Comparison between a bulk-fill resin-based composite and three luting materials on the cementation of fiberglass-reinforced posts
Article information
Abstract
Objectives
This study verified the possibility of cementing fiberglass-reinforced posts using a flowable bulk-fill composite (BF), comparing its push-out bond strength and microhardness with these properties of 3 luting materials.
Materials and Methods
Sixty endodontically treated bovine roots were used. Posts were cemented using conventional dual-cured cement (CC); self-adhesive cement (SA); dual-cured composite (RC); and BF. Push-out bond strength (n = 10) and microhardness (n = 5) tests were performed after 1 week and 4 months of storage. Two-way repeated measures analysis of variance (ANOVA), 1-way ANOVA, t-test, and Tukey post-hoc tests were applied for the push-out bond strength and microhardness results; and Pearson correlation test was applied to verify the correlation between push-out bond strength and microhardness results (α = 0.05).
Results
BF presented higher push-out bond strength than CC and SA in the cervical third before aging (p < 0.01). No differences were found between push-out bond strength before and after aging for all the luting materials (p = 0.84). Regarding hardness, only SA presented higher values measured before than after aging (p < 0.01). RC and BF did not present 80% of the maximum hardness at the apical regions. A strong positive correlation was found between the luting materials' push-out bond strength and microhardness (p < 0.01, R2 = 0.7912).
Conclusions
The BF presented comparable or higher push-out bond strength and microhardness than the luting materials, which indicates that it could be used for cementing resin posts in situations where adequate light curing is possible.
INTRODUCTION
Endodontic treatments are usually associated with large dental tissue loss and the subsequent use of intra-radicular posts may be necessary to improve the retention of restorations to the tooth’s remnant [1]. Fiberglass-reinforced resin posts are preferable to posts with other compositions because of their higher flexural strength and elastic modulus, which are similar to those of dentin. Although it may generate higher maximum stress levels and a higher risk of fracture of the core and post, it results in lower stresses at the interface between cement and post and a lower risk of root fracture [2]. Esthetics is also an advantage of the fiberglass posts since they are translucent or opaque white, favoring the reproduction of the tooth’s remnant [3].
However, the adhesion of posts to root canals is a challenge due to high stresses at the adhesive interfaces caused by a high C-factor; the possibility of voids in the cement layer; and limited visualization and access to the root canal [456]. These difficulties may lead to the highly usual adhesive failure between the luting agent and tooth [7]. Also, the polymerization reaction of light-cured or dual-cured resin-based cements can be prejudiced by the reduced access of the light into the root canal. Inadequate polymerization leads to decreased mechanical properties of the luting material, which may result in adhesive failure of the post [8].
Bulk-fill resin-based composites have been introduced with the claim that they induce fewer stresses during their polymerization reaction and present a higher depth of cure when compared to conventional resin-based composites. These properties would enable filling cavities in a single portion of up to 5-mm depth. Studies suggest that the stresses induced by restorations are lower when using bulk-fill resin-based composites and these materials achieve a higher depth of cure than conventional resin-based composites [910].
The increased depth of cure would enable the adequate light curing of the bulk-fill resin-based composites inside the root canal, even in deeper areas where the access of light is limited, and the low induction of polymerization stress into restorations would reduce stresses in the adhesive interface reducing the risk of adhesive failures. Thus, low-viscosity bulk-fill resin-based composites could be an alternative material for the cementation of fiberglass-reinforced resin posts. Also, it would be possible to reduce the number of different materials that the dentist must have in their offices and make choices easier between a variety of materials. Flowable resin-based composites have been proposed as a luting material for veneers and other indirect restorations, but the viability of the cementation of posts using bulk-fill resin-based composites needs to be investigated [1112]. Therefore, this study aimed to evaluate the performance of 3 resin-based luting materials and 1 flowable bulk-fill resin-based composite when used on the cementation of fiberglass-reinforced resin posts, comparing their push-out bond strength and microhardness, before and after aging. The null hypothesis of this study was that there would be no difference between push-out bond strength and microhardness values achieved by the luting materials and the bulk-fill resin-based composite before and after aging, nor correlation between these properties.
MATERIALS AND METHODS
Sixty roots of bovine teeth with similar sizes and narrow root canals were selected for the present study, following the inclusion criteria: bovine incisors with root lengths of approximately 20 mm and root canals narrower than a #80 K-files; and the exclusion criteria: the presence of cracks or fractures or root canals wider than a #80 K-files. They were endodontically treated, using sodium hypochlorite irrigation, until reaching a diameter compatible with a #80 K-file and a working length of 1 mm far from the apex. Gutta-percha cones associated with the calcium hydroxide-based cement Sealer 26 (Dentsply Maillefer, Ballaigues, Switzerland) were used on the obturation of the root canals. The cold lateral compaction technique was used, with standardized a #80 K-file gutta-percha cones (Dentsply Maillefer) associated with accessory cones (Dentsply Maillefer). After obturation, the root canals were sealed with glass ionomer cement and stored in distilled water for 1 week. Then, the filling material was removed from the root canals with Largo burs (Dentsply Maillefer). Rebilda 20 drills (Voco, Cuxhaven, Germany) were used in the preparation of the canals for the fiberglass-reinforced post Rebilda Post 20 (Voco) cementation, 8 mm into the root canal, maintaining the remnant of filling material in the apex. The posts were cut to a 12-mm length and the root canals were rinsed with distilled water and dried with paper cones. Posts were cleaned with 70% alcohol and silanized with Ceramic Bond (Voco). The luting materials were used, according to the groups: 1) CC: Self-etching dual-cured adhesive system Futurabond DC (Voco) + Dual-cured resin-based cement Bifix QM (Voco); 2) SA: Self-adhesive dual-cured resin-based cement Bifix SE (Voco); 3) RC: Self-etching dual-cured adhesive system Futurabond DC + Dual-cured flowable resin-based composite Rebilda DC (Voco); and 4) BF: Self-etching dual-cured adhesive system Futurabond DC + Flowable bulk-fill resin-based composite X-tra Base (Voco).
Futurabond DC adhesive system was applied using a brushing motion for 20 seconds. The luting agents were applied with specific tips that allowed the injection of the material from the apical to the cervical third of the root. The light curing of the adhesive and luting materials was performed with the light curing unit Elipar Freelight 2 (3M ESPE, St. Paul, MN, USA) for 40 seconds, in contact with the coronary end of the post. The calculated radiant emittance of the light curing unit was approximately 700 mW/cm2 and the emission spectrum had its peak at 460 nm, measured with a fiber-optic spectrometer USB-2000 (Ocean Optics, Dunedin, FL, USA).
After storage in distilled water for 24 hours, the roots were embedded in Epofix epoxy resin (Strues, Ballerup, Denmark) using a dental surveyor, to ensure its orientation following the long axis of the posts. Roots were sectioned into 1 mm slices, with the aid of a cutting machine (Isomet 2000; Buehler, Lake Bluff, IL, USA) and separated by thirds of the root (cervical, middle, apical), 2 specimens per third, considering that the portion of the root that contains only gutta-percha was excluded.
Push-out bond strength test
Forty teeth were randomly selected for the push-out bond strength tests (n = 10). For each experimental group, 1 slice from each third of the roots was randomly selected to be tested after 1 week of storage in distilled water and the other slice was tested after 4 months of storage. The specimens were stored submerged in distilled water, which was changed weekly. Specimens had their thickness and diameter of the post measured at both sides of the slice with the aid of a digital caliper (Mitutoyo, Kawasaki, Japan). A universal testing machine Instron 5942 (Instron, Norwood, MA, USA) was used to perform the push-out bond strength tests. Specimens were positioned on a rigid base, with the smaller diameter of the tooth slice facing the actuator of the machine, which had exchangeable pins with different diameters that were changed to fit the diameter of the posts and maintain the applied forces at the adhesive interface.
The push-out test was performed at a crosshead speed of 0.5 mm/min until the dislocation of the post. Push-out bond strength of each specimen (MPa) was calculated as the ratio of the force (N) of failure and the adhesive area (mm2). The adhesive area was calculated by using the formula for the area of the frustum of a cone: A = π(R + r) √(R − r)2 + h2, where π is the constant 3.14, R is the larger radius, r the smaller radius, and h the thickness of the slice of the tooth.
After dislocation, specimens were evaluated regarding fracture pattern, through optical microscopy (40× magnification). The fractures were classified following the patterns: adhesive failure between dentin and cement; adhesive failure between post and cement; and mixed fracture.
Microhardness test
Twenty teeth were randomly selected for the microhardness test (n = 5). The slices from each tooth were embedded in epoxy resin. The embedded slices were ground flat and polished with a sequence of silicon carbide sandpaper with decreasing abrasiveness and diamond pastes associated with polishing cloths.
After polishing, specimens were stored for 1 week in distilled water until the first measurements using the microhardness tester HMV-2000 (Shimadzu, Tokyo, Japan). After 4 months of storage in distilled water, the hardness of the specimens was measured again. The specimens were stored submerged in distilled water, which was changed weekly. The microhardness tests were performed at the top surface of the slices, using a Knoop penetrator with a load of 100 gf for 30 seconds, and the readings were performed using the CAMS-WIN software (Shimadzu, Tokyo, Japan). At the luting material layer, 5 indentations were made per slice, with a 100-µm distance between them. The mean of the hardness values measured in the 2 slices of each third of the root was calculated. The ratio between the hardness values observed in each slice in depth (mm) and the highest hardness value achieved by each material, at the upper surface of the most cervical slice was also calculated as the percentage of maximum hardness.
Statistical analysis
Shapiro-Wilk tests were applied to verify the normality of data. Two-way repeated measures analysis of variance (ANOVA) followed by Tukey post-hoc multiple comparison tests were applied to the push-out bond strength data, considering luting material and third of the root; microhardness data, considering third of the root and aging for each luting agent separately; and reduction in hardness (%), considering results before and after aging separately. A t-test was applied to compare the push-out bond strength results before and after aging. One-way ANOVA and Tukey post-hoc tests were applied to compare the microhardness results of the different luting agents. χ2 tests were applied to verify the associations between the luting materials and the failure mode distribution. Pearson correlation test was applied to verify the correlation between push-out bond strength and microhardness results (α = 0.05).
RESULTS
The means and standard deviations for the push-out bond strength results are shown in Table 1. BF presented significantly higher push-out bond strength than CC and SA in the cervical third of the root before aging (p < 0.01). Considering the effect of aging on the push-out bond strength results, no significant differences were observed between bond strength measured before and after 4 months of water storage (p = 0.84). The failure mode patterns are shown in Figure 1. Mostly adhesive failures between teeth and luting materials were observed, with exception of BF, which presented more mixed failures, independent of the third of the root (p < 0.01).
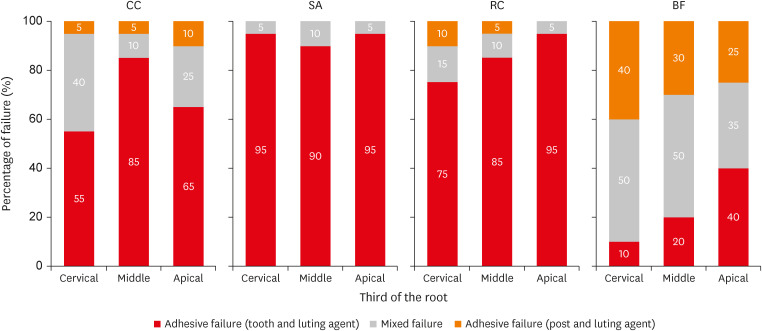
Percentage of failure according to its classification: Adhesive failure between tooth and luting material, mixed failure and adhesive failure between post and luting material.
CC, conventional dual-cured resin-based cement; SA, self-adhesive resin-based cement; RC, dual-cured resin-based composite; BF, bulk-fill resin-based composite.
The means and standard deviations for the microhardness results are shown in Table 2. Significant differences were found between microhardness values of the different thirds of the root (p < 0.01). The highest microhardness values were achieved in the cervical third, while the apical third presented lower hardness. Only the SA group presented significant differences between microhardness values measured before and after aging (p < 0.01). There were also significant differences in microhardness values of the different luting materials (p < 0.01). The percentage of the maximum hardness of the luting materials at the different depths is presented in Figure 2. After 1 week of storage, RC showed a percentage of maximum hardness below 80% (red area of the graph) at the 3 deeper slices, while the BF presented a percentage of maximum hardness below 80% at the deepest slice. The reduction in hardness (%) is presented in Table 3. RC and BF presented a higher reduction in hardness in the deeper slices after 1 week of storage, while SA presented the highest reduction in hardness after 4 months of water storage (p < 0.01). Pearson correlation test showed a strong positive linear correlation (total: p < 0.01, R2 = 0.7912; cervical: p < 0.01, R2 = 0.7765; middle: p < 0.01, R2 = 0.8504; apical: p < 0.01, R2 = 0.7456) between push-out bond strength and microhardness results measured before and after aging (Figure 3).
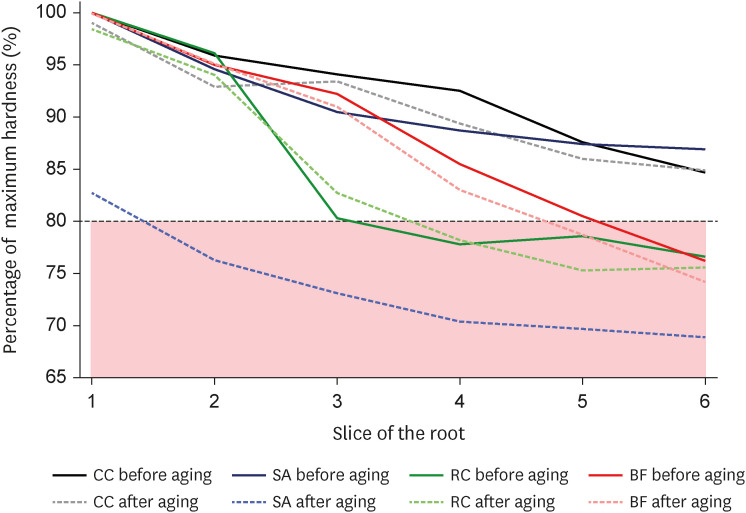
Maximum hardness ratio before and after aging. The area in which the hardness is below 80% of the maximum hardness is highlighted in red.
CC, conventional dual-cured resin-based cement; SA, self-adhesive resin-based cement; RC, dual-cured resin-based composite; BF, bulk-fill resin-based composite.
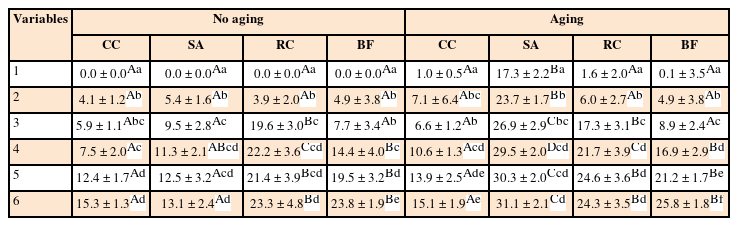
Reduction in hardness (%) means and standard deviations considering slice of the root and luting material
DISCUSSION
Push-out bond strength showed significantly higher results for BF compared to CC and SA in the cervical third of the root before aging; therefore, the null hypothesis was rejected. Three groups (CC, RC, and BF) had an adhesive system applied before the cementation of the post. A self-etch dual-cured adhesive system was used in this study because etching the inside of the root canal with posterior rinse and dry, with the maintenance of moist dentin, may present a high technique sensitivity, although feasible in a laboratory environment [13].
Although higher bond strength results were already reported when self-adhesive resin-based cements were used, the composition of these luting materials and, consequently, the bond strength results may vary [14]. A recent multicenter randomized double-blind clinical trial concluded that both self-adhesive and conventional resin-based cements obtained good survival rates and could be used for the cementation of fiberglass-reinforced resin posts [15]. In the present study, SA only presented lower push-out bond strength at the cervical third of the root when compared to BF and at the middle third of the root before aging, when compared to CC and BF. Therefore, the previous use of an adhesive system or the use of a self-adhesive resin-based cement may not justify the results.
Previous studies have reported lower polymerization stresses or lower cusps deflection when using bulk-fill resin-based composites, caused by modifications in their formulation [16]. Considering that the high c-factor and conical shape of root canals are determinants of the development of high stresses during the polymerization reaction, the use of luting materials that present lower stresses would result in higher bond strength [14]. Also, according to the manufacturer’s information, the luting agents used in this study have different filler contents. X-tra Base (BF) presents the highest filler content (75% by weight). Although there are no large differences between the filler content of the tested materials (Bifix QM [CC]: 70.2% w/w; Bifix SE [SA]: 68.6% w/w; Rebilda DC [RC]: 73.2% w/w), higher filler content should lead to less polymerization shrinkage and fewer stresses at the adhesive interface [17]. Although the filler content is not the only factor that determines the polymerization stresses, in the present study, the push-out bond strength results are in accordance with the percentage of filler by weight provided by the manufacturer, especially considering the cervical third of the root.
Different methods have been proposed for testing the bond strength of intra-radicular posts [1819]. The present study aimed to minimize issues regarding the sliding friction over the push-out bond strength test by using 1-mm thick root slices. Also, the punch pin was changed according to the post diameter in each slice to maintain the forces at the adhesive interface [20]. Regarding the failure pattern, the adhesive failure between the tooth and luting agent was the most common for the CC, SA and RC groups, reaching up to 95% of the failures in the SA group (Figure 1), which emphasizes the difficulty of adhesive procedure inside the root canal. Also, the higher prevalence of adhesive failures confirmed that the forces were maintained at the adhesive interface during the push-out tests.
Significant differences were observed between the hardness of the different tested materials; BF reached the highest hardness values, while SA achieved the lowest values (Table 2). Hardness values also decreased according to the increase of depth within the root, which can be seen by the slopes shown in Figure 2. Light transmission through the material is dependent on factors such as light scattering, surface reflection, and the absorption of light by the filler particles, photoinitiators, pigments and other components of the resin-based material [21]. When light-curing thick increments, a decrease in the light irradiance that reaches the bottom of restorations is expected, leading to lower polymerization in deeper regions of the root canal.
The hardness of the bottom of the restoration should achieve at least 80% of the maximum hardness of the material to be considered adequately polymerized [22]. CC and SA groups reached a minimum of 80% of the maximum hardness in the whole length of the root canal before aging. It was expected since both are dual-cured resin-based cements. However, even being a dual-cured resin-based composite, RC (green lines) presented 3 slices within the red area of the graph that represents a percentage of maximum hardness lower than 80% (Figure 2). Rebilda DC (RC) is a material used for the core build-up that can also be used for the luting of posts, and, to enhance the esthetic of restorations, it has higher opacity. While the other luting materials presented a translucent shade (CC and SA) and the bulk-fill resin-based composite presented a universal shade (BF), RC had an opaque dentin shade, and the higher opacity allows less light transmission through the restoration [23].
Although the bulk-fill resin-based composite (BF) did not achieve 80% of the maximum hardness at the deepest slice of the root, it reached approximately 76% of the maximum hardness. Considering the manufacturer's recommendation of portions with thicknesses of up to 4 mm, the depth of cure achieved in this study was about 6.2 mm, considering that about 0.3 mm of the slices were lost during the slicing procedure. Bulk-fill resin-based composites present higher translucency when compared to conventional resin-based composites, which may have allowed higher depths of cure [24]. Also, the use of a translucent fiberglass-reinforced post may have allowed the light transmission through the post, even knowing that the light transmission decreases in deeper regions of the root canal, it may have increased the reach of the light and, consequently, the depth of cure [25]. An increase in the exposure time and, consequently, an increase in the radiant exposure, may lead to better microhardness results, although more studies are necessary to guarantee that the achievement of an adequate polymerization at deeper regions of the root canal is possible [26].
Aging did not affect the push-out bond strength of the tested materials but affected the microhardness results. Four-month water storage was chosen as the aging method for this study based on previous studies that analyzed the bond strength after water storage [2728]. Also, the roots were sliced before the water storage and this is more aggressive than what happens in clinical conditions, where there is no exposition of the adhesive interface to water or saliva. The use of simplified self-etch adhesive systems should lead to the faster degradation of the adhesive layer, because of its hydrophilicity, and consequently, to the decrease in the bond strength, but it was not observed in the present study [29]. Longer water storage may be necessary to observe this decrease. Regarding hardness after aging, the SA group presented the highest decrease in hardness values (Figure 2). Self-adhesive resin-based cements have a more hydrophilic resin matrix when compared to resin-based composites. Also, the fillers of the self-adhesive cements are not coated with hydrophobic resin to allow them to react with the acidic monomers present in the resin matrix, leading to a less protected surface [30]. These formulation differences may have caused the greater degradation of the material observed in the hardness tests after aging.
Pearson correlation test showed a positive linear correlation between push-out bond strength and hardness values. Figure 3 shows that the scatter plot is homogeneous for results before aging, shown in blue, and after aging, shown in green. Hardness is associated with the degree of conversion and higher mechanical properties of the luting agent should lead to higher bond strength, avoiding fractures within the luting agent [31].
Although may be considered a limitation of the present study, the use of bovine teeth allowed better standardization of the size of the teeth and the root canal diameter. However, the light curing done in bovine teeth, performed in the laboratory, is more controlled than the light curing done in clinical situations. The reach of the light in posterior teeth, with the canals presenting some angle, may lead to inadequate polymerization of the bulk fill composites that are not dual-cured. Also, despite the fiberglass-reinforced resin post’s retention relies on the entire interface along the root canal, the bond strength was split by thirds of the root to allow the understanding of the adhesion in each segment of the posts, and the analysis of the correlation between bond strength and hardness of the luting materials.
More laboratory and longitudinal clinical studies need to be done to allow the indication of bulk-fill resin-based composites for the cementation of fiberglass-reinforced posts and the establishment of a light curing protocol to ensure the adequate polymerization of the material. However, considering the limitation of the present in vitro study, aiming to reduce the number of different materials that the dentist must have in their offices and to make choices between a variety of materials easier, bulk-fill resin-based composites should be considered in the cementation of fiberglass posts.
CONCLUSIONS
Although not the primary use of the flowable bulk-fill resin-based composites, it presented comparable or higher push-out bond strength and microhardness than the tested luting materials, which indicates it could be used on the cementation of fiberglass-reinforced resin posts in shallow preparations where the light curing can be properly done.
ACKNOWLEDGEMENTS
The authors thank Voco for the donation of the luting materials and posts used in this study.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
Author Contributions:
Conceptualization: Shimokawa CAK.
Data curation: Shimokawa CAK, Turbino ML.
Formal analysis: Shimokawa CAK, Turbino ML.
Investigation: Shimokawa CAK, Carneiro PMA, Lobo TRS.
Methodology: Shimokawa CAK, Carneiro PMA, Lobo TRS.
Project administration: Matos AB.
Resources: Shimokawa CAK.
Supervision: Matos AB.
Validation: Turbino ML, Braga RR, Matos AB.
Visualization: Turbino ML, Braga RR, Matos AB.
Writing - original draft: Shimokawa CAK.
Writing - review & editing: Turbino ML, Braga RR, Matos AB.






