Push-out bond strength and intratubular biomineralization of a hydraulic root-end filling material premixed with dimethyl sulfoxide as a vehicle
Article information
Abstract
Objectives
This study was designed to evaluate the parameters of bonding performance to root dentin, including push-out bond strength and dentinal tubular biomineralization, of a hydraulic bioceramic root-end filling material premixed with dimethyl sulfoxide (Endocem MTA Premixed) in comparison to a conventional powder-liquid–type cement (ProRoot MTA).
Materials and Methods
The root canal of a single-rooted premolar was filled with either ProRoot MTA or Endocem MTA Premixed (n = 15). A slice of dentin was obtained from each root. Using the sliced specimen, the push-out bond strength was measured, and the failure pattern was observed under a stereomicroscope. The apical segment was divided into halves; the split surface was observed under a scanning electron microscope, and intratubular biomineralization was examined by observing the precipitates formed in the dentinal tubule. Then, the chemical characteristics of the precipitates were evaluated with energy-dispersive X-ray spectroscopic (EDS) analysis. The data were analyzed using the Student’s t-test followed by the Mann-Whitney U test (p < 0.05).
Results
No significant difference was found between the 2 tested groups in push-out bond strength, and cohesive failure was the predominant failure type. In both groups, flake-shaped precipitates were observed along dentinal tubules. The EDS analysis indicated that the mass percentage of calcium and phosphorus in the precipitate was similar to that found in hydroxyapatite.
Conclusions
Regarding bonding to root dentin, Endocem MTA Premixed may have potential for use as an acceptable root-end filling material.
INTRODUCTION
The purpose of a root-end filling is to establish a seal between the root canal space and the periradicular tissues [1]. Hydraulic bioceramic cements have been used successfully in root-end fillings due to their favorable sealing ability [2]. Mineral trioxide aggregate (MTA) (ProRoot MTA, Dentsply, Tulsa, OK, USA) was the first type of hydraulic bioceramic material used for root-end filling. Originally, MTA was formulated from commercial Portland cement, which is mainly composed of calcium silicates, combined with bismuth oxide powder for radiopacity. However, the chemical composition of MTA was changed to improve clinical performance, and many derivatives have been introduced. These types of materials are now called hydraulic bioceramic materials instead of MTA for the appropriateness of nomenclature.
Despite its favorable sealing ability, hydraulic bioceramic material presents less-than-ideal working properties, since the cement resulting from the mixture of powder with liquid is difficult to handle [3]. Various approaches have been attempted to achieve convenience of manipulation and delivery. As a result, a method of mixing the powder with a non-aqueous vehicle to produce an injectable, ready-to-use form was developed. This process results in greater plasticity and higher flow, as well as improved handling characteristics compared to conventional bioceramic materials. However, little information exists regarding the effect of the vehicle on the bonding of the material to dentin. Recently, an injectable hydraulic bioceramic cement premixed with dimethyl sulfoxide (DMSO) was developed (Endocem MTA Premixed, Maruchi, Wonju, Korea). In the present study, we aimed to evaluate the bonding ability to root canal dentin of the DMSO-containing root-end filling material in comparison to a widely used conventional powder-liquid cement (ProRoot MTA). To evaluate the bonding, we investigated push-out bond strength and biomineralization in the dentinal tubules. The null hypothesis was that no significant difference exists between the tested materials.
MATERIALS AND METHODS
Preparation of the specimens
A total of 30 freshly extracted single-rooted mandibular human premolars with oval root canals were obtained after the study was approved by the institutional review board of Kosin University Gospel Hospital, Busan, Korea (KUGH-022-08-033). Teeth presenting dental caries, cracks, and fractures were excluded. After cleansing of visible blood and gross debris, radiographs were taken to ensure a similar buccolingual dimension of the root canals. The teeth were stored in a sodium hypochlorite (NaOCl) solution diluted 1:10 with distilled water until the time of experimental usage.
To obtain standardized root lengths, the roots were sectioned 12 mm from the apex with a diamond bar under water cooling. The root canals were instrumented using a rotary instrument system (ProTaper Next, Sybron Endo, Orange, CA, USA) up to size F3. During instrumentation, the root canals were irrigated with 2 mL of 1% NaOCl using a 27-gauge side-vented needle. The smear layer formed in the root canal wall was removed using 1 mL of 17% ethylenediaminetetraacetic acid for 2 minutes. Finally, the root canals were irrigated with 2 mL of distilled water and dried with paper points.
The root canal specimens were randomly divided into 2 groups (n = 15), which were then treated with different filling materials. In the first group, each root canal was filled with ProRoot MTA. After the powder was mixed with the liquid, the mixture was inserted into an MTA carrier (MAP system, Dentsply-Maillefer, Ballaigues, Switzerland). Then, the material was placed in the root canal and compacted apically with plugger and paper points. In the other group, the root canal was filled with Endocem MTA Premixed. The material was injected into the canal and apically placed using paper points. The filling procedure was performed until the canal was filled up to 3 mm from the orifice. Then, the orifice was restored with a temporary filling material (Caviton, GC, Tokyo, Japan). The specimens were stored in phosphate-buffered saline (PBS; HyClone Laboratories Inc., Logan, UT, USA) for 30 days to facilitate biomineralization.
Push-out bond strength
The specimens were embedded in a chemically cured acrylic resin (Ortho-Jet Acrylic, Lang Dental MFG, Wheeling, IL, USA) in a custom-made mold. The mold was placed perpendicular to the tooth surface. Using a low-speed micro-saw, each embedded tooth specimen was cut into a slice of 2.0 ± 0.2 mm in thickness to obtain a specimen for the push-out bond strength test (Figure 1A). A universal testing machine (Z020, Zwick Roell, Ulm, Germany) was used with a 500-N load cell at a crosshead speed of 0.5 mm/min to apply push-out force in the apico-coronal direction (Figure 1B). The maximum failure load was recorded in newtons (N) and then converted to megapascals (MPa) by applying the following formula:
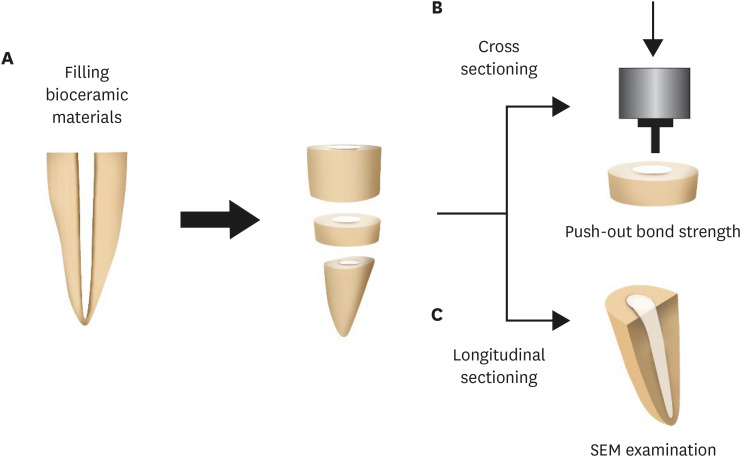
Illustration of the experimental procedure. (A) The tooth filled with the tested materials was sectioned horizontally to obtain a sliced specimen and an apical segment. (B) Push-out bond strength was measured with the sliced specimen using a universal testing machine. (C) The apical segment was sectioned longitudinally, and the intratubular biomineralization was observed under scanning electron microscopy.
SEM, scanning electron microscope.
The adhesion area of the root canal filling was calculated using the following equation:
 ----------(2)
----------(2)where r1 is the smaller radius of the root canal diameter (mm), r2 is the larger radius, h represents the thickness of the root section (mm), and π is the mathematical constant pi, approximated as 3.14.
The sample was observed under a stereomicroscope (MZ16FA, Leica, Wetzlar, Germany) at ×30 magnification to determine the failure mode. Failures were categorized as cohesive (dentin walls totally covered with sealer), adhesive (no sealer visible on dentin walls), or mixed (a combination of cohesive and adhesive failure).
Intratubular biomineralization
The apical segment was cut perpendicular to the long axis of the root with a disc until the cut was 1 mm short of the filling material. Then, the specimen was split in half. The split surface was observed under a scanning electron microscope (SU8230, Hitachi, Tokyo, Japan), and the intratubular biomineralization was examined (Figure 1C). Also, the chemical characteristics of the precipitates formed in the dentinal tubule were evaluated with energy-dispersive X-ray spectroscopic (EDS) analysis.
Statistical analysis
Power analysis was applied with the t-test (effect size = 0.8, power = 0.55) to determine the required sample size using G*Power 3.1 software (University of Düsseldorf, Düsseldorf, Germany). The Shapiro-Wilk test was used to determine normality of the distribution prior to the statistical analysis. Then, the data were analyzed using the Student’s t-test followed by the Mann-Whitney U test using SPSS version 23.0 (IBM Corp., Armonk, NY, USA). A p value < 0.05 was considered indicative of statistical significance.
RESULTS
No significant difference was observed between the 2 tested groups in push-out bond strength (p > 0.05) (Figure 2A). Cohesive failure was predominant in both groups, followed by mixed and adhesive failures (Figures 2B and 3). In both groups, small flake-shaped precipitates were observed along dentinal tubules (Figure 4). As shown by the EDS analysis of the crystal seeds visible in the tubules, the mass percentage of calcium and phosphorus was around 2:1, similar to hydroxyapatite (Figure 5).
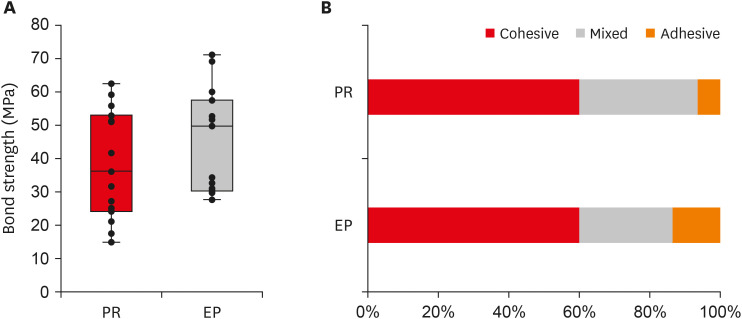
Push-out bond strength and the failure patterns of the tested materials. (A) Bar chart showing the mean bond strength of the 2 tested material groups. (B) Failure mode distribution according to filling material.
PR, ProRoot MTA; EP, Endocem MTA Premixed.
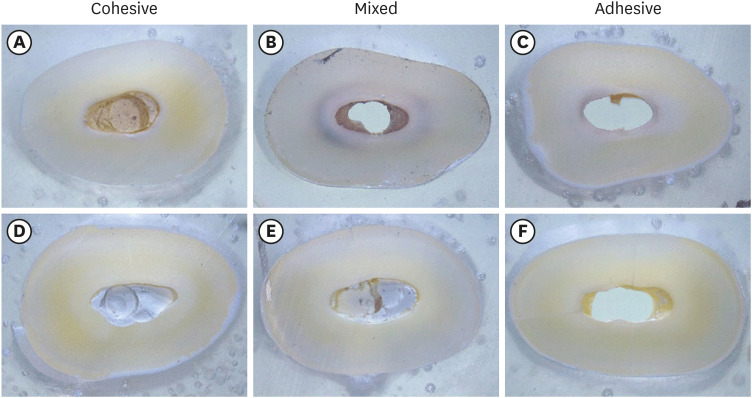
Failure mode analysis using a stereomicroscope at ×30 magnification. (A-C) Representative images of the ProRoot MTA group. (D-F) Representative images of the Endocem MTA Premixed group.
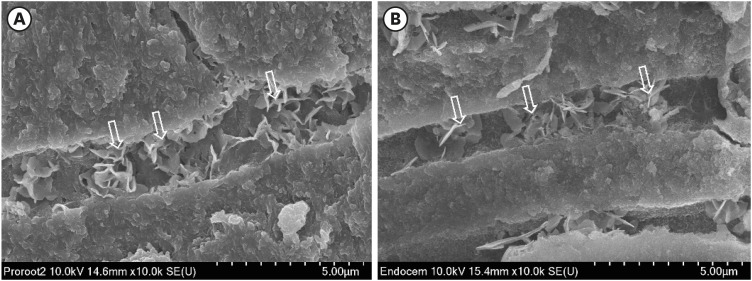
Representative scanning electron microscopy images of intratubular biomineralization. (A) ProRoot MTA-filled root canal. (B) Endocem MTA Premixed-filled root canal. Arrows indicate the flake-shaped intratubular precipitates.
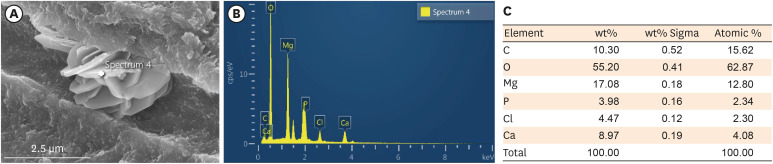
EDS analysis of the chemical characteristics of intratubular precipitate. (A) A scanning electron microscope image showing the precipitate (white cross). (B) Representative graph of EDS analysis of the precipitate. (C) Semiquantitative chemical composition showing the calcium/phosphorus ratio of the crystalline area denoted with a white cross.
EDS, energy-dispersive X-ray spectroscopic.
DISCUSSION
In this study, we investigated the interfacial adaptation of Endocem MTA Premixed, a newly developed premixed hydraulic bioceramic material, to the root canal dentin in comparison to the conventional material ProRoot MTA. Interfacial adaptation to root canal dentin is a principal characteristic of root-end filling material because it is thought to prevent reinfection and entomb any remaining microorganisms in root canals.
First, we measured the push-out bond strength to quantify the interfacial adaptation values of the cements to the root canal dentin. Endocem MTA Premixed was found to have a similar value to ProRoot MTA. Notably, ProRoot MTA has been considered a gold standard for root-end filling and is usually adopted as the control material when interfacial adaptation is evaluated [456]. Furthermore, push-out bond strength is a widely used methodology to evaluate the adaptation of root-end filling material [78]. Therefore, this result suggests that Endocem MTA Premixed is comparable to ProRoot MTA regarding interfacial adaptation and can be considered to show adequate performance in root-end filling.
In the present study, bond failures observed in the 2 experimental groups were predominantly found within the filling material (the cohesive type). In both groups, more than half of the specimens (9 of 15) exhibited cohesive failure. This finding contrasts with several previous studies in which bond failures were usually at the root-end filling material-dentin interface (adhesive or mixed failures) [910111213]. The failure mode may be affected by the thickness of the specimen slice. When the thickness of the slice ranges from 1 to 1.5 mm, adhesive or mixed failures occur, mainly because the mechanical strength of the cement exceeds the bond strength. On the contrary, in this study, the thickness of the slice was 2 mm, and the cohesive failure pattern was predominant over the adhesive type. Similarly, in studies involving 2-mm or thicker specimens, cohesive failure was frequently found [14]. In this respect, the difference in the thickness of root slices between the present study and previous studies may explain the different modes of bond failure. The thickness of the specimen should be considered in failure mode analysis.
The effect of liquid vehicles on the bond strength of hydraulic bioceramic materials is still under debate. Salem Milani et al. [15] reported that mixing with propylene glycol enhanced the strength of bonding of MTA Angelus (Angelus, Londrina, Brazil) to dentin. In contrast, Al-Hiyasat and Yousef [14] reported that a premixed putty-type material (TotalFill FS, FKG Dentaire, La Chaux-de-Fonds, Switzerland) exhibited lower bond strength than Biodentine and ProRoot MTA. Furthermore, Retana-Lobo et al. [16] found that a powder-liquid calcium silicate cement (BioRoot RCS, Septodont, Saint-Maur-des-Fossés, France) presented a higher push-out bond strength than a premixed sealer (EndoSequence BC Sealer, Brasseler, Savannah, GA, USA). The presence of vehicles might interfere with the direct interaction between the cement and the root dentin. Endocem MTA Premixed is also mixed with a non-aqueous vehicle, DMSO, which has been demonstrated to improve the adhesive bonding to coronal dentin and to decrease leakage by increasing dentin wettability [1718]. Interestingly, Lindblad et al. [19] recently reported that final irrigation with DMSO resulted in a significantly higher push-out strength of hydraulic calcium silicate cement. Also, in the DMSO irrigation group, the cohesive failure mode was more common than in the control group. In the present study, Endocem MTA Premixed exhibited similar push-out bond strength to ProRoot MTA (p > 0.05), perhaps due to the presence of DMSO, which increased the dentin wettability and provided sufficient opportunity for the hydraulic cement to interact with the root dentin.
Hydraulic bioceramic material is believed to be bioactive, forming hydroxyapatite crystals inside the dentinal tubules [20] in a process called biomineralization. Yoo et al. [21] reported intratubular biomineralization in root canals filled with bioceramic material after 8 years of clinical maintenance. Furthermore, this phenomenon can be promoted by treating the root canal with PBS in vitro [22]. To that end, we immersed the specimens in PBS for 30 days. In the present study, in both groups, small flake-shaped crystallized precipitates were observed along dentinal tubules up to around 300 μm. We also performed an EDS analysis to identify the chemical characteristics of the precipitates. According to the elemental analysis, the crystalline mass contained calcium and phosphorus at a mass percentage ratio of around 2:1, similar to the ratio found in hydroxyapatite. Yoo et al. [23] similarly found that the precipitates in their study had calcium/phosphorus ratios similar to hydroxyapatite and claimed that these may be favorable biomineralization patterns for the sealing of the root canal system. Reyes-Carmona et al. [24] also reported that the biomineralization induced by MTA enhanced the push-out strength of hydraulic cement. Leaving other issues aside, this study shows that Endocem MTA Premixed can induce biomineralization, and it suggests that further investigations are required on the effect of biomineralization in dentinal tubules on the bonding ability of hydraulic bioceramic materials.
CONCLUSIONS
This study showed that Endocem MTA Premixed, a newly developed premixed bioceramic root-end filling material, showed similar push-out bond strength to the widely used material ProRoot MTA. Consequently, the null hypothesis was accepted. Endocem MTA Premixed also exhibited biomineralization in dentinal tubules. Considering its ease of use and enhanced handling characteristics, Endocem MTA Premixed has potential for use as an acceptable root-end filling material for endodontic surgery.
Notes
Funding: This research was supported by a grant of the Korea Medical Device Development Fund grant funded by the Korea government (the Ministry of Science and ICT, the Ministry of Trade, Industry and Energy, the Ministry of Health & Welfare, Republic of Korea, the Ministry of Food and Drug Safety) (Project Number: RS-2020-KD000045).
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
Author Contributions:
Conceptualization: Park JH, Yu MK, Min KS.
Data curation: Park JH, Yu MK.
Formal analysis: Min KS.
Funding acquisition: Min KS.
Investigation: Park JH, Kim HJ.
Methodology: Park JH, Yu MK, Min KS.
Project administration: Yu MK, Min KS.
Resources: Yu MK, Min KS.
Software: Min KS.
Supervision: Lee KW.
Validation: Lee KW, Min KS.
Visualization: Park JH, Min KS.
Writing - original draft: Park JH, Min KS.
Writing - review & editing: Kim HJ, Lee KW, Yu MK.
