Influence of post types and sizes on fracture resistance in the immature tooth model
Article information
Abstract
The purpose of this study was to determine the effect of post types and sizes on fracture resistance in immature tooth model with various restorative techniques. Bovine incisors were sectioned 8 mm above and 12 mm below the cementoenamel junction to simulate immature tooth model. To compare various post-and-core restorations, canals were restored with gutta-percha and resin core, or reinforced dentin wall with dual-cured resin composite, followed by placement of D.T. LIGHT-POST, ParaPost XT, and various sizes of EverStick Post individually. All of specimens were stored in the distilled water for 72 hours and underwent 6,000 thermal cycles. After simulation of periodontal ligament structure with polyether impression material, compressive load was applied at 45 degrees to the long axis of the specimen until fracture was occurred.
Experimental groups reinforced with post and composite resin were shown significantly higher fracture strength than gutta-percha group without post placement (p < 0.05). Most specimens fractured limited to cervical third of roots. Post types did not influence on fracture resistance and fracture level significantly when cement space was filled with dual-cured resin composite. In addition, no statistically significant differences were seen between customized and standardized glass fiber posts, which cement spaces were filled with resin cement or composite resin individually. Therefore, root reinforcement procedures as above in immature teeth improved fracture resistance regardless of post types and sizes.
I. Introduction
When pulp necrosis of immature tooth is developed, tooth development would not continue any longer, and thickness of root dentin wall remains thin for the discontinuation of tooth development. Peritubular dentin appears higher mineral deposition in mature dentin than developing dentin.1) In addition, it is reported that 180-day of calcium hydroxide dressing decrease 10 to 20% reduction of fracture strength and increase the likelihood fracture of teeth.2) A study by Cvek3) pointed out that endodontically treated immature tooth is prone to fracture, especially at the cervical third. Therefore, there is a need to reinforce root structures after apexification procedure of immature tooth.
To date, various techniques for root strengthening of immature tooth have been introduced, for example, the reinforcement of wall thickness with composite resin or mineral trioxide aggregates (MTA) and post placement. It has been demonstrated that the increase in wall thickness of weakened tooth model using composite resins increased resistance to fracture.4) Also, it is documented that zirconium fiber post or composite resin can increase significantly the structural resistance in weakened teeth.5) In addition, twice fracture resistance was obtained compared with that of an apical MTA and filling with guttapercha and sealer.6) Recently, a clinical approach has been introduced to use titanium post and MTA for root reinforcement.7)
Ideal materials for root reinforcement should bond to root dentin and have a similar elastic modulus with root dentin.8) MTA lacks of bonding to dentin and has low strength in tension. Also, MTA is not clinically appropriate for root reinforcement because of difficulty in manipulation, longer setting time, and possibility of tooth discoloration. In comparison, dual-cured resin composite can bond to dentin with adhesive systems, polymerize chemically without a light source, and has a superior strength and elastically compatible with dentin. Therefore, Dual-cured resin composite can reinforce weakened root structure in immature teeth. Dual-cured resin composite, however, undergoes polymerization shrinkage more at the site of high C-factor like root canal. Also, although dual-cured composite can be polymerized chemically, its degree of conversion is mostly dependent on light curing.
Metal posts have higher elastic modulus than dentin by five times or more, and its stiffness can prevent post-and-core structures from deformation. However, the appreciable difference in elastic modulus with surrounding structure can lead to root fracture. Among them, as titanium posts have elastic modulus closer to dentin, its application is promising. A few cases were reported to use titanium posts clinically in immature teeth.7)
Fiber posts have similar elastic modulus with dentin and can bond with resin cement through surface treatment and bonding procedure. In addition, fiber posts can transmit light to deeper part of the canal so they can improve degree of polymerization of resin cements.9) Previous studies of fiber posts reported that fiber posts tend to result favorable fracture pattern compared with metal posts, because metal posts concentrate stress on surrounding dentin at the level of apical end of metal posts, rather than redistributed along the post surface as in fiber posts. It can be said that fiber posts with resin cement, therefore, are the most appropriate for root strengthening procedure clinically.
It is difficult to place post closely fitted in the flared canal of immature tooth because most post systems are standardized in size, so an increase in cement thickness is inevitable. Generally, mechanical and bonding properties are compromised when the film thickness is too great.10) To attain uniform cement thickness, two types of post can be considered as a candidate; cast post and recently released EverStick® Post. Experimental studies of cast post revealed that cast post demonstrated high incidence of catastrophic root fracture on fracture strength testing. Because of a marked difference in modulus of elasticity between cast post and dentin, however, it cannot reinforce root structure particularly in the case of thin-walled immature tooth11). EverStick® Post has comparable elastic modulus with dentin and can be customized in size by bonding to each other to adapt a large flared canal. Accordingly, EverStick® Post can be used to reinforce immature root with resin cements.
Previous studies demonstrated that root reinforcement with composite resin in immature tooth improves fracture resistance5,11). Nevertheless, comparative studies of fiber post and titanium post in flared large canal reinforced with composite resin has not been published. Furthermore, the use of resin composite for root strengthening has not been proved to be effective over post in customized size. Therefore, the purpose of this study was to determine the effect of post types and sizes on fracture resistance with or without resin reinforcement. Fracture strength of immature bovine incisors were compared between various restorative techniquesgutta percha, fiber post, titanium post and customized fiber post (EverStick® Post), also with dual-cured composite resin and resin cement after in vitro aging procedure.
II. Materials & Methods
1. Specimen Preparation
One hundred forty-three bovine incisors were extracted and sectioned 8 mm above and 12 mm below the cementoenamel junction, total length of 20 mm using the water-cooled diamond points6) (Figure 1). Tooth specimens were excluded which had cracks or defects on surfaces. Apical root shape, buccolingual or mesiodistal diameter, and remaining dentin thickness were measured using a digital caliper (Figure 2). Specimens of the size confined to limited range were selected, total 57 specimens were used in this experiment.
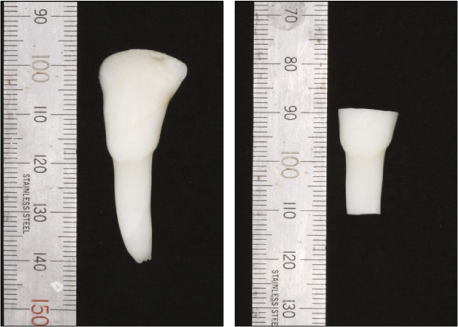
Model of immature permanent incisor.
Sectioned part of bovine tooth; the crown had a length of 8 mm from the cementoenamel junction, the root was 12 mm in length from the cementoenamel junction.
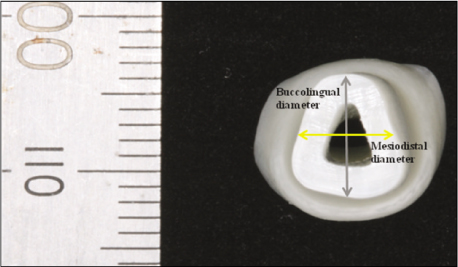
The width of remaining root dentin and the size of the specimen is measured with the electronic digital caliper.
Access cavities were prepared and pulps were extirpated, any debris in the canals were removed with minimal instrumentation. Canals were irrigated copiously with 5.25% sodium hypochlorite and 18% EDTA and finally dried.12) Portland cements were filled 4-mm-thick in apical area using sterile paper-points and endodontic condensors. Filling qualities were evaluated with pariapical radiographs and any specimens which were recognized gaps or voids were corrected with ultrasonic filling technique. Portland cements were mixed with a ratio of 3 to 1, powder to liquid, allowed to set and stored more than four hours in 100% humidity.
Control group: After drying root canals with paper-points, canals were filled with gutta percha and AH 26® (Dentsply DeTrey®) sealer using thermoplastic injection technique (Duo-beta, B&L Biotech.) 2 mm below the buccal cementoenamel junction. Access cavities were filled with Cavit™ G (3M ESPE) for temporary sealing, and specimens were stored in distilled water for 24 hours. After temporary sealing material was removed, semi-gel type of 37% phosphoric acid was used to etch endodontic cavity for 15 seconds. The canal was washed and left in slightly moistened state, two coats of ONE-STEP® (Bisco Inc.) were applied with microbrushes and gently dried. The adhesive was polymerized with light curing for 20 seconds, and dual-cured resin core material, LuxaCore® Smartmix Dual (DMG) was injected, light-cured for 40 seconds.
Group 1: D.T. LIGHT-POST® (Bisco Inc.) #3 was cut with a diamond bur to 14 mm in length, ONE-STEP® was applied on the post surface, gently dried and light cured for 10 seconds as manufacturer's instruction. The canal was rinsed, coated with ONE-STEP® as control group and the space between the post and the canal was filled with LuxaCore® Smartmix Dual. LuxaCore® Smartmix Dual was injected through two times, the first layer was light-cured for 10 seconds, and finally for 40 seconds.
Group 2: A serrated paralled titanium post, ParaPost® XT™ (Coletène/Whaledent Inc.) #6 was prepared for 14 mm in length and tribochemical silica coating and silanization with Monobond-S (Ivoclar Vivadent) on the post surface were followed.13) The post surface was dried with oil-free air syringe after 60 seconds, two coats of ONE-STEP® were applied and gently dried, polymerized with light curing for 10 seconds. The same procedures were followed as group 1.
Group 3: EverStick® Post (StickTech) 0.9 was prepared for 14 mm in length and light-cured for 40 seconds. After removal of the post, Adper™ Scotchbond™ Multi-Purpose Adhesive (3M ESPE), an enamel bonding agent, was applied for activation of post surface and left for 3 to 5 minutes under a light shield to prevent from premature curing, as manufacturer's recommendations, followed by light polymerization for 10 seconds. The same procedures were followed as group 1.
Group 4: EverStick® Post 1.5 was prepared for 14 mm in length, and light-cured for 20 seconds inside the canal. Additional posts were bonded and shaped to the main post according to the root canal with a thin layer of Adper™ Scotchbond™ Multi-Purpose Adhesive, and then light-cured for 10 seconds inside the canal. The post surface was treated as group 3. The canal was etched for 15 seconds with 37% phosphoric acid, ONE-STEP® was applied twice, gently dried and light-cured for 10 seconds. A dual-cured resin cement, Variolink® II (Ivoclar Vivadent) was applied in the canal with lentulo spiral, and the post was placed, polymerized with light curing for 40 seconds.
Periapical radiographs were taken to assess the quality of root canal restoration and specimens with voids were excluded in this study. All of specimens were stored in the distilled water for 72 hours (Figure 3).
2. Fracture Strength Testing
All specimens underwent 6,000 thermal cycles between 5℃ and 55℃, with a dwell time of 30 seconds and a transfer time of 5 seconds.14) Afterwards, specimens were preserved in 100% humidity for a week. 0.2 mm-thick blue sheet waxes were pressure-welded on root portion of specimens uniformly. They were mounted in the prefabricated acetal blocks, and embedded in acrylic resin up to 2 mm from the buccal cementoenamel junction. After setting of injected acrylic resin, specimens were pulled out of the block and waxes were removed from the surfaces. The 0.2 mm-gaps were filled with polyether impression material, Impregum™ F (3M ESPE) for periodontal ligament simulation (Figure 4). Any excesses were carefully removed with blades after setting of polyether.15)
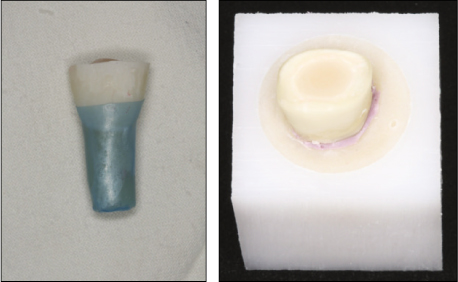
0.2 mm-thick sheet wax is pressure welded on the root surface. The specimen is placed in the acetal mold, and autopolymerizing acrylic resin is injected into the mold.
Specimens individually were tested fracture strength using Universal Testing Machine Instron (INSTRON Corporate Headquarters) at a constant speed of 0.5 mm/min. Compressive load was applied at 45 degrees to the long axis of the specimen, at the point of lingual incisal edge (Figure 5). The loads at fracture were recorded, at the point that stress was abruptly reduced. Fractured specimens were analyzed a direction and location of line of fracture, and they were classified into restorable and non-restorable fracture. Cervical fracture restricted within coronal third of the root was recorded as restorable fracture, and vertical or horizontal fracture extended into middle and apical third of the root as non-restorable fracture.
3. Statistical Analysis
Kruskal-Wallis ANOVA on Ranks was performed to determine significant differences between groups. Post hoc multiple comparison was applied using Bonferroni/Dunn test when data analysis showed significant difference, with a significance level of p < 0.05.
III. Results
Specimens were selected for similar size, and mean root diameters in buccolingual and mesiodistal direction were 7.41 mm (S.D. 0.47 mm) and 5.98 mm (S.D. 0.49 mm) respectively. Remaining dentin thickness of all specimens ranged between 2.0 ± 0.2 mm. Twelve specimens with gaps in cement layer in periapical radiographs were excluded, and total forty-five specimens were submitted to fracture strength test.
Median fracture strengths of the groups are shown in Table 1. Specimens of all experimental groups demonstrated significantly higher load at fracture than control group (p < 0.05), and group 4 showed slightly higher fracture strength compared with group 1, 2 and 3, but the difference was not statistically significant (Figure 6). The result of fracture analysis is also shown in Table 1. No significant differences in the incidence of restorable and non-restorable fracture were found between groups (Figure 7, 8). Location of fractures in control group was detected at the margin of core. All specimens of control and experimental groups fractured extended below the cementoenamel junction, not limited to crown portion.
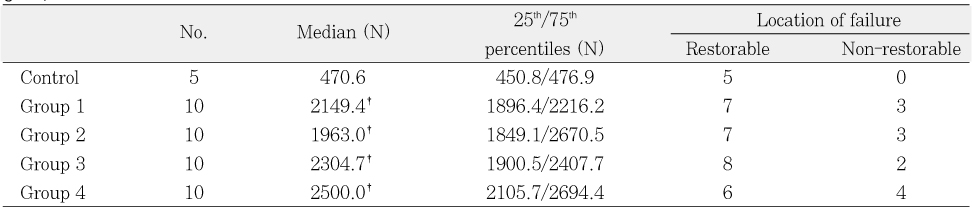
Median fracture strength (25th and 75th percentiles) and location of failure of control and experimental groups
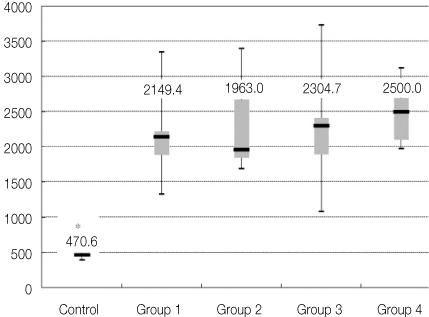
Box plots of fracture load (median, 25th and 75th percentiles) of the control and experimental groups (N).
IV. Discussion
Necrotic immature teeth require restorative procedure for root reinforcement due to discontinuation of root development. Thin root dentin and calcium hydroxide treatment reduce fracture resistance of immature teeth, although loss of coronal structure is minimal. Generally posts are used for the purpose of increasing retention of core and crown structures, not of root strengthening. In the case of endodontically treated immature teeth, however, posts can be used for root reinforcement.5,11,16,17) This study is designated for the determination of root reinforcement effect of posts, and for comparison of fracture resistance with combination of various post and cement systems.
Bovine teeth differ from human teeth morphologically. In addition, it is reported that bovine teeth are more susceptible to thermal fatigue and crack propagation after thermocycling than human teeth.18) However, ultimate tensile strength and elastic modulus of bovine teeth are not significantly different from those of human teeth,19) and bovine teeth facilitate to ensure large number of immature incisors of similar sizes. Immature permanent teeth have open and even divergent apical morphology, thin and weakened root dentin wall because of arrested tooth development. Therefore, bovine teeth were used in this study to model immature permanent tooth by the amputation of apical root portion.
Median fracture strength of bovine teeth restored with gutta percha over MTA apical plug in bovine teeth was 470.6 N in this study, and this value is relatively low compared with previously published studies of Carvalho and Bortoluzzi, 767 N and 872 N respectively.5,6) That is because thermocycling was not performed in the above studies and thermocycling may reduce fracture resistance of bovine teeth due to thermal fatigue.
MTA has superior biocompatibility, sealing ability and high strength although it has lack of bonding ability to dentin. Therefore, it has been widely used in apexification procedure of immature permanent teeth. 4-mm-thick MTA is recommended for prevention of apical leakage.20,21) Portland cement and MTA are similar in chemical compositions, sealing ability and solubility.22) Also, the compressive elastic modulus of Portland cement is up to that of dentin.8) Therefore, MTA can be replaced with Portland cement in experimental study. In this study, accordingly, 4-mm-thick portland cement was used as a substitute for MTA apical plug.
It was reported that a simulation of periodontal ligaments influences on fracture level. The teeth with periodontal ligament simulation tended to fracture at root level, while the teeth without periodontal simulation tended to fracture on top of resin blocks.15) That is because periodontal ligament transfers the load to the alveolar bone and the stress is redistributed in all root surfaces. Polyether, elastomeric impression material, can reproduce periodontal ligaments suitably based on its deformation limit, value and high ultimate tensile strength. On the analysis of fracture pattern in this study, fracture levels of all specimens are beyond the cementoenamel junction.
Bonding ability and elastic modulus similar to dentin are basic requirements of restorative materials for root strengthening,8) and composite resin is a corresponding material. Large flared root canals in immature teeth have the advantages of accessibility and C-factor for composite resin filling. In addition, dual-cured resin composites can be polymerized deep in the canal where light transmission is limited. However, canal obturation with dual-cured resin composite results in reduced mechanical properties because a large portion of dual-cured resin composite is dependent on light curing. For these reasons, resin reinforcement of root canal without post has not been attempted. In this experiment, light-curing time was increased and dual-cured resin composite was injected through two times, each layer was light-cured individually for improved polymerization.
Elastic modulus of materials within the canal for root reinforcement is an important factor for fracture resistance of weakened roots. The more rigid component in the canal can resist greater forces without distortion but it induces stresses within the canal. In contrast, a material with low elastic modulus of the material cannot prevent from distortion but it acts as a shock absorber increasing tooth strength. It means that resistance for distortion and stress distribution are dependent on elastic modulus of materials within the canal (Table 2).8,23,24)
The effect of elastic modulus of posts on fracture strength was evaluated from glass fiber posts and titanium posts. D.T. LIGHT-POST® is composed of unidirectional quartz-fiber post system with double tapers. It can transmit light along the post to improve degree of conversion of resin cements deep in the canal,9) and elastic modulus of the post is similar to dentin. ParaPost® XT™ is titanium post system and elastic modulus is about 60 GPa25), which the value is closer to that of dentin than stainless steel.8) It has threaded surface for mechanical retention, and the gap between post and canal was filled with composite resin in the experiment. This study revealed that fracture strengths of specimens restored with D.T. LIGHT-POST® and ParaPost® XT™ were not significantly different. In addition, the incidence of restorable and non-restorable fracture was not significantly different between post types. Many previous studies have reported that titanium post presents higher fracture resistance than fiber post and higher incidence of catastrophic fracture.26-29) It is known that maximum load capability is affected less by post strength, but more by the amount of surrounding hard tissue.17) These specimens are of sufficient tooth structures and height of coronal dentin as well as resin-reinforced dentin wall. For this reason, higher modulus of elasticity of titanium post does not increase fracture strength and the incidence of oblique root fracture. Therefore, both fiber posts and titanium posts improve fracture resistance and tend to induce favorable fractures in immature tooth model.
EverStick® Post consists of unidirectional E-glass and unpolymerized Bis-GMA matrix, and it has elastic modulus similar to dentin.30) An enamel bonding agent without solvent like acetone can penetrate into and partly solve unpolymerized resin matrix monomers, allowing to bond with resin cements.31,32) In addition, EverStick® Post can be bonded each other and trimmed for adaptation to root canal. It is intended to compare fracture strength according to width of cement space with customized and standardized EverStick® Posts. Customized EverStick® Posts tended to show slightly higher fracture strength than standardized EverStick® Posts, but the values were not statistically different. Several studies10,33) reported that retentive strength of posts are reduced as cement thickness increases, by reason that increased cement space may result in procedural errors, decreased integrity of cements, and these structural flaws can compromise mechanical properties of restorations. Root canals of immature teeth, however, are reinforced with high-strength dual-cured composite resin instead of resin cement in this study. Accordingly, a customized fiber post did not demonstrate additional advantages in spite of its labored procedure.
Immature teeth with sufficient crown structures were used in this study and this may contribute to high fracture strength independent of post types. The amount of remaining tooth structures are known to much influence on fracture strength of teeth restored with post and core.34,35) However, post groups showed significantly increased fracture strength compared with control group restored with gutta-percha and resin core. Therefore, it is recommended post placement for root strengthening in immature teeth. Further studies are needed to evaluate the effect of post types on fracture resistance of immature teeth in a model of severe loss of crown structures.
V. Conclusions
This study evaluated the effect of post on root strengthening and fracture resistance according to post types and post fitness in a model of immature bovine incisors. Experimental groups were designed to use fiber posts and titanium posts. Also, the effect of post fitness was compared using standardized and customized fiber posts. Within the limitation of this in vitro study, the following conclusions can be drawn:
In a model of immature bovine incisors, experimental groups reinforced with post and composite resin were shown significantly higher fracture strength than control group without intra-radicular reinforcement technique (p < 0.05).
Post types did not influence on fracture resistance significantly when cement space was filled with dual-cured resin composite.
No statistically significant differences were seen between customized and standardized glass fiber posts, which cement spaces were filled with resin cement or composite resin individually.
Notes
This work was supported by a 2008 research grant from College of Dentistry, Yonsei University.




