Influence of the root canal filling technique on the success rate of primary endodontic treatments: a systematic review
Article information
Abstract
Objectives
This study aimed to investigate the influence of different obturation techniques compared to cold lateral compaction on the success rate of primary non-surgical endodontic treatments.
Materials and Methods
Systematic searches were performed for studies published up to May 17th, 2022 in MEDLINE/PubMed, Cochrane Library, Web of Science, Scopus, EMBASE, and Grey Literature Reports. Randomized clinical trials and nonrandomized (nonrandomized clinical trials, prospective or retrospective) studies that evaluated the success rate of primary non-surgical endodontic treatments obturated with the cold lateral compaction (control) and other obturation techniques were included. The revised Cochrane risk of bias tools for randomized trials (RoB 2) and nonrandomized studies of interventions (ROBINS-I) were used to evaluate the risk of bias. The Grading of Recommendations Assessment, Development, and Evaluation (GRADE) tool was used to evaluate the certainty of evidence.
Results
Eleven studies (4 randomized clinical trials (RCTs), 4 prospective, and 3 retrospectives) were included. Two RCTs were classified as having some concerns risk of bias and 2 as a low risk of bias. Two nonrandomized studies were classified as having a critical risk of bias and 5 as having a moderate risk of bias. The GRADE analysis demonstrated a very low to moderate certainty of evidence.
Conclusions
This systematic review generally evidenced no differences in the success rate of primary non-surgical endodontic treatments when the cold lateral compaction technique and other obturation techniques are performed. Further well-designed studies are still necessary.
INTRODUCTION
Root canal filling aims to prevent communication between the root canal and the oral cavity or periapical tissues. It also aims to prevent residual microorganisms from having access to nutrients that allow them to proliferate and, thus, maintain or develop a periapical lesion [1]. For this, a tridimensional sealing of the root canal system is necessary. Canal irregularities such as isthmus, lateral and secondary canals, and accessory foramina are often present, and the presence of microorganisms or their by-products in these areas can impact the success of the endodontic treatment [234]. It has been reported that failure in endodontic treatments is associated with the low quality of root canal fillings [56]. These findings suggest the importance of root canal filling on the outcome of the endodontic treatment.
Several techniques have been proposed and advocated to achieve great filling of the root canal system. Cold lateral compaction (CLC) is the most common obturation technique and, for scientific purposes, is considered the technique against which all other techniques should be compared. It consists of selecting a master gutta-percha (GP) cone, usually corresponding to the last instrument that reached the working length (WL), that should fit in the apical space created after instrumentation with a slight resistance to traction. The canal walls and the master GP cone are coated with the endodontic sealer, and the master GP cone is positioned in the WL. The master GP cone is laterally compressed with finger spreaders to create spaces for the insertion of accessory GP cones until the canal is filled. The advantages of CLC are that this technique is of relatively low cost, easy to perform, and allows the control of the filling length [7]. However, micro-computed tomography studies have shown larger volumes of gaps and voids after CLC mainly if a poor preparation was performed, inadequate pressure is applied to the spreaders, or if there is a mismatch of tapers between spreaders or GP cone and the canal walls [89101112131415].
For these reasons, warm vertical compaction (WVC) techniques were developed [16]. Nowadays, WVC of GP is performed with heat generators for down-packing and an injectable GP device for backfilling. In this technique, the master GP cone should be coated with the sealer and positioned in the WL. Then, a heated tip is introduced into the canal until 4–5 mm from the WL, cutting the master GP cone. Backfilling is performed by inserting plasticized GP, and an apical pressure is maintained without heat until the GP is cooled [17].
Another technique, the carrier-based technique consists of a flexible plastic core carrier that is homogeneously coated with a layer of refined alpha-phase GP. The canal space is first checked with a “verifier,” then, a corresponding preheated carrier obturator is inserted with firm apical pressure until the WL. In WVC and carrier-based techniques, the GP becomes plasticized because of the heat applied to the material, allowing the GP to present better adaptation to irregularities and recesses, especially in oval-cross section canals [18]. However, techniques that involve the use of plasticized GP also have disadvantages. When GP is heated, it expands. During cooling, it presents a contraction of 1 to 2%, which may result in voids and gaps along with the root filling [19].
Finally, the single cone technique became popular with the increased use of rotary and reciprocating instruments for canal preparation. This technique uses matched GP cones with tip and taper corresponding to the last instrument used in the WL. The advantages include low cost, straightforward execution, and short working time. However, the presence of voids and gaps in cases of flattened or oval-cross section canals and the setting contraction of some endodontic sealers are the main drawbacks of this technique [20].
There are few previous systematic reviews on the subject [1921]. One did not find any difference between obturation techniques and materials used for root canal filling on the treatment outcome [21]. However, this systematic review only included teeth presenting apical periodontitis. And another, only compared long-term outcomes and obturation quality between WVC and CLC [19]. Therefore, it is not possible to determine if these results are applicable to vital teeth or when evaluating obturation techniques other than those previously reported.
Mainly because of these drawbacks, the present systematic review investigates the available evidence regarding the influence of the root filling technique on the success rate of primary endodontic treatments. In this systematic review, the CLC technique was considered as the comparison group, since it is commonly used by dentists, due to its simple execution, low cost, predictability, and controlled placement of GP cones [22]. Therefore, this systematic review aimed to answer the following question: “What is the impact of different obturation techniques compared to the CLC technique on the success rate of primary non-surgical endodontic treatment?”
MATERIALS AND METHODS
The present systematic review followed the recommendations of the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) [23] and was recorded in the PROSPERO database under number (CRD42021247855).
Search strategy
The following electronic databases were searched by two independent examiners (D.F.M. and G.S.S.): MEDLINE/PubMed, Cochrane Library, Web of Science, Scopus, EMBASE, and Grey Literature Reports. Searches were conducted from inception up to May 17th, 2022, with all searches starting and ending on May 17th, 2022. No restrictions for language or year of publication were applied. The descriptors most frequently cited in previous publications on the subject have been used for electronic research. The following Medical Subject Heading (MeSH) terms and text words (tw.) were combined in each database for search: “Root canal obturation,” “Obturation technique,” “Root canal filling material,” “Endodontic obturation,” “Cold lateral compaction,” “Cold lateral condensation,” “Lateral compaction technique,” “Lateral condensation technique,” “Lateral condensation,” “Lateral compaction,” “Periapical healing,” “Apical healing,” “Periapical repair,” “Success rate,” “Prognosis,” “Prognostic factors,” “Treatment outcome,” “Clinical effectiveness,” “Treatment effectiveness,” “Treatment efficacy,” “Clinical efficacy,” “Outcome assessment,” “Assessment outcomes,” “Outcomes assessment,” “Outcome measures,” “Outcome predictors,” “Clinical outcome.” Boolean operators ‘AND’ and ‘OR’ were used to combine terms and create a search strategy (Supplementary Table 1). A manual search on the references of the included studies was performed, and the related studies were selected from the PubMed database. All the selected studies were imported into the Mendeley (Mendeley Ltd., London, UK) reference manager to catalog the references and facilitate the exclusion of duplicates.
Eligibility criteria
Eligibility criteria were based on the PICOS strategy, as follows [242526]:
• Population (P) – adult patients undergoing primary non-surgical endodontic treatment;
• Intervention (I) – different obturation techniques;
• Comparison (C) – cold lateral compaction technique;
• Outcome (O) – clinical and radiographic success rate;
• Study design (S) – randomized clinical trials, nonrandomized clinical trials, and longitudinal (prospective and retrospective) studies.
Studies that evaluated the success rate of endodontic retreatment, endodontic treatment in primary or immature teeth, or used reparative materials (i.e., mineral trioxide aggregate) for canal obturation were excluded.
Selection of the studies
The selection of studies was done by two independent authors (D.F.M and G.S.S.). First, duplicate studies were excluded, and the title and abstract of studies were screened. When it was impossible to judge only by title and abstract, the full text was assessed and read for the final decision. The next step was to read the full text of the potentially eligible articles according to the eligibility criteria of the PICOS strategy. If there was disagreement, a consensus was reached by a third author (T.W.).
1. Data extraction
Two independent reviewers performed the data extraction (D.F.M and G.S.S.). In case of disagreements, a consensus was reached by a third author (T.W.). The extracted data were: author’s name(s), year of publication, study design, number of teeth evaluated per group, type of teeth, diagnosis, preparation technique, number of visits, obturation technique, follow-up time, parameters evaluated to determine success, and main findings. In cases of missing data, the authors were contacted three times by email within one week.
2. Risk of bias analysis
The risk of bias was independently evaluated by two authors (D.F.M. and G.S.S.). In case of disagreement, a third author was responsible for the final decision (T.W.).
For randomized controlled studies, studies were assessed by using the Cochrane risk of bias for randomized controlled trials (RoB 2) tool: ‘Risk Assessment of Bias of Randomized Controlled Trials’ - Cochrane Handbook 6.0 [27]. The following domains were considered: randomization process; deviations from intended interventions; missing outcome data; measurement of the outcome; selection of the reported results.
The blinding of operators was not considered since it is impossible to perform this type of intervention. However, blinding of evaluators was considered during the assessment of the risk of bias. Each included study was judged as having a “high” risk of bias for negative domain responses (red), a “low” risk of bias for positive domain responses (green), and a “some concerns” risk of bias (yellow) when the response was not it was clear. When the study was judged as ‘some concerns; authors of the study were contacted by email at least three times to obtain further information that would allow them to classify them as ‘low’ (green) or ‘high’ (red) risk of bias. When this information was not acquired, the articles were classified as having some “some concerns” risk of bias. Overall quality was based on scores within individual domains. When a low risk of bias was found for all domains, the overall quality was a low risk of bias. When at least one domain was of some concerns risk, the overall quality was of some concerns risk of bias. In addition, rating at least one domain as high risk or three or more domains as some concerns risk resulted in overall quality of high risk of bias.
The Risk of Bias in nonrandomized Studies of Interventions (ROBINS- I) tool was used to analyze both nonrandomized clinical trials and longitudinal studies (prospective and retrospective) [28]. The following domains were assessed:
1) Confounding factors: ‘Low’ risk of bias was considered when all possible confounding factors were checked in the design or the statistical analysis. ‘Moderate’ risk of bias when some possible confounding factors were controlled. ‘Serious’ risk of bias when no possible confounding factors were controlled. ‘Critical’ risk of bias when possible confounding factors were not even discussed.
2) Selection of participants: ‘Low’ risk of bias was considered when all eligible participants were included in the study. ‘Moderate’ risk of bias when the participant selection may have been related to intervention/outcome. ‘Serious’ risk of bias when participant selection was related to intervention/outcome. ‘Critical’ risk of bias when the selection process was not described.
3) Classification of interventions: ‘Low’ risk of bias was considered when the chemo-mechanical preparation and obturation techniques were well described. ‘Moderate’ risk of bias when the chemo-mechanical preparation and obturation techniques presented some missing information, but the missing data were not relevant to the purpose of the included study. ‘Serious’ risk of bias when the chemo-mechanical preparation and obturation techniques were not well described. ‘Critical’ risk of bias when the chemo-mechanical preparation and obturation techniques were not described.
4) Deviations from intended interventions: ‘Low’ risk of bias was considered when no differences occurred after the beginning of the study, or differences in one or both groups occurred after the beginning of the study, but the participant continued (for analysis purposes) to be part of the study. ‘Moderate’ risk of bias when differences occurred after the beginning of the study, but it does not seem to affect its outcome. ‘Serious’ risk of bias when few differences occurred after the beginning of the study and changes in the sample or intervention were required. ‘Critical’ risk of bias when several differences occurred after the beginning of the study.
5) Missing data: ‘Low’ risk of bias was considered when the number of teeth evaluated per group, type of teeth, preparation technique, number of visits, obturation technique, follow-up time, and parameters evaluated to determine success were well reported. ‘Moderate’ risk of bias when there were some missing data, but the missing data were not relevant to the purpose of the included study. ‘Serious’ risk of bias when there were some relevant missing data. ‘Critical’ risk of bias when there were several relevant missing data
6) Measurement of outcomes: ‘Low’ risk of bias was considered when valid parameters (clinical and radiographic) were used to determine success. ‘Moderate’ risk of bias when using a valid methodology, but the methodology was not well described. ‘Serious’ risk of bias when a valid methodology was not used, but the methodology was well described. ‘Critical’ risk of bias when a valid methodology was not used, not well described, or the methodology used was not described.
7) Selection of described results: ‘Low’ risk of bias was considered when all results were presented. ‘Moderate’ risk of bias when results were reported but not well described. ‘Serious’ risk of bias when there was a substantial difference in the description of the results of each intervention. ‘Critical’ risk of bias when information is not presented.
Each domain was registered as low, moderate, serious, critical, or with no information available to address the risk of bias. The overall risk of biased judgment was determined by combining the bias levels in each domain. The low overall risk of bias was considered when all domains were considered to be at low risk of bias; overall moderate risk of bias was considered when at least one domain was considered to have moderate bias; overall serious risk of bias was considered when at least one domain was considered to be severely biased, and the overall critical risk of bias was considered when at least one domain was considered to be at critical risk of bias.
3. Certainty of evidence
Certainty of evidence of the included studies was assessed through the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) tool. The following domains were independently assessed by the reviewers following the GRADE guidelines: risk of bias; inconsistencies; indirectness; imprecision; and other considerations - assessment of publication bias, significant effect, plausible confounding, and dose-response gradient [29].
RESULTS
Study selection
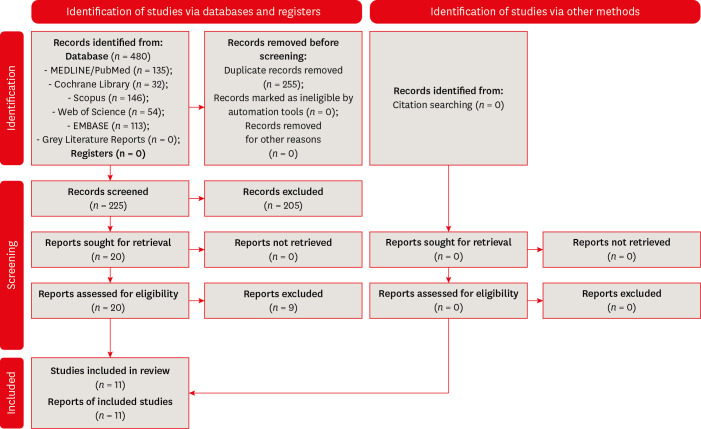
Figure 1 displays the flowchart of the search strategy. Initial screening of databases resulted in 480 studies. Of these, 255 were excluded because of being duplicates. From the analysis of the titles and abstracts of 225 eligible articles, 20 studies were selected for full-text reading [3031323334353637383940414243444546474849]. Of these, nine studies were excluded. Four studies due to sample overlap (data used in more than one study); 2 studies for not having assessed periapical healing; 1 study for not having an experimental group; 1 study for including data on retreatments; and 1 study for not having evaluated obturation techniques [313233364041434649]. Finally, 11 studies were included in the current systematic review [3034353738394244454748].
Data extraction
The characteristics and main results of the included studies are presented in Table 1. Authors of studies that lacked information were contacted 3 times by email. No further information was obtained. In addition to the lateral cold compaction technique, 3 studies investigated the success rates of the WVC techniques [353747]. Six studies evaluated carrier-based obturation techniques; 2 studies investigated the single-cone techniques; and 1 study also investigated the use of silver/titanium cones, or the use of Endomethasone (Septodont, Saint Maur Des Fosses, France) sealer alone, compared to the CLC [303437383942444548].
When considering the follow-up periods, one study performed a follow-up of only 2 months [47]. In 2 studies, the follow-up period was one year [3948]. Two other studies had a follow-up ranging from 1.5–3 years [4245]. One study performed a follow-up of 2 years; 3 studies presented a follow-up of 3–4 years; 1 study performed the follow-up for a period ranging from 4–6 years; and finally, 1 study reported a follow-up of 5 years [303435373844].
Regarding the parameters adopted to determine the success of the endodontic treatments, the absence of clinical symptoms (pain, sensitivity to percussion or palpation, mobility) and absence of radiographic evidence of pathology were the most frequently adopted parameters [3034353738394244454748]. Three studies used the periapical index (PAI) as a tool to assess periapical healing and 1 study considered the Strindberg and PAI criteria [35374448].
Regardless of the diagnosis, most studies indicated no difference in the success rate of endodontic treatments performed by the CLC technique compared to the other evaluated techniques [3435383942444548]. Only 2 studies reported higher success rates for teeth obturated with the WVC technique; and 1 study reported for better results when CLC was used compared to the single-cone technique, silver/titanium cones, or Endomethasone sealer used alone [303747]. Additionally, one study reported higher success rates for the WVC in teeth presenting radiographically visible periapical lesions [35].
Quality assessment
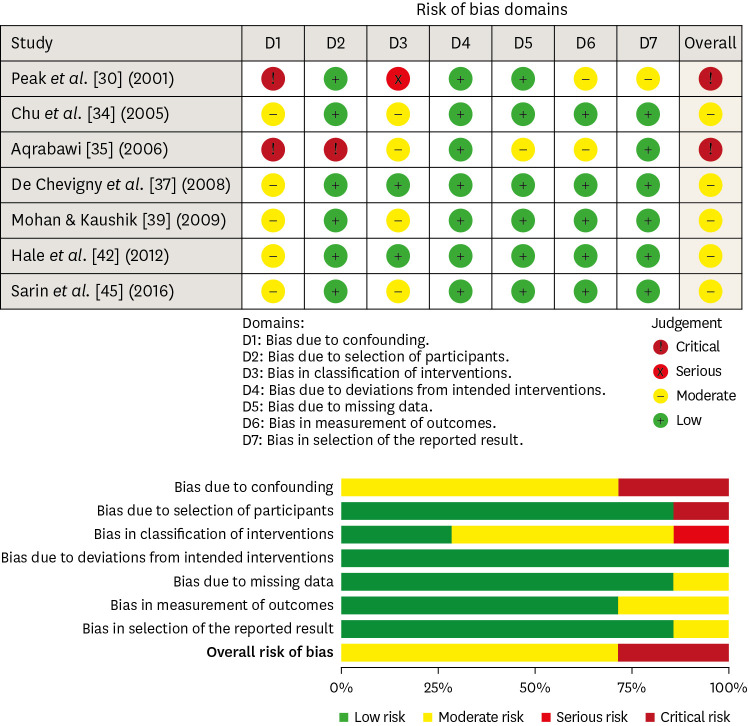
Figure 2 displays the risk of bias assessment of the randomized controlled trials [50]. Among the four randomized clinical trials included, 2 were classified as having a ‘low’ risk of bias, and 2 studies as having ‘some concerns’ risk of bias, mainly due to presenting some concerns in the domain bias arising from the randomization process [38444748].
Quality assessment of the randomized clinical trials, according to the Cochrane Collaboration standard scheme for bias and RoB2 tool.
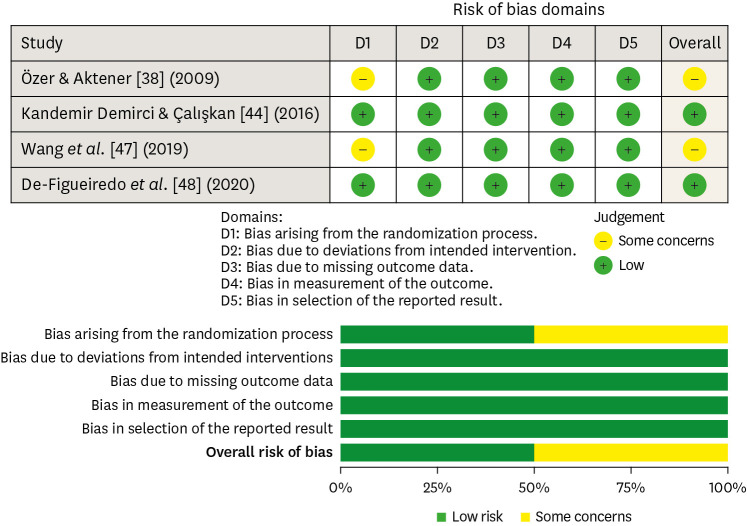
Figure 3 displays the risk of bias assessment of the nonrandomized controlled trials and longitudinal studies [50]. Two studies were classified as having a ‘critical’ risk of bias, while the others were classified as having a ‘moderate’ risk of bias [3035]. In the domain of bias due to confounding factors, 2 studies had a critical risk of bias, and 5 had a moderate risk of bias [30343537394245]. In the domain of bias due to the selection of participants, 1 study had a critical risk of bias, and the others had a low risk of bias [35]. In the domain of bias in the classification of interventions, 1 study had a serious risk of bias; 4 studies had a moderate risk of bias, and the other studies had a low risk of bias [3034353945]. In the domain of bias due to deviations from intended interventions, all studies had a low risk of bias. Only 1 study had a moderate risk of bias in the domain bias due to missing data [35]. Additionally, 2 studies had a moderate risk of bias in the domain bias in the measurement of outcomes [3035]. And finally, 1 study had a moderate risk of bias in the domain bias in the selection of reported results [30].
Strength of evidence
A summary of the results of the GRADE evaluation is presented in Table 2. The GRADE tool demonstrated a moderate to very low certainty of the evidence for the included studies. The randomized clinical trials received the ‘serious’ classification for risk of bias; the ‘not serious’ classification for inconsistency, indirectness, and imprecision; and no other considerations. The nonrandomized studies received the ‘very serious’ classification for risk of bias; the ‘serious’ classification for inconsistency; the ‘not serious’ classification for indirectness and imprecision; and the ‘strong association’ in other considerations.
DISCUSSION
Several obturation techniques have been proposed to fill the root canal system, aiming to eliminate, as much as possible, the presence of voids and gaps [3]. Since a root canal filling of low quality is associated with worst outcomes in primary endodontic treatments, it is necessary to investigate whether one obturation technique can favor better clinical outcomes over the other [5].
Through the data extracted from the included studies, eight out of eleven studies did not find any difference in the clinical and radiographic success rate between CLC and the other tested techniques [3435383942444548]. Therefore, it can be suggested that the disinfection of the root canal system, considering the apical limit of instrumentation and a sufficient degree of canal enlargement, the use of auxiliary chemical substances in adequate concentrations to allow the dissolution of microorganisms and organic tissue content, and, when necessary, the use of root canal dressing, allowing the reduction of the microbial content, is more important than the obturation technique itself [5152].
Controversially, 2 studies observed that the vertical compaction technique presented superior results when compared to the CLC technique [3747]. Wang et al. [47] observed a success rate of 98% for teeth filled with WVC and 71% for teeth filled with CLC. However, these conclusions are based on a short period of clinical and radiographic follow-up (2 months), which is insufficient to determine the treatment’s outcome. The American Association of Endodontists [53] suggests that the follow-up period be performed until the lamina dura is restored. The European Society of Endodontology [54] recommends that the follow-up period be performed until the complete repair of the periapical tissues, which can take up to 4 years. Only 2 studies included in this systematic review performed a follow-up of 4 years or more [3537]. Aqrabawi [35], comparing the CLC and the WVC, reported a success rate of 79% and 82%, respectively. Although a significant difference was not observed in these results, it was observed a significant difference in teeth presenting radiographically visible periapical lesions, favoring a better outcome for the WVC.
It is important to emphasize that the study by Chevigny et al. [37] had the most significant sample investigated (number of teeth: 1952). Additionally, Chevigny et al. [37] reported 87% and 77% success rates for teeth obturated with the WVC and lateral compaction techniques, respectively. Since this study is a cohort that encompasses previous studies, only the pooled sample size was considered for purposes of data analysis [313336].
Only one study found better clinical and radiographic outcomes for the lateral compaction technique [30]. In this study, the authors compared the lateral compaction to the single-cone technique and reported a 92% and 68% success rate, respectively. In this study, the lower success rate on teeth filled with the single-cone technique can be explained by the use of an endodontic sealer based on zinc oxide and eugenol (Endomethasone), which presents lower-dimensional stability [55]. This feature favors a higher sealer contraction after setting and the occurrence of more gaps and voids. It is known that the single-cone technique, depending on the root canal anatomy, generates a thicker sealer layer around the main GP cone. Therefore, when performing this technique, the use of endodontic sealers with good physicochemical properties, especially dimensional stability and flow, is essential for the adequate filling of the root canal system.
The included studies evaluated anterior and posterior and lower and upper teeth. It is important to emphasize that the internal morphology of posterior teeth is more complex than those presented by anterior teeth [3]. For this reason, it is reported that the success rates for posterior teeth can be lower compared to anterior teeth, ranging from 80% to 90% [304245]. The evaluated studies also included different pulpal and periapical statuses. Some selected only cases with periapical pathologies, while others did not consider this variable for the inclusion criteria [444748]. The presence of periapical pathologies is a critical factor that can influence the success rate of the endodontic treatment [5657]. Therefore, the results of obturation techniques in teeth with and without periapical pathologies should be carefully analyzed.
The absence of clinical and radiographic signs and symptoms has been used to evaluate the endodontic treatment outcome [58]. The most used radiographic criteria were the Periapical Index (PAI). Regarding the Periapical Index, it radiographically classifies endodontic success into 5 levels – PAI 1: Normal appearance, without bone alterations; PAI 2: Minor changes, possibly without bone destruction; PAI 3: Change in the visible bone structure; PAI 4: Presence of periradicular lesion with well-defined bone resorption; PAI 5: Severe periradicular lesion with signs of expansion [59]. Additionally, Strindberg’s criteria were used in one study [35]. Strindberg’s criteria determine the clinical success of the treatment through the presence or absence of symptoms and radiographically by evaluating the periodontal contour and the integrity of the lamina dura [60]. Despite the differences in the methodologies adopted by some included studies, these criteria seem to be similar in terms of parameters evaluated to determine success, allowing a comparison between studies.
Another critical factor is the differences in the chemo-mechanical preparation. Several systems were used for mechanical preparation in the included studies. Also, despite sodium hypochlorite (NaOCl) being the chemical substance used in all studies, its concentration ranged from 1% to 5%. It has been shown that the concentration of NaOCl does not appear to influence the reduction of the microbial load of the root canal system [6162], but the volume of irrigant solution, the frequency of irrigant renewal, and the time that it remains inside the root canal are factors that play an essential role during treatment [6364]. However, the included studies did not describe these aspects.
Another significant limitation is the lack of data regarding the number of visits and use of intracanal medications. The influence of intracanal medications, such as calcium hydroxide, was not accessed by any of the included studies. However, it has already been shown that the outcome of treatments performed in single- or multiple-visits is similar [65]. The investigated sealers also varied. Despite the results presented by one study, the different sealers do not seem to have influenced the outcomes investigated in most studies [30].
Regarding the risk of bias assessment of the randomized clinical trials, 2 studies had some risks in the randomization process because the authors did not describe the randomization method and if the allocation sequence was concealed [3847]. The other domains were of low risk of bias for all studies. As for the risk of bias in nonrandomized studies, 5 studies had a moderate risk due to confounding factors, and 2 had a critical risk [303435394245]. The presence of a confounding factor can result in a mixture of effects. The effects of the intervention on a given outcome are mixed with the effects of an additional factor, resulting in a distortion of a genuine cause-and-effect relationship [66]. Bias in the selection of participants occurs when some eligible participants, or the follow-up time of some participants, are excluded in a way that leads to an association between intervention and outcome different from the association that would have been observed under other circumstances [28]. In this domain, only 1 study had a critical risk [35].
When intervention status is incorrectly classified or not sufficiently detailed, it can result in bias in the classification of interventions [28]. For these reasons, in this domain, 4 studies had a moderate risk of partially presenting information about the chemo-mechanical preparation and obturation technique [34353945]. One study had a serious risk for not presenting crucial information about the chemo-mechanical preparation and obturation technique [32].
In the bias due to deviations from intended interventions, all studies had a low risk of bias. One study had a moderate risk of bias due to missing data for not presenting information on the group of teeth evaluated and the number of visits during treatments [35]. In the bias in outcome measurement, 2 studies had a moderate risk for not presenting sufficient information on the methodology adopted to evaluate treatments’ success [3035]. Finally, 1 study had a moderate risk of bias in selecting the reported results for not reporting all the investigated outcomes [30].
Due to these limitations, the overall certainty of evidence classified using the GRADE tool was very low to moderate. In the domain of risk of bias, the randomized clinical trials received the ‘serious’ classification because 2 studies presented concerns regarding the randomization process [384767]. The nonrandomized studies received the ‘very serious’ classification, because 5 studies did not control for all possible confounding factors, and 2 studies did not control for confounding factors at all [30343537394245]. In the domain inconsistency, the randomized clinical trials received the ‘not serious’ classification; and the nonrandomized studies the ‘serious’ classification because some heterogeneity was verified, including differences in populations and interventions [68]. In the domain of indirectness, the randomized clinical trials and the nonrandomized studies received the ‘not serious’ classification [69]. The domain imprecision was accessed following the recommendations of since a meta-analysis was not feasible in the present systematic review [70]. The recommendations from Murad et al. [70] are to consider the total number of participants (i.e., pooled sample size) of the included studies and the confidence interval (CI) of the most extensive studies. A pooled sample size of fewer than 400 concerns imprecision, and results may be imprecise when the CIs of the largest studies include no effect and meaningful benefits or harms [70]. Therefore, the domain imprecision was considered ‘not serious’ for randomized and nonrandomized studies since their pooled sample size was more significant than 400, and the 95% CI of the studies with the most expansive sample sizes included meaningful effects of the investigated outcomes [70]. The domain 'other considerations' included the assessment of publication bias, large effect, plausible confounding, and dose-response gradient, which can upgrade the overall certainty of evidence [71]. For both randomized and nonrandomized studies, none were verified, and, therefore, the certainty of the evidence was not upgraded.
This systematic review presents some strengths. It was performed based on a protocol registered a priori, and only included studies of high level of evidence (randomized and non-randomized clinical trials, and longitudinal clinical studies) in order to provide a level I evidence on the investigate topic [72]. Based on the presented results, it is possible to suggest that the choice of one specific obturation technique over another does not present a significant impact in the treatments outcomes. However, meta-analyses were not possible to be performed due to a high heterogeneity among studies. Therefore, external validity and generalization of results should be cautiously interpreted, since it was not possible to quantitively analyze the available data and to accurately determine if the different obturation techniques were really not statistical different.
Further clinical studies should perform a solid randomization process and describe the randomization method and allocation sequence. Authors must control all possible confounding factors and standardize their interventions, especially regarding the group of teeth, chemo-mechanical preparation, number of visits, obturation techniques, and the evaluated parameters to determine success. Additionally, longer follow-up periods must be adopted to determine success.
CONCLUSION
Based on the results of the present systematic review, it is possible to infer that the investigated obturation techniques does not impact on the treatment’s outcome. However, further well-designed studies are necessary to confirm the trends of this review.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
Author Contributions:
Conceptualization: Marconi DF, Weissheimer T, da Rosa RA.
Data Curation: Marconi DF, da Silva GS, Weissheimer T.
Formal Analysis: Marconi DF, da Silva GS, Weissheimer T.
Investigation: Marconi DF, da Silva GS.
Methodology: Weissheimer T, Skupien JA, Só MVR, da Rosa RA.
Project administration: Weissheimer T, Skupien JA, Só MVR, da Rosa RA.
Supervision: Skupien JA, Só MVR, da Rosa RA.
Writing - original draft: Marconi DF, da Silva GS, Weissheimer T.
Writing - review & editing: Jahnke LT, Silva IS, Só GB, Skupien JA, da Rosa RA.
References
SUPPLEMENTARY MATERIAL
Supplementary Table 1
Search strategy in each database