composition of orthodontic devices, maxillofacial prostheses, implants, direct and indirect restorative materials, and endodontic materials, in order to anticipate complications and take precautions prior to MRI in patients with the aforementioned dental materials.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
Author Contributions:
Conceptualization: Deepak BS.
Data curation: Chockattu SJ.
Formal analysis: Chockattu SJ.
Investigation: Chockattu SJ.
Methodology: Chockattu SJ.
Project administration:
Resources: Chockattu SJ.
Software: Chockattu SJ.
Supervision: Thakur S.
Validation: Thakur S.
Writing - original draft: Chockattu SJ.
Writing - review & editing: Deepak BS.